Summary
Reverse total shoulder arthroplasty (rTSA) is an expanding operative solution for complex proximal humeral fracture. Vascular thrombosis of the axillar artery is a rare but possible complication concomitant with RTSA. According to our knowledge, this is the first described early acute post-operative axillary artery occlusion after rTSA for proximal humerus fracture dislocation in the elderly. We describe the case of a 79-year-old female with a type 11 C-3 fracture according to the AO/OTA classification who underwent RTSA. Signs of acute ischemia of the left upper limb and axillary nerve stupor were detected clinically in the early post-operative. Prompt vascular surgery operation restored normal peripheral flow. At 1-year follow-up, patient resumed a normal life with complete restoration of circumflex nerve and residual dysesthesia of the median nerve. Probably, the intimal lesion caused by the trauma was worsened by the increased tension on the neurovascular structures during the procedure of fracture reduction and replacement. Moreover, rTSA places brachial plexus and axillary artery under longitudinal strain by lengthening the arm. This case report shows the importance of early clinical follow up after rTSA in displaced proximal humeral dislocated fractures. In these cases, combined vascular and orthopedic surgeons monitoring and careful post-operative physiotherapy is crucial for a good clinical and functional result.
Keywords: Reverse Shoulder Arthoplasty; Proximal Humeral Fracture; Axillary Artery
Introduction
Several studies have reported an overall increase incidence of proximal humeral fractures in the elderly with considerable patient disability and increased public spending [1,2]. Almost 80% of these fractures can be treated nonoperatively, being non or minimally displaced [3]. The gold standard surgical treatment for humeral complex fractures is still controversial. Numerous implants are available, including fixation devices (ORIF) and hemi, total or reverse arthroplasties. Reverse total shoulder arthroplasty (rTSA) was developed for treatment of cuff-tear arthropathy [4,5] but in the last decade has been used as a surgical solution for displaced proximal humeral fractures in the elderly [6]. It is a safe procedure with a very low in-hospital mortality rate [7]. However, many perioperative complications such as hematoma, deep venous thrombosis, cerebrovascular accident, blood transfusion, nerve injuries and postoperative infection [8] has been described. Axillary artery vascular thrombosis following shoulder trauma might be due to acute or iatrogenic, during open reduction techniques, anterior proximal dislocation [9,10]. However, this complication has been rarely described while performing RTSA [11,12]. According to our knowledge, this is the first case report of an early post-operative axillary artery thrombosis after rTSA for proximal humeral fracture in the elderly.
Case Report
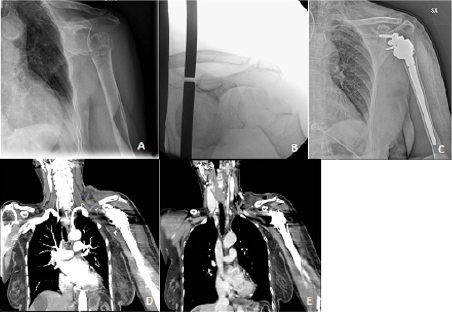
A 79-year-old patient accidentally fell at home tripping over her shoes. She got in our emergency department with pain and functional limitation at her left shoulder. The patient was conscious, oriented with no headache, no nausea, no vomiting, no apparent motor or sensory deficits and valid bilateral radial pulses. Hypertension, vascular encephalopathy, intestinal sub-occlusion, partial nephrectomy and chronic therapy with acetylsalicylic acid (ASA) and atenolol were part of patient’s medical history. Barthel index premorbid was 90/100. Standard radiographs of her left shoulder were performed revealing a displaced, fracture-anteriordislocation of the proximal left humerus, described as type 11 C-3 fracture according to the AO/OTA classification (Figure 1A-1B). After two unsuccessful attempts of closed reduction of the humeral head, a Desault bandage was applied.
The patient was then admitted to our Orthopedic department in order to be treated surgically, with a reverse total shoulder replacement. Pre-operative routine tests and anesthesia evaluation were performed. Surgery was performed under general anesthesia about 30 h after trauma, through a lateral trans-deltoid approach in a beach chair position. After appropriate fracture site exposing, antero-inferior dislocation of the humeral head was found, medially to the coracoid and in contact with the brachial plexus. The transdeltoid approach not enabling the humeral head to me removed easily, caused a greater medial dislocation of the bone fragment. After several attempts the humeral head was removed and a Lima SMR Reverse Shoulder Prosthesis (Villanova di San Daniele del Friuli, Udine) was implanted (Figure 1C). The duration of the operation was 2 hours ad no significant intraoperative blood loss was detected. At the end of the procedure, arm sling was positioned at 15° of abduction.
