Abstract
Introduction: Bone fracture often occurs in trauma patients. Bone fractures can be open or closed. Although closed, fractures should still be treated as soon as possible because closed fractures in several places can cause a severe occult bleeding that threatens the patient’s life. In adults, fractures can occur in many places, one of which should be considered is the hip as intertrochanter fracture. Impaired walking (asymmetry) is the next symptom that often occurs. It may occur due to compensatory mechanisms of pain or from changes in leg length, weakness of the hip abductor muscles, joint instability and the presence of bone fractures. Patients may complain of disturbances in walking long distances, and some patients begin to use assistive devices to walk. An inter trochanter fracture is one of 3 types of hip fracture. The site of this fracture is in the proximal to the femur. The proximal area of the femur consists of the head of the femur, neck of the femur and the inter trochanter region. Usually an intertrochanter fracture occurs between the major trochanters where the gluteus medius and minimus (hip extensor and abductor) muscles are attached with the minor trochanter to which the ilipsoas (hip flexor) is attached.
Discussion: Inter trochanter fractures of the femur also account for ½ of hip fractures caused by low energy mechanisms such as falling from a standing position. This fracture often occurs in people who have risk factors, including: getting older, women, there is osteoporosis, a history of falls, and abnormalities in walking. Surgery is the recommended therapy because of the high morbidity and mortality rates in nonoperated patients. Usually there are also co-morbidities that accompany, thus affecting the outcome of therapy. Therapy for patients with inter trochanter fractures is of various kinds. ORIF (Open reduction and internal fixation) is indicated in all inter trochanter fractures, except in patients with medical conditions in which anesthesia, both general and spinal, is contraindicated. Total hip arthroplasty has a limited role and is usually performed on patients who also have arthritis of the hip joint. External fixation is also rarely indicated but is very useful as a short procedure in patients who cannot undergo general or spinal anesthesia and can only tolerate local techniques. Medial displacement osteotomy and valgus reduction are no longer performed, because of the resulting severe deformity and improved understanding of fracture fixation.
Conclusion: Patients with intertrochanter fractures can undergo surgery after the medical evaluation or trauma has been performed and the medical condition has stabilized. Surgery is contraindicated when the patient has uncontrolled or uncorrected blood disorders or other metabolic disorders that cannot be corrected with possible death.
Keywords: Fracture; Inter Trochanter; Surgery
Introduction
Bone fracture often occurs in trauma patients. Bone fractures can be open or closed. Although closed, fractures should still be treated as soon as possible because closed fractures in several places can cause a severe occult bleeding that threatens the patient’s life. In adults, fractures can occur in many places, one of which should be considered is the hip (intertrochanter fr. Femur, fr. Femoral neck, disloc and fr. Of hip), pelvis (fr. Pelvis) .1 If the internal rotation is full of pelvis widened but flexed back. This may be a pathological sign of the anterosuperior femoral head, possibly avascular necrosis. However, in young people, pain on internal rotation with hip flexion can be a sign of tearing of the acetabular labrum [1]. Pain in the hip joint is felt in the groin, descending forward toward the thigh, and some to the knee, sometimes knee pain is the only symptom. Pelvic back pain rarely comes from the joints, often the pain originates from the lumbar spine. Impaired walking (asymmetry) is the next symptom that often occurs. It may occur due to compensatory mechanisms of pain or from changes in leg length, weakness of the hip abductor muscles, joint instability and the presence of bone fractures. Patients may complain of disturbances in walking long distances, and some patients begin to use assistive devices to walk [2]. An inter trochanter fracture is one of 3 types of hip fracture. The site of this fracture is in the proximal to the femur. The proximal area of the femur consists of the head of the femur, neck of the femur and the inter trochanter region. Usually an intertrochanter fracture occurs between the major trochanters where the gluteus medius and minimus (hip extensor and abductor) muscles are attached with the minor trochanter to which the ilipsoas (hip flexor) is attached [2]. Aims of this article is to review management of inter trochanter fracture.
