Abstract
The Introduction starts with the unusual case of three consecutive cancers (uterine cervix, ovarian and rectal) and their relapses in one patient, requiring several surgical procedures, sometimes in emergency settings. Methods We drew a minute analysis of this case, which was operated on in the First Clinic of General Surgery and Surgical Oncology of the Bucharest Oncology Institute, and we looked into the details and examined the clinical context in which a series of surgeries were needed: at first, in the beginning of the disease process, for surgical oncologic reasons - and, further on, in the case of tumour relapse, in order to perform life-saving interventions. Results The surgical personal patient history, in this case, is impressive: the patient was initially histerectomised for a cervical tumour, a few years after she presented with an intraabdominal cystic tumour, which was diagnosed as ovarian cancer relapse, and after that she underwent further chemotherapy and, afterwards, a rectal tumour was diagnosed and treated with preoperative radiotherapy and abdomino-perineal resection.
This year she presented with a bleeding tumour at the level of the vagina which was biopsied and treated with radiofrequency ablation and afterwards the patient addressed the hospital in intestinal obstruction with an enterovaginal fistula. The fistular path was found, it was in strict adherence to the pelvic floor, and the lesional process was shunted by an ileocaecal anastomosis. In the postoperative period, the patient developed an anastomotic leak, and a median ileostomy was performed. Conclusion of this retrospective case analysis would lead towards the fact that, in such unusual cases, in which the surgeon must deal with several complications from cancer and cancer relapse, in the context of multiple primary tumours, it becomes imperative to try to solve the surgical emergency setting and not to try in vain to cure the advanced stage of disease through extensive and dangerous resections in a frail patient.
Keywords: Cancer of the Uterine Cervix, Ovarian Cancer, Rectal Cancer, Cancer Relapse, Triple Cancer, Multiple Primary Cancers (MPC)
Introduction
The number of patients living after cancer diagnosis is better every day due to the advances in treatment. The probability of a patient suffering from multiple primary cancers also increases due to better survival rates, long term side effects of chemotherapy and /or radiation therapy. One of the accepted definitions in use is: multiple primary cancer is the appearance of more than one synchronous or metachronous cancer in the same patient. The definitions proposed come from the Surveillance, Epidemiology and End Results Program and The International Agency for Research on Cancer (IACR/IARC). Varying with the source, overall reported frequency of multiple cancers varies between 2.4% and 17%. Underlying factors for the above-mentioned condition might include genetic factors, host and lifestyle related factors and treatment related factors.
The Case
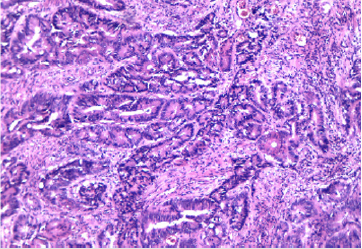
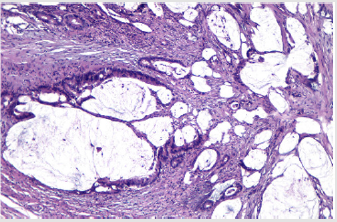
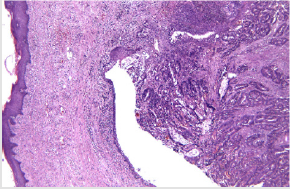
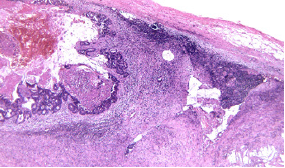
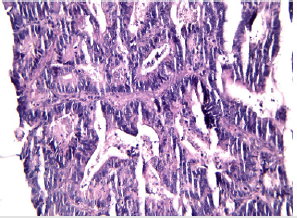
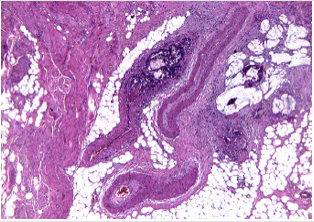
IN 1999, When the patient was 37, a cancer of the uterine cervix debuted (stage IA2), and the patient had total hysterectomy. In 2003, a neoplasm of the ovary was diagnosed and treated (Pathology result: endometrioid adenocarcinoma, grade II), for which bilateral adnexectomy and omentectomy were performed. Further on, the patient pursued chemotherapy. In 2017, a rectal cancer (pathology report: moderately differentiated mucinous adenocarcinoma), was diagnosed for which the patient received radiotherapy and, after that, abdomino-perineal resection. In June 2020, the patient presents with a bleeding vaginal tumor, relapse from the ovarian cancer (Pathology exam: tumor with aspects of papillary adenocarcinoma). The procedure performed was radiofrequency ablation for haemostasis . In September 2020, the patient presents with an enteral- vaginal fistula secondary to a non- resectable pelvic relapse, a block communicating with the small bowel loops and further on with the vagina, with a vaginal discharge of small bowel content of approx 1L/day.
The surgical intervention performed was an internal digestive derivation (ileal-caecal anastomosis) and exclusion ligations of the fistulised loop. After the operation, a fistula of the ileal-caecal anastomosis occurred with faecal peritonitis. In an emergency setting, due both to the nature of the disease and to systemic infection signs, reoperation was performed, and an ileostomy was performed (Figures 1-8) [1].