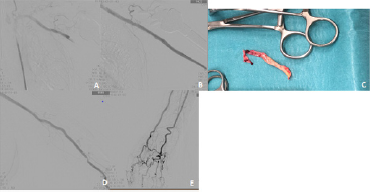
Signs of acute ischemia of the left upper limb and axillary nerve stupor were detected clinically approximately 2 hours after surgery. The Patient reported pain, paraesthesia and functional limitation of the wrist and fingers with absence of peripheral arterial pulses. Urgent vascular surgery evaluation was requested: the duplex-ultrasound revealed patency of the subclavian artery up to the distal third but absence of flow within the axillary, humeral, radial and ulnar arteries. A CT angiography of the left upper limb (Figure 1 D-E) confirmed occlusion of the axillary artery at the origin, without opacification of the downstream vessels. After 5 hours from the diagnosis of left upper limb ischemia and under general anaesthesia, vascular surgeons performed an angiography with percutaneous left femoral access. Due to lack of visualization of downstream vessels, occlusion of the first tract of the axillary artery was diagnosed (Figure 2A). Angioplasty and stenting of the left axillar artery restored blood flow to the downstream vessels though appearing to be diffusely thrombosed and demanding for an open surgery (Figure 2B).
The non-pulsatile humeral artery was isolated and thromboembolectomy was carried out with removal of the tunica intima damaged and fresh thrombus (Figure 2C) until direct flow was restored. At the end of the procedure, angiography showed patency of the subclavian-axillar-humeral axis with significant stenosis at the level of the arterial suture (Figure 2D) which was therefore revised with the interposition of patches from ipsilateral basilica vein. Echo duplex ultrasound showed pulsating humeral artery with peripheral blood flow confirmed by angiography (Figure 2E). The procedure lasted 2 hours and 20 minutes. Upon awakening, the patient was admitted initially to the Intensive Care Unit for post-operative monitoring and then hospitalized in the Vascular Surgery’s ward. Despite persisting weakness of the entire upper limb and dysethesia of the first, second and third finger, the patient showed progressive reduction of paresthesia, complete regression of pain and partial resumption of wrist and hand sensitivity and mobility.
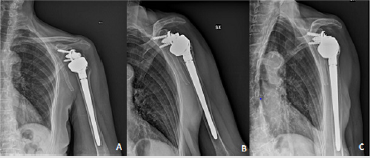
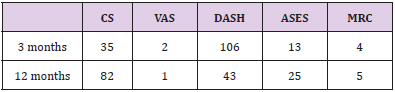
The patient was discharged from the hospital in stable conditions on the fourth post-operative day with appropriate antiplatelet therapy prescription. After 1 month the patient removed the arm sling with chest strap and begun standard shoulder rehabilitation protocol. The patient was called for clinical (using the Constant Score, DASH, MRC scale and VAS) and radiological follow up at 3 and 12 months (Table 1). The 6-month follow-up visit was not performed because of SARS-Cov2 lockdown. No scapular notching or tuberosity reabsorption were recorded clinically and radiographically (Figure 3A-3B-3C). The patient resumed a normal life with a sharp increase in Constant score and DASH values and complete resolution of pain (VAS) at 1 year follow up. Despite physiotherapy was interrupted due to the SARSCov2 Italian lockdown, the patient kept on doing home exercises resulting in an excellent recovery of strength as proved by MRC evaluation.
Electromyography of the upper limb, vascular examinations and duplex-ultrasounds were carried out during the follow up. The patient showed progressive improvement in terms of upper limb sensitivity, strength and functionality with complete restoration of circumflex nerve conduction, but residual dysesthesia persisted in the territory innervated by the median nerve. Vascular follow-ups reported normal peripheral flow and no signs of stent stenosis.
Discussion
Reverse total shoulder arthroplasty (RTSA) has been increasingly carried out during the past decade, and it is now widely preferred for treating displaced proximal humeral fractures in the elderly [6]. Furthermore, a recent multicentre randomized controlled trial has showed better clinical outcomes with rTSA than ORIF in the treatment of complex proximal humeral fractures of the elderly at a 2-year follow-up [13]. However, whatever type of surgery performed, leads to stress and damage to the shoulder periarticular structures. The increase of tension, compression and shear forces to a vessel might develop an innermost layer damage with further thrombosis obstructing the blood flow. In our case, the innermost layer damage could have been caused both by the trauma itself with the dislocated humeral fractures and the type of surgical approach carried out. The lateral trans-deltoid approach does not allow the surgeon to work easily on shoulder intraarticular medial structures.
The prolonged attempts of humeral proximal fragment reduction displaced it more medially, increasing the stress on the neurovascular bundle. Moreover, the rTSA biomechanics, distalizing the humerus, places the brachial plexus and axillary artery under longitudinal strain. All these factors could have lead to early post-operative vascular obstruction with acute signs of ischemia. The ischemia tissue damage correlates to the restriction of blood supply duration. As the time elapsed between the vascular injury and the reperfusion was less than 4 hours, there was no impairment of the limb strength, appearing fully recovered at 1 year. Furthermore no signs of prosthetic implant mobilization and chronic pain were shown. The occurrence of nerve complications following rTSA, relates to direct nerve damage, indirect traction, compression secondary to retractors use and post-operative hematoma formation [14]. Isolated axillary nerve stupor [15]. as well as persisting residual dysesthesia in the territory innervated by the median nerve, produced by an injury of the upper sensitive trunk have been described [16].