Discussion
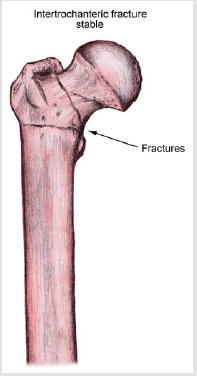
Inter trochanter fractures of the femur also account for ½ of hip fractures caused by low energy mechanisms such as falling from a standing position. This fracture often occurs in people who have risk factors, including: getting older, women, there is osteoporosis, a history of falls, and abnormalities in walking. Surgery is the recommended therapy because of the high morbidity and mortality rates in non-operated patients. Usually there are also comorbidities that accompany, thus affecting the outcome of therapy [3]. The inter trochanter area of the femur is distal to the neck of the femur and proximal to the femoral shaft. This area is where the two trochanters of the femur are located. Major and minor Trochanters. There is a femoral artery and nerve anteriorly and a sciatic nerve posteriorly. The majority of the bones in this area are cancellous, extracapsular, and have high vascularization which allows a strong healing environment to be created. The femoral calcar is a solid component of the posteromedial bone that supports the transfer of pressure from the neck to the femoral shaft.6 The stability of the inter trochanter fracture depends on the amount of contact between the proximal and distal major fragments. A fracture consisting of 2 parts is very stable because when the two halves are reduced, they are attached to each other so that they are stable for the implant [4] (Figure 1).
In a three-part fracture, the stability of the fracture depends on the size of the fragment of the minor tochanter. Instability occurs when more than 50% of the calcar femoral is affected, causing the proximal fragment to fall into the varus position and shorten. Therefore, the fracture is said to be unstable if there is a large minor trochanter fragment or if the major and minor trochanters are separated by fracture fragments (4-part fracture) [5]. Another indicator of fracture stability is the degree of intimacy of the lateral wall of the trochanter, one part of the greater trochanter that extends to form the vastus ridge (attachment of vastus lateralis) to the tip of the greater trochanter. If the wall is fractured, the fixation may collapse at an undesirable position, or the implant will fall off [6]. The more unstable the fracture is, the more difficult it is to reduce and the more indications that implants, such as a cephalomedullary nail, will be needed to stabilize the fracture and prevent collapse. Stable fractures can be treated with a sliding hip screw-plate device. Inter trochanter fracture occurs as a consequence of high force trauma (rarely, usually in males) or from a fall with low force (often, usually in older women). The etiology of low-force inter trochanter fractures is a combination of various factors [5]:
A. Increased bone susceptibility in the inter trochanter of
the femur
B. Reduced flexibility and muscle tone
Increased bone susceptibility can originate from osteoporosis
or osteomalacia, reduced intake of calcium or vitamin D and the
aging process.
Older patients often have pathological conditions that can
reduce the ability to withstand trauma and increase the need
for later rehabilitation. Some of these pathological conditions
include: Cardiovascular insufficiency, hypertension, dehydration,
malnutrition and some metabolic syndromes such as diabetes
mellitus. In younger patients with high-force fractures, it usually
occurs because of an overt trauma process and the potential for
multiple trauma [6]. This pathological condition is obtained from
a complete physical examination, laboratory checks, chest x-rays
and ECG. Additional examinations are required depending on the
clinical needs of the patient. Radiological photos are important
for the diagnosis of inter trochanter fractures. The photographs
that are important are the hip position anteroposterior (AP) and
the lateral position. Pelvic radiographs are also very important in
preparation for surgery. A CT scan is also needed to see the details
of the fracture for accurate surgery [5].
Management of Inter Trochanter Fracture
Therapy for patients with inter trochanter fractures is of
various kinds. ORIF (Open reduction and internal fixation) is
indicated in all inter trochanter fractures, except in patients with
medical conditions in which anesthesia, both general and spinal,
is contraindicated. Total hip arthroplasty has a limited role and is
usually performed on patients who also have arthritis of the hip
joint. External fixation is also rarely indicated but is very useful
as a short procedure in patients who cannot undergo general or
spinal anesthesia and can only tolerate local techniques. Medial
displacement osteotomy and valgus reduction are no longer
performed, because of the resulting severe deformity and improved
understanding of fracture fixation. Surgery is contraindicated when
the patient has uncontrolled or uncorrected blood disorders or
other metabolic disorders that cannot be corrected with possible
death. Surgery is also contraindicated if the patient has a stable,
nondisplaced intertrochanter fracture, which can be treated
conservatively, and refuses surgery for personal reasons [7].
