Abstract
Background: Our genetic code can make a difference in how our body function. There is a significant interaction between our environment and our genes. Our diet is one of the most basic and potentially component of our environment .How our gene determine our response to nutrients in food is still controversy. Determination of blood groups and red cell Lewis phenotype provide a simple method for measuring the prevalence of nonsecretors within children with Coeliac disease.
Methods: We screened thirty one known Coeliac patients on gluten free diet and twenty seven age and gender matched control for ABO & Rh using standard technique and Lewis phenotypes by gel column agglutination tests (ID-Cards- Bio Rad) in central Blood bank at Tripoli University hospital.
Results
a) Determination of ABO and Rh alone did not contribute to the susceptibility of Coeliac disease.
b) 48.4% of Coeliac patients and 36% of control group and 52.9% of Coeliac and 37.5 % of control blood group O , were Le a+b- (non-secretor), these results did not reach a statistically significant differences.
Conclusions: No firm relationship between ABO, Rh, Lewis non-secretor state and Coeliac disease in this study.
Keywords: -ABO; – Rh; –Lewis; – Coeliac
Introduction
We are what we eat, is one face of the coin, the other face is the genetic makeup, one man’s diet is another man’s poison. Our inherited genes from our parents and their DNA combines to create our unique genetic makeup, this can include the obvious ones such as the colour of our eyes to more complex traits that involve multiple genes such as risk of diseases including diabetes, heart disease, obesity and cancer. Human genome has been proposed to contribute to interpersonal variability in the way we respond to nutritional intakes. Coeliac disease from the other side arises from immunological sensitization of small intestine to dietary gliadin and is associated with HLA.DQ2, HLA.DQ8 on chromosome 6. Environmental factors and other non-HLA associated genes may contribute to the developmental of overt disease. Patients who cannot secrete ABO and Lewis blood group antigens into body fluids, an ability controlled by a single gene on chromosome 19, are known to be at increased risk of bacterial, fungal, viral, allergic conditions, gastrointestinal diseases, malignancy, and some autoimmune disorders associated with other markers [1-5]. This study was conducted to determine the association between ABORh , Lewis phenotypes and Coeliac disease in Libyan children.
Subjects and Methods
A case- control study was conducted in Paediatric Gastroenterology outpatient clinic and inpatients at Tripoli University hospital. 58 children aged 20 months to 14 years (the mean age 7years and 7 months) were included in this study, of which 31 children were known Coeliac disease, based on clinical, positive serology (anti tissue transglutaminase IgA and IgG), histopathological finding according to Marsh classification and clinical response to Gluten Free Diet (GFD). Those who did not fulfill any of these criteria were excluded. Twenty-seven non Coeliac control, with minor illness were randomly selected by independent doctor from Paediatric outpatient clinic during the same period. After verbal consent from parents/ patients, blood samples were collected from all participants in this study and tested for ABO, Rh using the standard technique, and Lewis phenotypes by gel column agglutination tests ( ID-Cards-Bio Rad ,Laboratories, Inc ) in central blood bank at Tripoli University hospital.
Statistical Analysis
The statistical analysis of the data was carried out using statistical package for social sciences (SPSS) version 23.0 software programme for Window. Mann Whitney U test, and Pearson Chi square statistics corrected with Yates were used for statistical evaluation of significance between Coeliac and control groups. A “P” value less than 0.05 was regarded as statistically significant.
Results
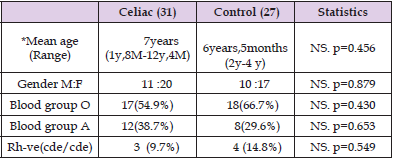
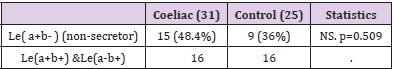
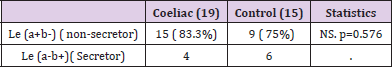
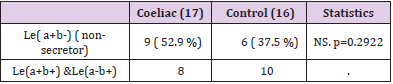
Thirty one known Coeliac patients , mean age at the time of the study was 6.8 y ( 22months-12.4y), 20 females (64.5% ) and 11 males (35.5%) and 27 matched age and gender controls. The most observed ABO blood group among Coeliac patients and control were blood group O (54.8 %-66.7%) followed by Blood group A (38.7%-29.6% respectively , Rh-ve was 14.8% in control and 9.7% in Coeliac. There were no significant differences between Coeliac and control groups in the prevalence of blood group O (p=0.430), blood group A (p=0.653) and Rh. (p= 0.549) (Table 1). (48.4%) of Coeliac and (36%) of control were (Le a+b-). These differences did not reach a statistically significant level. p=0.509. p=0.576. (Table 2A & 2b). 52.9%(9/17) and 41.7% (5/12) of blood group O and A of Coeliac patients respectively were Le (a+b-), 50% of the blood group A Coeliac and controls were Le (a+b+). The prevalence of Le (a+b-) in blood group O in Coeliac was 52.9% and 37.5% in control, these results did not reach a statistically significant differences. p= (0.2922) (Table 3).
