Abstract
This article summarizes what we know and what we need to know about social distancing and its importance in reducing the COVID-19 virus (SARS-CoV-2). Many countries around the world have developed social distancing policies to curb COVID-19 infection rates among their population. The virus that causes COVID-19 is transmitted from human to human, so social distancing is key to mitigating the spread of the illness. According to government and non-governmental organizations reporting on COVID-19 in the literature, there is currently no general consensus regarding social distancing in the workplace. The recommended distances range from 1 to 11 meters. Moreover, neither meteorological parameters nor engineering ventilation methods are taken in account in estimating safe social distancing in the workplace. This study investigates also the importance of using engineering ventilation in healthcare settings, especially during widespread disease outbreaks such as COVID-19. Ventilation can be used to improve indoor air quality in care homes, hospitals, and quarantine locations. Although there are several different types of engineering ventilation, mechanical ventilation is most suitable for reducing the impact and spread of COVID-19 in healthcare and other facilities.
Keywords: COVID 19; Coronavirus; Social Distancing; Air Quality; Ventilation
Introduction
At the end of 2019, a new virus (SARS-CoV-2) appeared in the
city of Wuhan, China. It sickened thousands of people first in China
and then started sickening thousands of people in other countries,
prompting the World Health Organization to declare a pandemic in
March of 2020. The WHO called the disease caused by the novel
coronavirus “COVID-19”, which is short for “coronavirus disease
2019”. Over the past several months, COVID-19 has continued
to spread around the world, infecting people in more than 150
countries. The rapid expansion of the disease is due to many factors,
in particular its biological formation [1], the absence of human
immunity, the lack of information concerning the virus, and other
physical, chemical and meteorological parameters. Throughout
human history, viruses have inflicted misery and disease on
humans. Among the most frequently occurring of viruses resulting
in widespread disease are coronaviruses, which may cause anything
from the common cold to more severe and potentially fatal illnesses
such as Severe Acute Respiratory Syndrome (SARS) or Middle East
Respiratory Syndrome (MERS).
At the end of 2019, a new (novel) coronavirus appeared in the
city of Wuhan, China. The illness caused by this virus was officially
labeled “COVID-19” by the World Health Organization (WHO).
COVID-19 stands for “Corona Virus Disease 2019”. According to
the WHO, the majority of people who are infected with this novel
coronavirus experience either mild or moderate illness that does
not require treatment in a healthcare setting. However, the virus is
more likely to cause severe to fatal illness in the elderly and those
with pre-existing medical conditions such as diabetes or chronic
respiratory issues. The virus is passed from person to person in a
number of ways, including droplet infection when a person with
COVID-19 coughs, sneezes, or speaks. These droplets are relatively
heavy, do not travel far, and quickly sink to the ground. However,
people can catch COVID-19 if they breathe in the infected droplets.
Another way that the COVID-19 virus spreads from person to
person is via fomites.
When droplets from a person’s cough, sneeze, or “talk spray”
land on surfaces near the infected person, other people may catch
the disease by touching these surfaces (doorknob, elevator button,
handrail, etc.) and then touching their face, particularly their mouth,
nose and eyes. Virus particles from COVID-19 may stay viable
on fomites for up to several days, depending on environmental conditions. To reduce the impact of COVID-19, most countries
around the world have imposed numerous restrictions of movement
and socializing on their populations. Some restrictions are very
stiff, such as prohibiting people from going outside for several days.
Most domestic and international borders are also closed. Even
without the threat of contracting COVID-19, governments have
been paying more and more attention to air quality over the past
few decades, both indoor and outdoor. In fact, indoor air quality
is related to outdoor air quality. According to scientific studies [2-
5] and recent satellite images, outdoor air quality has improved
during the pandemic period.
This is because industrial activity has mostly shut down,
temporarily slashing air pollution levels around the world [3-5].