Management of treating comorbidities or other potential
trauma, a 4-stage therapy program is recommended for treating
patients with intertrochanter fractures. In stage 1, fracture
identification is performed on the basis of the history and findings
from physical and radiological examination. Patients with low-style fractures often present with a history of slipping, falling, or twisting
of the lower limb followed by severe pain in the affected pelvic area.
High-style trauma can occur as a result of a traffic accident, a fall
of more than 3 m, or other significant trauma. The patient will be
unable to stand or move his body or affected limb without pain.
Local physical examination may show external rotation in the hip
extension position of the affected limb, and the patient feels pain
with either active or passive movement of the hip joint or affected
limb [8]. The diagnosis of an intertrochanter fracture is confirmed
by the presence of a supportive radiological appearance, including
an anteroposterior (AP) pelvic radiograph, an anteroposterior (AP)
hip radiograph on the affected side, and a lateral cross-table image
of the hip, as well as a hip AP traction radiograph if the operator
does not understand the pattern fracture. The radiological features
above also indicate fracture stability or instability, the need for
fracture reduction, and whether further manipulation is required
to make the reduction stable enough for healing before implant
fixation is lost [9].
In stage 2, stabilize the patient’s medical condition prior to
operative intervention. At this stage, consultation with the internal
medicine department and other relevant sections is required. This
stage also includes identifying any underlying medical conditions
in the patient. If certain medical conditions are found in the patient,
good preoperative management is needed to reduce the potential
postoperative problems that can result from these conditions.
This medical condition can be discovered by a complete physical
examination; heart, lung and laboratory examinations; and other
necessary examinations, which include complete blood count (DL),
urinalysis, chest X-ray, and EKG5,8. Additional investigations may be
required, depending on clinical findings, past and current medical
history, and results of laboratory and radiological screening. Any
medical disorder needs to be treated promptly and as best as
possible before operative intervention is carried out to ensure that
complications do not occur due to delays in initiating treatment.
Precise measurements are needed to reduce the likelihood of
developing DVT and secondary pulmonary embolism (usually
considered preoperative protocol) [6,9].
Stabilization needs to be done as soon as possible. Patients have
a good outcome if the fracture can be stabilized operatively within
24-48 hours of admission. This does not mean that this case is an
emergency case, but in most cases, management and stabilization
should be done and the patient should be in the operating room
within 48 hours. In patients with major force fractures, good trauma
management is required first. The operation is performed as soon
as the patient is stable and the appropriate team of operators is
available [5,10].
Stage 3 includes operative procedures and postoperative
recovery in the hospital. Joint treatment of elderly patients by
orthopedic surgery and internal medicine or geriatrics is highly recommended. When discharged, routine follow-up should be
planned thereafter. Standard postoperative control is indispensable
for all patients. Patients with low-style fractures also require
control in the area of osteoporosis [9,11]. Stage 4 consists of the
rehabilitation of the patient, both in an outpatient facility and in
a rehabilitation facility. The goal is to get the best possible posttraumatic
outcome. In elderly patients, emphasis should be placed
on fall prevention and proper exercise and diet program [8].
Operative Therapy
Patients with intertrochanter fractures can undergo surgery after the medical evaluation or trauma has been performed and the medical condition has stabilized. In September 2014, the American Academy of Orthopedic Surgeons released a clinical practice management of hip fracture in elderly patients. Recommendations include preoperative regional analgesia, immediate surgery (<24 hours after hospital admission), intensive post-discharge physical therapy and evaluation of osteoporosis [5].