Table 1: Patients demographics.
Note: y = years. M =months. *Mann Whiteny u tests and Pearson Chi square corrected with Yates. NS: non-significant.
Table 3: Prevalence of Lewis in blood group O.
Note: Pearson Chi square corrected with yates. NS: nonsignificant.
Discussion
The major human blood group system is ABO and the incidence of ABO groups varies markedly in different races, ethnic groups, and socioeconomic groups in different parts of the world [6]. The blood group O is the most common blood group worldwide. In Libya it ranges from 37.4% in males in Albyda, to 50% in Wadi Alshati, Fezzan province ,and Algabel Algharbi . In our study blood group O accounts for 54.9% of Coeliac and 66.7% of control. Rhve is relatively rare, it accounts for 17% in Britin ,15% in USA, less than 1% in china, Indonesia ,Japan , Korea, native American and india, 9.5% in Moroccans ,8.8% in Saudi Arabia and 7.9% in Egypt [6]. In Libya it was 6.8% in Wadi Alshati, 8.4% in Fezzan province and 12.8% in Algabal Algharbi with the exception in male Libyan from Albyda where it reached up to 16.08% [8-11]. In our study it ranged from 9.7% in Coeliac to 14.8% in control. It was reported that there were various associations between particular ABO phenotypes and an increased susceptibility to disease [12,13]. Type O’s are more prone to ulceration whereas type A’s are prone to cancer and cardiovascular diseases, however the reason for these observations was not known.
The ‘Blood-Type’ diet proposes that lectins , which are sugarbinding proteins found in certain foods ,could cause agglutination if they are not compatible with an individual’s ABO blood group. So, they may experience many health problems. The lectin- connection has been extensively studied in Coeliac disease though the results were mixed and inconclusive [14,15]. A few studies have already examined the association between blood groups and intestinal disorders, but the results were controversial. As early as 1965, a study with 170 patients with Ulcerative Colitis (UC) reported no relation between the ABO system and UC [16]. But there was a strong association between ABO blood groups and intestinal pathogen Helicobacter Pylori infection [17], another study of Colorectal Cancer (CRC) in Turkey has identified a significant association between ABO blood groups and CRC risk [18]. A cohort study in Italy and Belgium found no effect of ABO variants in risk of Crohn’s Disease (CD) but suggest a role for non-O histo-blood groups in developing a structuring or penetrating disease [19]. In our study we found no relation between blood groups, ABO, Rh and susceptibility to Coeliac disease (Table 1).
Secretors usually possess the red cell Lewis phenotype Le (a-b+), conversely non –secretors have Le (a+b-) phenotype as determined by erythrocyte markers. Le (a-b-) may be either secretor or nonsecretors. Le (a+b+) phenotype is transiently observed in infants , secretor activity increases with age ,it was encountered in 16% of Japanese individuals [7], in our study it accounts for 25%, this high results is probably due to small sized sample. Further large scale studies are required to determine the precise size of this group in our population. Coeliac patients with le (a+b-) ( non-secretor) accounts for 48.4% of which 52% blood group O and 41.7% blood group A ,but it did not reach a statistically significant levels from control (Table 2A & 2B) . These results agree with Langman et al study in 1969 (Table 3) [20],who compared the prevalence of nonsecretor among adult patient with Coeliac disease with that of controls, using saliva samples to determine secretor status by the method of Boyd and Shapleig.
They reported that only 14% of 50 patients with Coeliac disease in Birmingham were non- secretor compared with 27% of 92 Coeliac patients in London and 22% of 591 healthy controls and also with Heneghan et al study in 1996 [21] who studied 112 adult Coeliac and 103 control tested for Le(a+b-) using commercially murine anti-lewis “a” and anti-lewis “b” blood grouping reagents ( Organon Teknika Corp. Durham .NC.USA) ,showed no firm relationship between the non-secretor state and Coeliac disease but in contrast to the only study by Dickey. W et al in 1994 [22] who tested 75 adult patients with Coeliac disease ,45 blood donors and 67 staff control for Le (a+b-) (non-secretors) against Le (a-b+) (secretors), by standard haem-agglutination techniques using commercially available anti-Lewis “a” and anti-Lewis “b” blood grouping reagents, they found that non-secretor state is significantly associated with Coeliac disease ,this finding could not be reproduced. Although our sample size was relatively small but we can conclude that neither major blood groups nor Lewis phenotype has any relation to the susceptibility to Coeliac disease in this study. Ending by saying that effectively utilizing genetic information to guide more precise individual nutrition modifications require far more than simply testing major and minor blood groups.