Discussion
In a study performed by Shinohara et al (1990), [2] (in which there were taken into consideration 17 multiple primary cancers including 16 double cancers and one triple cancer out of 316 patients with gynaecologic malignancies), it was found that the incidence of multiple primary cancers in gynaecologic malignancies was 5.4%. The most frequently encountered site of a second cancer, apart from the genital “primer” location was the large intestine/rectum, a phenomenon which we also noticed in our patient. We also find interesting to discuss, the association between colorectal cancers and other malignancies, departing from a study which investigated colorectal cancer in the context of multiple primary malignant neoplasms [3,4]. The conclusion was that colorectal cancer may share etiologic factors with hormone dependent neoplasms.
Of course, that new primary cancers can occur in patients with a previous neoplasm –then intercedes the question: among the risk factors, therapies such as chemo and radiotherapy and hormonal therapy have been traditionally associated with the development of neoplasms? The general opinion in the literature has been that yes - until rather recently. Nevertheless, a pilot study on the occurrence of multiple cancers following cancer related therapy at the University of Florida - Seegobi [4] states that there is no statistical difference in the rates of second cancers after exposure to chemotherapy, radiotherapy, hormonal therapy. In an article [5] discussing the therapeutic possibilities and limits in multiple primary carcinomas: taking into consideration a total of 38 cases, the authors found a mean survival of 5.53 years in 17 patients with synchronous tumours and more than 10 years in the 21 cases of metachronous tumours. In the present case from this article the patient was under observation in the 21st year after the diagnosis of the cervical cancer, the 17th year after the ovarian cancer and in the third year after the rectal cancer.
Another aspect that we would like to underline is that the multitude of interventions which proved (after all) successful were done and indicated even though the patient was not from the same city as the surgical center. Therefore, the precision and promptness of the diagnosis were lifesaving. We also looked at the literature for that matter and we found a multicenter study “Does distance to treatment affect mortality rate for surgical oncology patients?” by Garstka et al Am Surg 2020 sept [6], a study including 1 424 482 patients -the conclusion being that the increased distance travelled for surgical care had a significant correlation with lower mortality rates for multiple cancers, highlighting the importance of centralized referral patterns for oncology care [7,8].
The discussion section cannot be ended without a brief reminder of the phenomenon of multiple operations on the same patient (MOSP) in the study of which we found a record patient which underwent 27! Procedures of spine surgery. Also, the literature concerning -this time - abdominal multiple primary cancers and therefore a more similar situation to the one we are presenting, describes difficult clinical contexts, like ours, in which the surgeons had to intervene in emergency settings, secondary to complications such as bowel obstructions. [9,10].
Conclusion
Considering the frailty of the patient, due to multiple cancers and consecutive cancer treatments and multitude of complications, the series of surgical interventions was only at first imposed by the surgical oncology indications, and, afterwards, by the urgent need to solve a surgical complication which was life-threatening. Curative surgery at first, followed by palliative surgery further on. How many surgeries are (could be) too many in the life-saving process?
References
- Copur MS, Manapuram S (2019) Multiple Primary Tumours Over a Lifetime. Oncology (Williston Park) 33(7): 629384.
- Shinohara M, Matsuura Y, Baba S, Kashimura M (1990) Multiple primary cancers associated with gynaecologic malignancies. Nihon Sanka Fujinka Gakkai Zasshi 42(6): 561-566.
- Seegobin K, Staggs E, Khawaja R, Maharaj S, Gautam S, et al. (2018) Pilot study on the occurrence of multiple cancers following cancer related therapy at the University of Florida Jacksonville (2011-2016). J Investig Med 66(7): 1050-1054.
- Garcia Anguiano F, Marchena Gomez J, Aguiar Morales JA, Gomez Guerra G, Conde Martel A, et al. (1995) El cancer colorectal en el contexto de las neoplasias primarias malignas multiples. Rev Esp Enferm Dig 87(5): 369-374.
- Demandante CG, Troyer DA, Miles TP (2003) Multiple primary malignant neoplasms: case report and a comprehensive review of the literature. Am J Clin Oncol 26(1): 79-83.
- Knast W, Strutynska-karpinska M, Rabczynski J (2001) Surgical treatment of patients with multiple carcinomas. Med Sci Monit 7(6): 1256-1262.
- Popova TN, Sel’chuk Vlu (2002) Khirurgicheskoe lechenie previchno-mnozhestvennykh sinkhronnykh (Surgical treatment of multiple primary neoplasms). Khirurgiia (Mosk) (8): 28-31.
- Garstka M, Monlezun D, Kandil E (2020) Does Distance to treatment Affect mortality rate for surgical oncology patients? Am Surg 86(9): 1129-1134.
- Oancea TG, Horvat T, Singer D (1993) Therapeutic possibilities and limits in multiple primary carcinomas: consideration of 38 cases. Eur J Surg Oncol 19(1): 1-9.
- Al Baqmi KH, Al MUdaiheem FA, Boghdadly S, Al Hussaini KA, Shokor N, et al. (2020) Multiple Primary Malignancies of the colon, stomach and kidney in a patient with bowel obstruction requiring emergency surgery a case report. Am J Case Report.

 Research Article
Research Article