SUMMARY
The purpose of this article is to show the result of a collaborative and transdisciplinary effort between human and veterinary medicine (ONE HEALTH) in fading up the spread of the SARS-CoV-2 among nursing homes and other social-sanitary centres in the province of Almería (Spain). The term One Health, although relatively new, is being increasingly used in conferences, communications, and various organizational frameworks that advocate global health. As the results have shown, this approach benefit not only the individual but the entire community, reducing the number of infections and the transmission of the disease in retirement homes, which would have caused a greater number of ill and deceased.
Results: Of the total of 59 CREs, which accumulate a total number of 3.609 residents, 93 positive residents were registered, belonging to 6 residential centers for the elderly and none belonging to a socio-sanitary center for the disabled. With regard to employees, out of a total of 1.500 there were 38 confirmed positives, all of them from centres that had confirmed positive residents, except for 3 workers who were COVID-19 positive despite working in a centre with no positives registered. The implementation of the basic principles of biosafety imply the creation of environments in which the care of residents is optimized. It is a priority for Public Health to promote disease-control practices among resident people and employees, as it leads to reducing the risk of exposure to the disease, and therefore the threat posed by COVID-19.
Keywords: One health; Public Health; nursing homes; biosecurity; veterinary; medicine; COVID-19
Introduction
The concept “ONE HEALTH” is a methodological approach
conceived to design and apply programs, policies, laws and
research in which the different sectors involved communicate and
collaborate closely with one another in order to achieve the best
results regarding public health, understanding that both human
and animal health are interdependent and necessarily linked to the
environment in which they coexist. This strategy is recommended
by the World Organization for Animal Health (OIE, 1924) to
address the interrelation between Public Health, Animal Health
(including both domestic and wild animals), and ecosystems.
Many pathogenic microorganisms that represent global risks to
public health affect both animals and humans when they share the same habitat, so to concentrate the efforts into just one sector will
not prevent nor eliminate the problem. Examples of this are RNA
viruses-retroviruses, such as the human immunodeficiency virus
(HIV), the West Nile virus, the avian influenza virus, the Zika virus
and, more recently, the coronavirus (SARS, MERS). All these disease
outbreaks, including the current COVID-19 pandemic, illustrate
how essential these transdisciplinary collaborations are [1].
It therefore becomes clear that a comprehensive protection
of public health should be based on the development of global
strategies for the prevention and control of pathogens, through the
implementation of adequate and coordinated policies that act in the
animal-human-ecosystem interface. This is why the FAO Director-
General has recently requested in the context of “One Health” the
inclusion of veterinarians as specialists in animal health in the
prevention and control of COVID-19. Hence, veterinarians play an
essential role in the development and implementation of health
risk management policies: protecting animals health and welfare
and controlling food safety, ultimately public health.
Objectives
General
a. To apply the “One Health” concept to the highly
transmissible and serious pandemic caused by SARS-CoV-2
throughout the collaboration between medicine and veterinary.
b. To establish a multidsiciplinary approach that allows
the control the virus from all perspectives as well as the
understanding of its origin, avoiding new outbreaks.
Specific
a. To assist in the evolution and control of the pandemic as
well as in the relationship between the virus and animals &
humans, applying key concepts such as biosecurity, movement
control and generalized diagnostic tests.
b. To implement early detection and appropriate contingency
plans as the best tool to control infectious disease outbreaks in
residential centers for the elderly (RCE) for which we do not
have effective treatments or vaccines at the present time.
c. To turn RCE into genuine health fortresses with isolation
conditions that prevent the arrival of infectious agents to arrive
or, in case they do, their massive spread.
Methods
A plan with two strategic lines was establish.
Line of Assistance and / or Treatment of the Individual, Developed in turn Through two Action Plans
a. Preparation and implementation of a clinical management
protocol, with daily check-ups of asymptomatic residents residents with compatible symptoms and residents with
positive PCR test results for COVID-19.
b. Urgent medicalization and resource endowment of the
centers through coordination and cooperation between the
nursing homes´ staff, the Primary Health Care Districts and the
Internal Medicine department of the referral hospital.
Line for the Prevention of Infection and/ort Spread of the Disease Among the RCE Population (Elderly Residents and Employees)
This line is as well divided into five action plans:
a. Centralization, coordination and distribution of hygiene
and personal protection equipment.
b. Systematic sampling of the RCE population To this effect,
PCR and serological tests were performed in order to early
identify and contain the infection sources as well as interrupt
the chain of transmission. In advanced stages of the disease,
Ig-M and Ig-G antibody testing were included using the ELISA
technique.
