Abstract
The appearance of a crust initially suggests inflammatory scalp diseases, although infectious diseases such as impetigo or insect bites should also be considered among the differential diagnoses. We report a case of 40-year-old woman presented to our Hair Disease Outpatient Service with an adherent serous crust on the scalp and lymphadenopathy of the neck. Serological tests confirmed the aetiology of B. Burgdorferi, while rickettsia infection was excluded. Lyme borreliosis can mimic rickettsia infection and may present as scalp eschar and neck lymphadenopathy after a tick bite (SENLAT). Appropriate tests should be included in the diagnostic workup of patients with necrotic scalp eschar in order to promptly set up targeted therapy also if only the scalp is involved.
Keywords: Borrelia Burgdorferi; Lyme Disease; SENLAT; Eschar; Scalp Eschar and Neck Lymphadenopathy
Abbreviations: SENLAT: Scalp Eschar and Neck Lymphadenopathy after a Tick Bite; EPDS: Erosive Pustular Dermatosis of the Scalp; APS: Amicrobial Pustulosis of the Scalp; DEBONEL: Dermacentor-Borne Necrosis Erythema and Lymphadenopathy; EM: Erythema Migrans
Introduction
Scalp eschar and neck lymphadenopathy after tick bite (SENLAT) is an emerging and increasingly common syndrome, primarily described in Europe. Clinically, it is characterized by the presence of a scalp eschar associated with an enlargement of the occipital and/or cervical lymph nodes after a tick bite. This may be accompanied by systemic symptoms such as rash, fever and malaise. Often the eschar results in a form of permanent scarring alopecia. The syndrome was initially associated with several rickettsial genotypes, nowadays other causative agents such as Bartonella henselae, Coxiella spp, Borrelia burgdorferi and Francisella tularensis are described. The scalp as a site of infection is a rarely reported. We report a case of a 40-year-old woman who presented to our Hair Disease Outpatient Service with an adherent serous crust on the scalp, which turned out to be a necrotic eschar from a tick bite.
Case Presentation
A 40-year-old woman presented to our Hair Disease Outpatient Service with an adherent serous crust on the occipital site of the scalp. On clinical examination she presented with a serous haematic crust adhering to the scalp since about 10 days, associated with general malaise, fatigue, muscle pain, fever (37.3 °C) and laterocervical lymphadenopathy. The crusty lesion measuring 2 cm in diameter was removed with saline and hydrogen peroxide and a necrotic eschar was detected (Figure 1). The clinical presentation initially suggested a diagnosis of an inflammatory hair diseases such as an initial phase of erosive pustular dermatosis of the scalp (EPDS) or an infectious dermatosis such as impetigo. An insect bite was also investigated and in fact the patient brought photographic material showing a picture of the tick attached to the scalp.
In view of this finding, the clinical presentation and history of tick exposure suggested a rickettsia infection diagnosis. Because a certain diagnosis of Lyme disease could not be ruled out, systemic therapy with Doxycycline100mg twice daily for 14 days was administered, with a rapid improvement of the symptoms. The necrotic eschar was treated with Inadine® gauze with a good clinical result. Three weeks after the start of antibiotic, serological tests for the respective tick-borne pathogens was performed and high concentrations of antibodies against B. burgdorferi s.l.: IgG 44 U/mL (positive cut-off >22 U/mL) and IgM 270 U/mL (positive cut-off >22 U/mL), also confirmed by immunoblot, was detected. Antibody levels against Rickettsia spp. were indeed negative.
Discussion
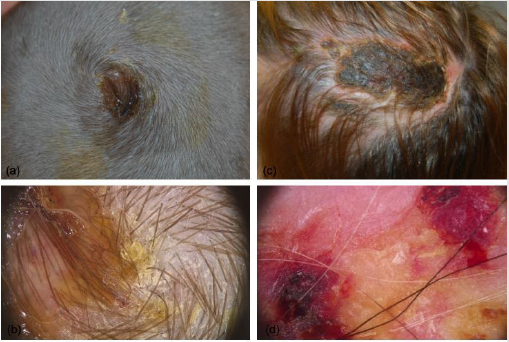
The appearance of a crust on the scalp initially suggests an inflammatory hair disease such as an early stage of EPDS, infectious diseases such as impetigo or insect bites should also be considered among the main differential diagnoses (Figure 2). EPDS, also known as amicrobial pustulosis of the scalp (APS), was first described in 1979 by Pye, et al. as a rare inflammatory entity with a chronic course usually affected the elderly age. The clinical presentation varies according to the clinical stage: solitary or multiple areas, sometimes coalescent, superficial erosions, sterile pustules and brownish-yellow crust with serum-haematic exudate are the clinical features of EPDS in the early stages; these lesions may develop into diffuse atrophy and patches of cicatricial alopecia in the later phases, slowly involving adjacent areas of the scalp [1]. Bacterial folliculitis, also known as impetigo, is an infectious disorder of the scalp, mostly shown in childhood, frequently caused by Staphylococcus aureus or Streptococcus pyogenes. Clinically it manifests as tufted hair emerging together from a yellow-white pustule with an erythematous border.