On the other hand, many countries have been extensively using
commercial disinfectants. These chemical products can have a
negative impact on human health and on-air quality (outdoor and
indoor). Some products used as disinfectants, such as chloride, can
also have a deleterious effect on stratospheric ozone. Additionally,
air quality can be reduced by solid wastes. During a pandemic
period, there is an augmentation of solid wastes. However, these
wastes may be improperly managed, as is the case now during the
COVID-19 pandemic [6]. Solid wastes that are improperly managed
can affect air quality and our environment. Hospitals and other
care facilities produce a huge quantity of medical wastes [5]. The
medical wastes are mainly composed of gloves, masks, textiles,
needles, sanitizers, and disinfectants.
For example, the hospitals in Wuhan produced an average of
240 metric tons of medical waste per day at the height of their
initial outbreak, compared to their previous average of fewer than
50 tons. A sudden drop in IAQ has likely resulted from COVID-19-
related effects. Isolating or quarantining at home has become the
global norm nowadays to protect people from the virus, but at the
same time a lack of information of how the virus spreads and who
is susceptible may be leading to poor IAQ [7]. It is worth noting
that while the virus can infect people of any age, the hardest hit
demographic currently is the elderly, especially those residing
in care homes. The engineering ventilation should be designed
according to the specifications of the American Society of Heating,
Refrigerating and Air-Conditioning Engineers (ASHRAE). More
details can be found on the ASHRAE website (https://www.ashrae.
org/technical-resources/standards-and-guidelines). To stop the
spread of COVID-19, many measures are suggested to be taken,
such as frequent handwashing, avoiding the touching of eyes, nose
and mouth, using medical and cloth masks, staying home as much
as possible, and following social distancing guidelines.
These measures are being taken in order to protect human
health, to reduce the impact of the virus, and to provide an
environment that is safe to reopen society. In the present study, our
investigations are focused on indoor air quality (IAQ). Addressing
IAQ is key to protecting human health in an enclosed building. Most
people spend more than 90% of their time in enclosed residential,
industrial or commercial structures. This percentage has risen
dramatically during the COVID-19 pandemic, as millions of people
have been mandated to stay at home, including working from home.
The present paper focuses also on social distancing. According to
the WHO, social distancing means maintaining at least a 1-meter
(approx. 3-foot) distance between people when interacting in the
workplace, shops, parks, etc. Social distancing is an important
method for protecting human health and reducing the impact of the
disease outbreak around the world. This form of physical distancing
is recommended to be applied in schools, airports, restaurants, and
healthcare facilities, and in many countries, social distancing has
now become mandatory.
According to Prin and Bartels (2020), during the 2009 influenza
A (H1N1) pandemic, social distancing contributed to a 23% median
decline in the cumulative influenza attack rate in the workplace.
Social distancing is important because when someone coughs,
sneezes or speaks, they emit small liquid droplets from their nose
and mouth. If the person is infected with the novel coronavirus,
these droplets can spread COVID-19 to people breathing them in or
touching them and then touching their eyes, nose or mouth. During
the present study, the importance of social distancing is investigated.
The main objective of this paper is to study the positive impact of
air profiles in an enclosed building space (operation room). Air flow
speed and direction can play an import role in social distancing, and
this factor should be taken into account by healthcare authorities.
In this study, a series of recommendations is given to protect
workers and staff in enclosed buildings as well as people outside
the building.
Engineering Ventilation in Hospital Buildings
Natural Mode Ventilation
The natural mode ventilation is based on air supply coming
through windows and doors. The replacement of indoor air
generally occurs under natural conditions in structures that have
abundant windows and doors that are not air-tight and induce air
currents that move along corridors and in and out of rooms. In this
case, there no conditions for the requirement of pressure to move
the air in or out. In care facilities, however, this mode of ventilation
cannot be used, as windows are mostly for lighting purposes and
cannot be opened, and there are only a few doors. Furthermore,
natural ventilation cannot occur in operation rooms, bronchoscopy
units, or waiting rooms, all of which typically have no operable
windows. There is essentially no control over the indoor air under
a natural mode of ventilation, as the dispersion of the air cannot be
effectively managed. Hence, any contamination existing in the air
can be easily spread throughout the building.