Request for a Contingency Plan and isolation of Residents with Suspicion or Confirmation of Covid-19, Through the Elaboration of a “Plan of Action” Foreseen by the Health Territorial Delegation
Each center must assume a firm commitment to risk
management, leading a systematic implementation of measures to
minimize it, and a guarantee from the Management Office to help
implementing the Contingency Plan and apply the extraordinary
preventive measures recommended by the health authorities. This
Contingency Plan, properly documented, must contain at least:
a. The allocation of authorities for the supervision of
compliance with the recommendations and guidelines issued
by the health authorities in relation to special measures
for COVID-19 and the additional measures contained in the
contingency plan.
b. The allocation of material and human resources.
There must be a detailed list with the available personal
protective equipment (PPE), the sanitary hygiene protection
products (soap and paper towels, hydroalcoholic solution
dispensers, disposable tissues and waste containers, preferably
with a pedal-operated lid) and the cleaning/disinfection products
(bleach, 62-71% ethanol or 0.5% hydrogen peroxide, detergents
and disinfectants with virucidal effect). There must be an estimate
of the needs to guarantee the stock, as well as a list of pre-evaluated
suppliers with possibility of supplying in case of need. With regard
to human resources, the centres must have a file of the available
workers by category and by shift, and the ratio of professionals and
users. Regarding the Personnel Policy, the company must encourage employees with symptoms to abstain from going to work, report
to the occupational risk prevention department and self-isolate at
home for two weeks.
A Personnel Continuity Plan with a substitute employee list
should be established in the event of possible work leaves as a
result of the epidemic. Centres must determine an action protocol
for people with compatible symptoms (cough, fever, shortness of
breath, etc.) or who have been in contact with the former.
a) Description of the Centre´s infrastructures and
Residents´typology
Each Center must have a scale plan that includes all the
existing spaces, volumetric and functionality. A description of the
infrastructures, number of floors, rooms, number of beds in the
rooms, the existence or lack of private bathrooms on each room
and the access systems (stairs, elevator, access landings) must
be made. Each Center must have sufficient material, structural,
organizational and personnel capacity to maintain the isolation of
suspected, probable and confirmed cases.
b) Resident Characteristics, including their level of
dependency, in order to offer them the appropriate healthcare
in the event of SARS-CoV-2 infection. It is recommended to
classify them according to the disease (COVID-19), and their
personal characteristics. Based on COVID-19, residents are
classified as:
a. Asymptomatic with no close contact with probable or
confirmed cases,
b. Asymptomatic in preventive isolation due to close contact
with probable or confirmed COVID-19,
c. With compatible symptoms of COVID-19 and
d. Confirmed cases of COVID-19. Depending on personal
characteristics, they are classified according to their ability
to perform basic activities of daily living (BADLs)* and
instrumental activities of life daily (IADLs)**.
c) Family Communication Plan, so that residents can
maintain bonds and periodic communication with their loved
ones in order to make the temporary isolation due to COVID-19
more bearable, via phone calls, video chats, e-mails, written
letters.
d) Management of a dead body in the context of COVID-19.
Each center must have a documented protocol for handling
infected COVID-19 corpses.
Interpersonal Distance, Training and Qualification of Work Personnel
Protecting the health and safety of employees must be a priority. Tasks must be planned in such a way that the 2-metre safety distance established by the health authorities is guaranteed. To this end, Centres were adapted and guidelines were developed for the distribution of spaces and movement of the people, avoiding the overlap in entrances and common areas such as bathrooms, changing rooms and dining halls. Work shifts were organized so that the same employees were always on the same shifts, avoiding exchanges between groups as well as joint activities. A person in charge was assigned on each working group to ensure compliance with the planned preventive measures. All personnel-including new recruits, work leaves, and R&D personnel-received theoretical and practical training in occupational risks, infection control and potential infectious diseases exposure prevention. For the success of the training program it was subsequently supervised and followed on-site.
Biosafety and Infection Control Measures
The first step in preventing a disease is to understand its
etiology. In COVID-19, the preferred route of transmission and
the route of exposure are believed to be identical, that is through
the respiratory route: from respiratory aerosols (droplets) from
an infected person to a susceptible one [2,3]. Recent studies have
shown that the SARS-CoV-2 virus is capable of remaining suspended
in aerosols for hours [4-6]. However, it is believed that there may
also be a spread by direct or indirect contact with contaminated
surfaces or objects (fomites) where the virus can remain active for
up to several days, depending on the nature of the contaminated
surface [7].