Postoperative Handling
After the intertrochanter fracture has been repaired, other nonorthopedic conditions in the patient can be further treated. The DVT prevention protocol is followed by a combination or appropriate choice of antiembolic and anticoagulant stockings. Anticoagulants include aspirin, heparin or heparin derivatives, and warfarin or warfarin derivatives. Anticoagulants require proper monitoring to ensure adequate doses and to prevent over-medication and bleeding. With each treatment or protocol, the dose of therapy given is different, the length of therapy is different, and the combination of medication and anticoagulant use varies [12]. Physical therapy is needed to help the patient walk with the help of a therapist or nurse. The equipment required includes walkers, crutches, fourpost canes, and other assistive devices as recommended by the therapist and surgeon. The therapist directs the therapy program and the use of walking aids based on the surgeon’s instructions. The surgeon indicated a difference between no weightbearing, toe touching, partial weightbearing, and full weightbearing therapy and the proper technique of using a walking aid. Elderly patients may find it difficult to administer full weight-bearing therapy [10].
Complications
Intertrochanter hip fractures have a significant complication rate: 20-30% in the first year, including 5% incidence of non-union, 5% incidence of infection, and 11% of appliance failure. Important measures to prevent complications include7:
A. Follow preoperative sterilization techniques carefully
B. Perform careful preoperative radiological examination
C. Perform proper tool insertion
D. Carry out close postoperative monitoring with clinical
and radiological examinations to ensure fracture healing. Systemic
complications can occur as a consequence of anesthesia (general or
spinal) used in surgery, stress induced by operative procedures, or
even stress in general. Local orthopedic complications may occur
when adequate stable reduction of the fracture is not obtained and
cannot be maintained or if the true position has been lost before the
healing process due to movement associated with daily activities.
Loss of positioning before healing can also occur if the fixator fails
to work due to improper insertion [12].
Conclusion
Patients with intertrochanter fractures can undergo surgery after the medical evaluation or trauma has been performed and the medical condition has stabilized. Surgery is contraindicated when the patient has uncontrolled or uncorrected blood disorders or other metabolic disorders that cannot be corrected with possible death.
References
- Salter, Robert Bruce (1999) Textbook of Disorders and Injuries of the Musculoskeletal System. Lippincott Williams & Wilkins, Baltimore, Maryland.
- Thompson Jon (2010) Netter’s Concise Orthopaedic Anatomy. Elsevier Inc, Philadelphia, USA.
- Solomon Louis (2010) Apley’s System of Orthopaedics and Fractures. Hodder Arnold, Bristol, England.
- Kellam James (2016) Intertrochanteric Hip Fractures. Medspace.
- Ahn Jaimo, Bernstein Joseph (2010) In Brief: Fractures in Brief: Intertrochanteric Hip Fractures. Clin Orthop Relat Res 468: 1450-1452.
- Lumbantobing SM (2001) Neurologi klinik pemeriksaan fisik dan mental UI hal 88-96, Jakarta: Penerbit FKUI, Indonesia.
- Baehr M, Frostcher M (2010) Diagnosis Topik Neurologi DUUS. Penerbit EGC, Jakarta, Indonesia.
- Ahrengart L, Tornkvist H, Fornander P, Thorngren KG, Pasanen L, et al. (2002) A randomized study of the compression hip screw and Gamma nail in 426 fractures. Clin Orthop Relat Res 401: 209-222.
- Grisso JA, Kelsey JL, Strom BL, Chiu GY, Maislin G, et al. (1991) Risk factors for falls as a cause of hip fracture in women. The Northeast Hip Fracture Study Group. N Engl J Med 324: 1326-1331.
- Lindskog DM, Baumgaertner MR (2004) Unstable intertrochanteric hip fractures in the elderly. J Am Acad Orthop Surg 12: 179-190.
- Bhandari M, Schemitsch E, Jonsson A, Zlowodzki M, Haidukewych GJ (2009) Gamma nails revisited: gamma nails versus compression hip screws in the management of intertrochanteric fractures of the hip: a meta-analysis. J Orthop Trauma 23: 460-464.
- Moran CG, Wenn RT, Sikand M, Taylor AM (2005) Early mortality after hip fracture: is delay before surgery important? J Bone Joint Surg Am 87: 483-489.

 Review Article
Review Article