Figure 2:
(a) Clinical presentation of scalp impetigo;
(b) Dermoscopical image;
(c) Clinical presentation of erosive pustular dermatosis of the scalp;
(d) Dermoscopical image.
Itching with possible bleeding or pus leaking from the lesions is frequent and may lead to the formation of a secondary yellowbrown crust [2]. Among eschar due to entomodermatoses, we must certainly mention those induced by tick bites. In particular, these may be associated with a characteristic clinical presentation with locoregional lymphadenopathy, as part of a clearly recognized syndrome. The syndrome called TIBOLA (Tick-borne lymphadenopathy) due to its association with a painful swelling of the lymph nodes in the neck following a tick bite [3], was first reported in France in 1997. It subsequently took the name DEBONEL (Dermacentor-borne necrosis erythema and lymphadenopathy) to specify the name of the tick (Dermacentor) involved and to describe the associated symptoms, erythema and necrosis [4]. More recently, however, the syndrome has been renamed with the acronym SENLAT [5] (Scalp Eschar and Neck Lymph Adenopathy After a Tick Bite). The etiopathogenesis is varied and is attributed to infections with Ricketsia (Rickettsia slovaca and R. raoultii), Bartonella and Borrelia. In some cases, the causative agents remain unknown.
The most common cutaneous manifestation of Lyme borreliosis is erythema migrans (EM) [6,7] at the site of a tick bite; other associated presentations can include multiple EM, borrelial lymphocytoma and chronic atrophic acrodermatitis. In case of EM, the diagnosis is clinical and does not require supporting laboratory investigations. Antibiotics are the first line of treatment depending on the clinical stage. In most cases of early localized infection, oral administration of doxycycline is widely recommended as the firstchoice therapy, as it is effective not only against Borrelia bacteria but also against a variety of other tick-borne diseases such as rickettsiosis. Our report highlights the importance of an accurate and detailed medical history in order to provide appropriate treatment for Lyme disease, even in the case of a simple diagnostic suspicion. The inclusion of B. burgdorferi in the differential diagnosis of patients with SENLAT seems justified, especially if the test for Rickettsia spp. is negative. Doxycycline therapy is effective for both infections and should be started as soon as possible.
Conflict of Interest
The authors have no conflict of interest.
References
- Starace M, Loi C, Bruni F, Alessandrini A, Misciali C, et al. (2017) Erosive pustular dermatosis of the scalp: Clinical, trichoscopic, and histopathologic features of 20 cases. J Am Acad Dermatol 76(6): 1109-1114.e2.
- Pfützner W (2020) Infectious skin diseases in childhood. 1: Bacteria and fungi. MMW Fortschr Med 144(25): 24-28, 30.
- Raoult D, Berbis P, Roux V, Xu W, Maurin M (1997) A new tick-transmitted disease due to Rickettsia slovaca. Lancet 350(9071): 112-113.
- Raoult D, Lakos A, Fenollar F, Beytout J, Brouqui P, et al. (2002) Spotless rickettsiosis caused by Rickettsia slovaca and associated with Dermacentor ticks. Clin Infect Dis 34(10): 1331-1336.
- Dubourg G, Socolovschi C, Del Giudice P, Fournier PE, Raoult D (2014) Scalp eschar and neck lymphadenopathy after tick bite: an emerging syndrome with multiple causes. Eur J Clin Microbiol Infect Dis 33(8): 1449-1456.
- Stanek G, Wormser GP, Gray J, Strle F (2012) Lyme borreliosis. Lancet 379(9814): 461-473.
- Shapiro ED (2014) Clinical practice. Lyme disease. N Engl J Med 370(18): 1724-1731.

 Case Report
Case Report