Natural ventilation is therefore not recommended for hospitals
and places of quarantine that house infected patients. A recent
incidence of high infection occurred in a care home in the province of Quebec, Canada. All of the staff and residents became infected
with COVID-19. The local authorities did not understand this
phenomenon, as appropriate distancing was being observed, as
well as the wearing of personal protective equipment (PPE). In
this case, however, the infection was due to poor quality indoor
air that had become contaminated with the virus. The mass of air
within a building must be frequently changed according to ASHRAE
standards, as building air ages. When air spends too much time in
a building, it becomes dangerous for human health. In fact, bacteria
and viruses can use the surface of aerosols to spread and thereby
infect occupants of these buildings. In the case of the care home
in Quebec, the building was not ventilated according to ASHRAE
standards.
It was relying on natural ventilation, but this type of ventilation,
as mentioned previously, is generally ineffective in large, enclosed
buildings. On the other hand, in terms of energy and investment,
the natural mode of ventilation is practically free, which is why it is
preferred in institutional settings.
Mechanical Mode of Ventilation
This forced mode of ventilation requires equipment, energy, maintenance, and technicians. The advantage of mechanical ventilation is that IAQ can be controlled, along with the air pressure. This means that the changing of air within a building can be adjusted to adhere to ASHRAE standards. To freshen the IAQ, indoor air is extracted from the building via an exhaust fan. The mode of mechanical ventilation systems mainly comprises supply fans (which enable the entrance of outdoor air into a building) and exhaust fans (which extracts air out of a building). Mechanical ventilation is recommended for care homes, hospitals, quarantine places, other healthcare facilities, and residential long-term care facilities.
Mixed Mode of Ventilation
In this mode, natural and mechanical ventilation are combined to provide the desired flow rate. A technician can switch to mechanical ventilation when the natural ventilation cannot guarantee the desired flow. This mode of ventilation is recommended for care homes and residential long-term facilities. In other healthcare settings, such as hospital wards in older facilities, mechanical ventilation is not usually required, as freshening the air through openable windows is the preferred solution.
Air Treatment
The current COVID-19 pandemic has brought building exhaust
air to the attention of authorities. Exhaust air can affect outdoor air
quality and infect populations, especially if comes from care homes,
hospitals, care facilities, and residential long-term facilities where
infectious disease is present. This air should be treated before venting
it outdoors. However, the reality is that the exhaust air of medical
facilities or quarantine places is not treated and escapes outside to infect other sectors of the population. A suitable engineering
solution is to collect this air and consider it Class 4 according
to ASHRAE standards. Class 4 air refers to air with potentially
dangerous particles, bio-aerosols or gases at concentrations high
enough to be considered harmful. Consequently, any exhaust
ducts which carry these potentially harmful Class 4 contaminants
should be negatively pressurized, thereby preventing potentially
hazardous exhaust air from impacting people outside the building
and its environs.
In the case of hospitals, care homes, other care facilities and
quarantine places, the minimal distance between exhaust and
supply should be 5 meters, according to ASHRAE standards, and
the outflow of contaminated air should be a minimum of 5 liters
per second per square meter. The positioning and placement of
the exhaust and supply air are critical to these calculations. The
positioning is chosen according to a simulation of the contamination
spread. In the present study, the engineering solutions are
specifically proposed to reduce the impact of COVID-19 in hospitals,
care homes, and other care facilities.
Medical Wastes
The medical sector generates copious amounts of different kinds of wastes. This includes discarded surgical gloves, surgical instruments, needles used to give shots or draw blood, masks, sanitizers, disinfectants, gowns, eye protectors (goggles or face shields), other PPE, and medications [8,9]. Medical wastes are classified as hazardous wastes on the basis of their biological, chemical, and physical properties. These materials are either toxic, reactive, ignitable, corrosive, infectious or radioactive, which means they should be stored in a safe place before being moved to their final waste-treatment location and disposed of. The location of waste storage within healthcare premises must be properly determined and sized [10]. It should also be under negative pressure, as these wastes can infect an entire building and its occupants. Hence, medical wastes should be professionally treated according to local bylaws and in adherence to the international convention of hazardous wastes. There are a number of engineering techniques for treating medical wastes, including incineration, thermal treatment, biological treatment, landfilling, neutralization, macro-encapsulation, and deep well disposal [11].