Taking this into account, the following measures were adopted:
Control of the Entry of the Infectious Agent to the Facilities: As a general measure, in order to prevent the entry of the infectious agent into the facilities, the access of non-essential visitors and the exits of residents outside the centre were temporarily interrupted. Movement inside the centre was restricted and all socialization activities, group physiotherapy, and non-pharmacological therapies were suspended. The reception of raw materials and supplies was limited, maintaining a space reserved for the reception/return of merchandise, located near the access door and physically or temporarily separated from the rest of areas. With regard to personnel, employees had to go directly to the changing room area and change clothes and shoes.
Environmental Control of Facilities: Nursing homes
ambient air can constitute a source of contagion for both staff
and residents. Controlling this potential pool of infections is
increasingly recognized as an important component of infection
control and prevention [8]. Natural ventilation by opening doors
and windows for as many hours as possible is considered a simple,
effective measure to this end. It is recommended to maintain a
relative humidity between 40 and 60% in those spaces where
the equipment allows it, since the nasal systems and mucous membranes are more sensitive to infections with humidity below
10-20%. If mechanical ventilation systems are used, it is necessary
to avoid the recirculation of the air in the room and to use systems
that allow the extraction and renewal of it. Frequent filter cleaning
or replacement is recommended.
Regular cleaning and disinfection of equipment and surfaces
is extremely important for the environmental pathogens control.
To facilitate cleaning and disinfection tasks and reduce as well
any equipment or elements that acted as reservoirs, it was
recommended to remove all unnecessary decoration utensils,
paintings, curtains, furniture made of porous materials difficult to
clean, etc. It was recommended to have a documented procedure
specifying the type of product, the application method, the contact
time, the cleaning frequency, and the responsible personnel for
each area of the establishment. These viruses are inactivated after 5
minutes of contact with halogen disinfectants such as hypochlorites.
For surfaces that cannot be bleached, 62-71% ethanol or oxidizing
agents such as 0.5% hydrogen peroxide can be used.
Special attention should be paid to areas where the contact rates are high and increase the cleaning frequencie, especially in those areas of greater contact (knobs, sinks, taps, handles, doors, table surfaces, toilet flush buttons, protection barriers, exits, entrances, stairs, elevators, handrails, armchair supports, wheelchairs, crutches, vending machines, switches, keyboards, etc.). It was recommended to have dispensers with hydroalcoholic solution (with 60-95% alcohol) for hand hygiene, disposable tissues for respiratory hygiene and waste containers with a pedal-operated lid in common areas, work areas, corridors and bedrooms. Bedding and other garments should be washed mechanically with common detergent and in full wash cycles at 60-90ºC.
Quarantines and Isolations: In order to keep healthy individuals apart from suspicious and / or ill people and limit the spread of viruses within the facilities, the centers were zoned into floors or areas (being vertical or floor isolation a preferable grouping criterion). Centers should be able to have, if necessary, at least the following: a floor or area for asymptomatic residents, with no close contact with positive or confirmed COVID-19 patients; another floor or quarantine area for asymptomatic residents who have had close contact with a possible or confirmed COVID-19 and a final floor or isolation area for confirmed residents. The center can use the fire sectorization already defined as the location area for each of the indicated groups, unless this is not possible due to the size of the Center.
Every one of these areas must be correctly marked and identified with a placard, and both access and transit through them must be limited, with exclusive work personnel assigned for each of them. Footbaths and/or mats impregnated with water and bleach were placed for infection control when changing areas and the mandatory use of clogs. All the equipment to be used for this area must be exclusive for it and must be identified with some striking element, for example by colors. No object should leave the quarantine or isolation area without proper cleaning and disinfection or in sealed bags for proper disposal [9-17].
Discussion
Of the total of 59 CREs, which accumulate a total number of
3.609 residents, 93 positive residents were registered, belonging
to 6 residential centers for the elderly and none belonging to a
socio-sanitary center for the disabled. With regard to employees,
out of a total of 1.500 there were 38 confirmed positives, all of them
from centres that had confirmed positive residents, except for 3
workers who were COVID-19 positive despite working in a centre
with no positives registered (Figure 1). Of the residents in Centers
for the elderly and other social health centres, there were a total of
149 confirmed positives, 106 in residential centres for the elderly
and 43 in other social and health centers. There were a total of 16
deaths due to causes attributable to COVID-19, all of them in RCEs
and none in other health centers. 9 of these 16 deaths were within
the residential centre, and the other 7 died during their stay in the
hospital (Figure 2).