Acknowledgment
The authors express their thanks and gratitude to the staff of the blood bank –Tripoli University Hospital who perform the gel column agglutination tests and to Dr. Abdussalam Hweta for his help in statistical analysis.
References
- Blackwell CC (1989) Genetic susceptibility to infectious agents. Proc R Coll Phys Edinb 19: 129-138.
- Dickey W, Collins JSA, Watson RGP, Sloan JM, Porter KG (1993) Secretor status and helicobacter pylori infection are independent risk factors for Gastro-duodenal disease. Gut 34(3): 351-353.
- Chen YL, Chen JC, Lin TM, Haung TJ, Wang ST (2005) ABO/secretor genetic complex is associated with the susceptibility of childhood asthma in Taiwan. Clin Exp Allergy 35(7): 926-932.
- Falsarella N, Ferreira AI, Nakashima F, deMattos Cde C, de Mattos LC (2011) Evidence of an association between the O blood group and allergic rhinitis. Rev Bras Hematol Hemoter 33(6): 444-448.
- Miao Sy, Zhou W, Chen L, Wang S, Lin XA (2014) Influence of ABO blood group and Rheuses factor on breast cancer risk; a meta-analysis of 9665 breast cancer patients and 244,768 controls. Asia Pac J Clin Oncol 10(2): 101-108.
- Barua S (2002) Human Genetics: An Anthropological Perspective Classique Books. In Barua S (Eds.), Kolkata.
- Rh blood group system.
- Saad KAO (2016) Distribution of ABO Blood Groups and Rhesus Factor (RH) in Albyda /Libya. Journal of Medical and Dental Science Research 3(9): 28-31.
- Altyyar IA, Ali SMK (2017) Distribution of ABO and Rh blood groups in Wadi Alshati, Research gate , Libya. First scientific conference for postgraduate students, At Sebha University.
- Fayrouz IN, Farida N, Irshad AH (2012) Relation between fingerprints and different blood groups. J Forensic Leg Med 19(1):18-21.
- Salih K, Abdrhman OM, Irhuma A, Elgadi B, Abdel Latif MH (2005) Anthropological studies among Libyans of Fazzan Province: ABO and Rh Systems. Sebha University Journal for Medical Sciences 4(1): 64.
- Huston AM, Atmar RL, Graham DY, Estes MK (2002) Norwalk virus infection and disease is associated with ABO histo blood group type. J Infect Dis 185(1): 1335-1337.
- Ewald DS, Sumner CJS (2016) Blood type biochemistry and human disease. Wiley Interdiscip Rev Syst Biol Med 8(6): 517-535.
- Ghazarian H, Idoni B, Oppenheimer SB (2011) A glycobiology review: carbohydrates, lectins and implications in cancer therapeutics. Acta Histochem 113(3): 236-247.
- Wang J, García Bailo B, Nielsen DE, El Sohemy A (2014) ABO genotype, 'blood-type' diet and cardiometabolic risk factors 9(1): e84749.
- Thayer WR, Bove JR (1965) Blood groups and ulcerative colitis. Gastroenterology 48(3): 326-330.
- Boren T, Falk P, Roth KA, Larson G, Normark S (1993) Attachment of Helicobacter pylori to human gastric epithelium mediated by blood group antigens. Science 262(5141): 1892-1895.
- Laryea JA, Siegel E, Burford JM, Klimberg SV (2013) Racial disparity in colorectal cancer: The role of ABO blood group. J Surg Res 183(1): 230-237.
- Forni D, Cleynen I, Ferrante M, Cassinotti A, Caglimi RI, et al. (2014) ABO histo-blood group might modulate predisposition to Crohn’s disease and affect disease behavior. J Crohn's Colitis 8(6): 489-494.
- Langman MJS, Banwell JG, Stewart JS, Robson EB (1969) ABO blood groups, secretor status, and intestinal alkaline phosphatase concentrations in patients with celiac disease. Gastroenterology 57(1): 19-23.
- Heneghan MA, Kearns M, Goulding J, Egan EL (1996) Secretor status and human leucocyte antigens in coeliac disease. Scand J Gastroenterol 31(10): 973-976.
- Dickey W, Wylie JDC (1994) Lewis phenotype, secretor status, and coeliac disease. Gut 35(6): 769-770.

 Review Article
Review Article