Social Distancing in Hospitals
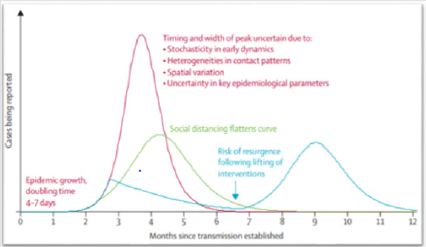
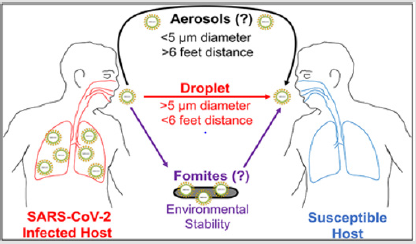
Based on our investigations of the WHO website, social distancing as recommended by the WHO is 1 meter (3 feet) for the following reasons: “People can catch COVID-19 by touching contaminated surfaces or objects, and then touching their eyes, nose, or mouth. If they are standing within 1 meter of a person with COVID-19, they can catch it by breathing in droplets coughed out or exhaled by them. In other words, COVID-19 spreads in a similar way to the flu.” How many meters we should we leave between us and other people in schools, shops, healthcare facilities, parks, etc.? In exploring a broad range of scientific works on the topic, we could find no consensus among the information concerning measurement of social distancing [12-19]. Several articles decribe, define and give advantages of social distancing during the COVID-19 pandemic [12- 20] and also discuss the benefit of social distancing to reduce the impact of COVID-19 (Figure 1), but the precise measurement is not yet agreed upon by experts in the field.
Unlike the WHO’s recommendations, some studies suggest a social distancing measurement of 2 meters between people [21, 22], while another study found that, based on simulations, the droplets (100-200μm) can be transported between 8 to 11 meters by the action of turbulent air flow [23]. This distance can also be changed according to droplet diameter (Figure 2). In other study [24], a droplet with a 100μm was transported up to 3 meters in less than 1 second. Generally, the majority of the countries in the world are encouraging people to stay home throughout the pandemic. The slogan “Stay Home” has been used widely to limit human contact. Many countries have also imposed more restrictive measures, such as isolation and quarantine. However, social distancing is not determined explicitly by the authorities and governments. Recently, many countries and local authorities set out their plans for a phased ending of coronavirus lockdown, with many of the measures imposed including social distancing.
According to our investigation, physical distancing differs from
country to country. For example, in the United States, the Centers for
Disease Control and Prevention (CDC) and the Occupational Safety and Health Administration (OSHA) have recommended a spacing
of 6 feet between people to decrease the spread of COVID-19 in
the workplace [25,26]. In Singapore, non-medical people who
spend a prolonged period within 2 m of a confirmed case must
self-isolate for 14 days [27]. Canadian authorities are requiring
a 2-meter distance in most public and commercial locations, and
Middle Eastern countries also require 2-meter spacing. In Europe,
Col. Rodney Coldren, chief of Preventive Medicine Services, Public
Health Command Europe, is asking people to stay as far away from
each other as possible. There is as yet no consensus in Europe
concerning social distancing. In France, the distance is 1 meter,
while in Germany the distance is 1.5 meters.
Chinese authorities have stipulated 1-meter distancing in
schools, but social distancing measures in Japan are quite lax.
From the above, it is clear that there is no international consensus
on social distancing. To date, social distancing ranges between
1 to 2 meters but can also be as high as 11 meters in relation to
droplet spread. The international rules established by authorities,
healthcare, and local governments are practically the same for
outside (i.e., parks) as for inside (i.e., enclosed workplaces).
Numerous factors should be taken in account to determine social
distancing, including meteorological parameters such as wind and
air flow direction, temperature, and humidity. Unfortunately, the
CDC, OSHA, and WHO have not considered these parameters when
declaring their rules. Some countries require barriers between
workers or staff in workplaces, and these barriers are considered
sufficient to make the workplace “safe”.