The implementation of the basic principles of biosafety imply
the creation of environments in which the care of residents is
optimized. It is a priority for Public Health to promote diseasecontrol
practices among resident people and employees, as it
leads to reducing the risk of exposure to the disease, and therefore
the threat posed by COVID-19. It is vitally important to avoid the
introduction of the infection in a residential center, since the elderly
people are especially vulnerable, they are in close contact with the
caregivers, and the isolation of many of them is impossible. The
joint work of veterinarians, in the prevention and spread of the
disease (COVID-19), and that of doctors, with their commendable
care work, focused on the individual, is necessary to achieve the
best results in Public Health. The practical implementation of
the “One Health” approach, forging professional ties between
doctors, veterinarians, nurses and other workers benefit not only
the individual, but the entire community, reducing the number of
infections and the spread of the disease which could lead to greater
number of ill and deceased.
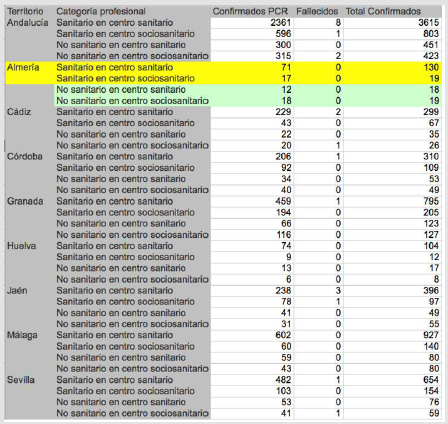
Figure 1: Confirmed, cured and deceased cases of COVID 19 in risk professionals according to their profession. Unit of measurement: number of cases. Both genders.
Figure 2: Confirmed cases, deceased and cured by COVID 19 in populati on living in residences according to sex by province. Unit of measurement: number of cases. Both genders
Acknowledgments
The authors would like to thank for the professionalism, dedication and sacrifice the personnel of these centres has shown in the care of the most fragile and vulnerable, without whom none of this would have been possible.
Competing Interests
None declared.
References
- Atlas RM, Maloy S (2014) One Health: People, Animals and the Environment. American Society of Microbiology, Washington, DC, USA.
- Renyi Zhang, Yixin Li, Annie L Zhang, Yuan Wang, Mario J Molina (2020) Identifying airborne transmission as the dominant route for the spread of COVID-19. Proceedings of the National Academy of Sciences 117(26): 14857-14863.
- Liu J, Liao X, Qian S et al. (2020) Community transmission of severe acute respiratory syndrome coronavirus 2, Shenzhen, China, 2020. Emerg Infect Dis 26(6).
- N van Doremalen Bushmaker, Morris (2020) Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N. Engl. J. Med 382: 1564-1567.
- Alex W H Chin, Julie T S Chu, Mahen RA Perera, Kenrie P Y Hui, Hui-Ling Yen, et al. (2020) Stability of SARS-CoV-2 in different environmental conditions. Lancet 1(1): 10.
- Park SY, Kim YM, Yi S, Lee S, Na BJ, et al. (2020) Coronavirus disease outbreak in call center, South Korea. Emerg Infect Dis 26(8).
- Kampf G, Todt D, Pfaender S, Steinmann E (2020) Persistence of coronaviruses on inanimate surfaces and their inactivation with biocidal agents. J Hosp Infect 104(3): 246-251.
- Agoritsa Baka, Orlando Cenciarelli (2020) Interim guidance for environmental cleaning in non-healthcare facilities exposed to SARSCoV-2. ECDC Technical report.
- (2020) Report on the situation of COVID-19 in health personnel in Spain as of May 07, 2020. Equipo COVID-19. RENAVE. CNE. CNM (ISCIII).
- (2020) Informe COVID-19 nº 30 de marzo de 2020 SiViES. CNE. CNM (ISCIII).
- (2020) Federation of European Heating, Ventilation and Air Conditioning Associations (REHVA) COVID-19 guidance document.
- (2020) Recomendaciones a residencias de mayores y centros sociosanitarios para el COVID-19. Versión de 5 de marzo, de 2020. Ministerio de Sanidad.
- (2020) Guía de prevención y control frente al COVID-19 en residencias de mayores y otros centros de servicios sociales de carácter residencial. Versión de 24 de marzo, de 2020. Ministerio de Sanidad.
- Recomendaciones de actuación para residencias de mayores y centros sociosanitarios para el COVID-19. Junta de Andalucí Consejería de Salud y Familias.
- Actuación en centros residenciales de mayores y otros sociosanitarios asimilados COVID-19. Junta de Andalucí Consejería de Salud y Familias.
- (2019) Informe COVID-19 en Andalucí Junta de Andalucía. Consejería de Salud y Familias.
- (2021) COVID-19 report in Andalusia. Junta de Andalucia.

 Research Article
Research Article