However, while such barriers can reduce the spread of the
virus, they cannot stop it, as the virus can float through air
currents. In certain workplaces, infected air can bypass physical
obstacles and be driven by air flow velocity and direction. These
factors change from one workplace to another depending on the
mode of ventilation used (natural, mechanical, or mixed). Wind
and air flow profiles can also change according to the nature of
the barriers and obstacles. Therefore, the ventilation strategy
adopted at a workplace can play an important role in determining
the type of social distancing that should be used. Social distancing
parameters should not be fixed (that is, the same for all places and
all people at all times), but instead be able to be altered according
to meteorological parameters, temperature profiles, the profile of
the air flow, and the position and debit of ventilation (in the case of
mechanical of mixed mode of ventilation). Thus, the positioning of
workers and staff should be based on parameters that are relatively
unique to each workplace (Figure 3).
As depicted in Figure 3, the direction of the air flow within a
building can play a crucial role in determining the spread of the virus
in the workplace. Hence, the correct positioning of workstations
and care beds is essential. In hospitals or other healthcare facilities
in particular, air flow profiles in the rooms should be used to reduce
the transmission of the virus to staff and patients. This technique
can also be useful for dental clinics.
Conclusion
Air quality is an important factor that can profoundly influence
human health. More attention should be given to the IAQ in care
homes, quarantine locations, hospitals, and residential long-term
facilities, as these places house a vulnerable population that can
be easily infected. To reduce the impact of COVID-19 during the
current pandemic, aerosols, particulate matter, viruses and bacteria
can be removed from building air with a suitable ventilation
design. The ventilation approach should be designed according
to ASHRAE standards and be under the consultation of highly
qualified engineers and researchers. In medical facilities, including
places of quarantine, the mixed mode of ventilation is optimal. As
well, the ASHRAE standard should be respected with regard to the
exhaust and supply air. Exhaust flow air should be at least 5 liters
per second per square meter, and a surface of at least nine meters
square should be guaranteed to each patient. Moreover, patients
who are confirmed to be COVID-19 positive should be separated
from other patients and housed in a room under negative pressure.
Furthermore, the exhaust air from this room should be treated,
as without treatment this air can be dangerous and contaminate
other residents both inside and outside the facility. In the future,
more attention should be paid to engineering ventilation as a
means to improve air quality in enclosed buildings. Additionally,
the position of exhaust and supply air should be investigated, as the
suitable positioning of these air flows can improve IAQ immensely
and reduce the impact of viruses. It is also recommended that
ventilation be stopped during the night in care facilities. At the
beginning of the COVID-19 pandemic, the majority of social,
educational, healthcare, economic and industrial activities
temporarily ceased operations. As well, international boundaries
were closed to stop the spread of the novel virus among vulnerable
populations. Now, with the passing of the first wave of illness,
the majority of countries have decided to reopen most activities
gradually throughout the summer.
To prepare for the reopening, policies are being developed and
imposed, with social distancing being one of the most important
and ubiquitous. The concept of social distancing was defined and
explored in this paper, first by reviewing the literature related to
the idea and then by considering it from a technical perspective,
according to the most recently published scientific papers on social
distancing, the recommended distance range between people
should be anywhere from 1 to 11 meters, depending on the activity
being engaged in. This measure is based on numerical simulations
of the propagation of 100 μm droplets. However, for most countries,
social distancing has been set at 1 to 2 meters. For social distancing
measures in the workplace, positioning of workers, staff, shoppers
and patients should depend on a variety of factors, including
meteorological parameters, air flow profiles and velocity, and the
impact of the engineering ventilation.
According to our investigations, the social distancing measures
as required by most established policies are insufficient to protect
human health in workplaces and reduce the spread of COVID-19. In
some workplaces, barriers have been erected between workers and
staff, but these physical obstacles are ineffective if air flow velocity
and direction are not taken in account.
Acknowledgments
The author of this paper thanks specially the Deanship of scientific research at University of Tabuk and my scientific collaborators.
Funding
This work was supported by the Deanship of Scientific Research at University of Tabuk [Grant number S-0048-1441].
References
- Prin M, Bartels K (2020) Social distancing: implications for the operating room in the face of COVID-19. Canadian journal of anaesthesia. Journal canadien d'anesthesie p. 1-9.
- Dutheil F, Baker JS, Navel V (2020) COVID-19 as a factor influencing air pollution? Environmental Pollution.
- Watts J, Kommenda N (2020) Coronavirus pandemic leading to huge drop in air pollution. The Guardian 23.
- Saadat S, Rawtani D, Hussain CM (2020) Environmental perspective of COVID-19. Science of The Total Environment 728: 138870.
- Zambrano Monserrate MA, Ruano MA, Sanchez Alcalde L (2020) Indirect effects of COVID-19 on the environment. Science of The Total Environment 728: 138813.
- Nzediegwu C, Chang SX (2020) Improper Solid Waste Management Increases Potential for COVID-19 Spread in Developing Countries. Resources, Conservation, and Recycling 161: 104947.
- Zakaria Abouleish MY (2020) Indoor Air Quality and Coronavirus Disease (COVID-19). Public Health.
- (2020) Organization WHO. Infection prevention and control during health care when COVID-19 is suspected: interim guidance, 19 March 2020. World Health Organization.
- Huang L (2020) Special attention to nurses' protection during the COVID-19 epidemic. BioMed Central.
- Al Khatib IA, Majed I Al Sari (2020) Medical waste management at three hospitals in Jenin district, Palestine. Environmental Monitoring and Assessment 192(1): 10.
- Jiri JK (2020) Minimising the present and future plastic waste, energy and environmental footprints related to COVID-19. Renewable and Sustainable Energy Reviews 127: 109883.
- Lewnard JA, NC Lo (2020) Scientific and ethical basis for social-distancing interventions against COVID-19. The Lancet. Infectious diseases pp. S1473-3099
- Adolph C (2020) Pandemic Politics: Timing State-Level Social Distancing Responses to COVID-19. medRxiv.
- Singh R, Adhikari R (2020) Age-structured impact of social distancing on the COVID-19 epidemic in India. arXiv preprint arXiv.
- Kissler SM (2020) Social distancing strategies for curbing the COVID-19 epidemic. medRxiv.
- Viner RM, Jessica Packer (2020) School closure and management practices during coronavirus outbreaks including COVID-19: a rapid systematic review. The Lancet Child & Adolescent Health 4(5): 397-404.
- Briscese G (2020) Compliance with covid-19 social-distancing measures in italy: the role of expectations and duration. National Bureau of Economic Research.
- Friston KJ (2020) Second waves, social distancing, and the spread of COVID-19 across America. arXiv preprint arXiv pp.13017.
- Stein RA, Vladimir Litvak, Cathy J Price, Rosalyn J Moran, Christian Lambert, et al. (2020) COVID-19 and rationally layered social distancing. International Journal of Clinical Practice pp. e13501.
- Anderson RM (2020) How will country-based mitigation measures influence the course of the COVID-19 epidemic? The Lancet 395(10228): 931-934.
- Abel T, McQueen D (2020) The COVID-19 pandemic calls for spatial distancing and social closeness: not for social distancing! International journal of public health 65: 231.
- Guzman M (2020) Bioaerosol size effect in COVID-19 transmission. Preprints.
- Guerrero N (2020) COVID-19. Transport of respiratory droplets in a microclimatologic urban scenario. medRxiv.
- Stariolo DA (2020) COVID-19 in air suspensions. arXiv preprint arXiv pp. 05699.
- Galbadage T, Peterson BM, Gunasekera RS (2020) Does COVID-19 Spread Through Droplets Alone? Frontiers in Public Health 8: 163.
- Sen Crowe B, McKenney M, Elkbuli A (2020) Social distancing during the COVID-19 pandemic: Staying home save lives. The American Journal of Emergency Medicine 38(7): 1519-1520.
- Lie SA (2020) Practical considerations for performing regional anesthesia: lessons learned from the COVID-19 pandemic. Canadian Journal of Anesthesia/Journal canadien d'anesthesie 24: 1-8.

 Research Article
Research Article