Conclusion
This early acute post-operative event of axillary thrombosis was correctly managed with the following vascular surgery procedure. Furthermore, satisfactory long-term radiographic and clinical follow-up outcomes, without further complications, were obtained. Care has to be given to early post-operative clinical evaluation after rTSA in displaced proximal humeral dislocated fractures, looking for trauma related or iatrogenic neurovascular damages. Posttraumatic injuries of the vessel innermost layer are fearful and unpredictable complications. A careful pre-operative planning, primarily focusing on both the choice of the surgical approach used and peripheral vascular status, is also fundamental while treating proximal humeral dislocated fractured with a reverse total shoulder prosthesis. Furthermore, careful post-operative physical therapy is important for a good clinical and functional outcomes as shown in this report. Further investigations of the incidence of arterial and deep vein thrombosis after rTSA for proximal humeral fractures might be helpful to evaluate also the benefits of prophylactic anticoagulant therapy in order to avoid the complication described.
References
- Palvanen M, Kannus P, Niemi S, Parkkari J (2006) Update in the epidemiology of proximal humeral fractures. Clin Orthop Relat Res 442: 87-92.
- Lippuner K, Popp AW, Schwab P, Gitlin M, Schaufler T, et al. (2011) Fracture hospitalizations between years 2000 and 2007 in Switzerland: a trend analysis. Osteoporos Int 22(9): 2487-2497.
- Iyengar JJ, Devcic Z, Sproul RC, Feeley BT (2011) Nonoperative treatment of proximal humerus fractures: a systematic review. J Orthop Trauma 25(10): 612-617.
- Franceschetti E, de Sanctis EG, Ranieri R, Palumbo A, Paciotti M, et al. (2019) The role of the subscapularis tendon in a lateralized reverse total shoulder arthroplasty: repair versus nonrepair. Int Orthop 43(11): 2579-2586.
- Franceschetti E, Ranieri R, Giovanetti de Sanctis E, Palumbo A, Franceschi F (2020) Clinical results of bony increased-offset reverse shoulder arthroplasty (BIO-RSA) associated with an onlay 145 degrees curved stem in patients with cuff tear arthropathy: a comparative study. J Shoulder Elbow Surg 29(1): 58-67.
- Savin DD, Zamfirova I, Iannotti J, Goldberg BA, Youderian AR (2016) Survey study suggests that reverse total shoulder arthroplasty is becoming the treatment of choice for four-part fractures of the humeral head in the elderly. Int Orthop 40(9): 1919-1925.
- McCormick F, Nwachukwu BU, Kiriakopoulos EB, Schairer WW, Provencher MT, et al. (2015) In-hospital mortality risk for total shoulder arthroplasty: A comprehensive review of the medicare database from 2005 to 2011. Int J Shoulder Surg 9(4): 110-113.
- Klug A, Wincheringer D, Harth J, Schmidt-Horlohe K, Hoffmann R, et al. (2019) Complications after surgical treatment of proximal humerus fractures in the elderly-an analysis of complication patterns and risk factors for reverse shoulder arthroplasty and angular-stable plating. J Shoulder Elbow Surg 28(9): 1674-1684.
- Rangdal SS, Kantharajanna SB, Daljit S, Bachhal V, Raj N, et al. (2012) Axillary artery thrombosis with anteroinferior shoulder dislocation: a rare case report and review of literature. Chin J Traumatol 15(4): 244-248
- Gallucci G, Ranalletta M, Gallucci J, De Carli P, Maignon G (2007) Late onset of axillary artery thrombosis after a nondisplaced humeral neck fracture: a case report. J Shoulder Elbow Surg 16(2): e7-8.
- Ghanem OM, Sacco J, Heitmiller RF, Gashti SM (2016) Delayed Axillary Artery Occlusion after Reverse Total Shoulder Arthroplasty. Case Rep Orthop 2016: 5463514.
- Wilkerson J, Napierala M, Shalhub S, Warme WJ (2019) Axillary artery intimal dissection with thrombosis and brachial plexus injury after reversing total shoulder arthroplasty. Journal of Shoulder and Elbow Surgery 28(12): e393-e397.
- Fraser AN, Bjørdal J, Wagle TM, Karlberg AC, Lien OA, et al. (2020) Reverse Shoulder Arthroplasty Is Superior to Plate Fixation at 2 Years for Displaced Proximal Humeral Fractures in the Elderly: A Multicenter Randomized Controlled Trial. J Bone Joint Surg Am 102(6): 477-485.
- Ball CM (2017) Neurologic complications of shoulder joint replacement. J Shoulder Elbow Surg 26 (12): 2125-2132.
- LiBrizzi CL, Rojas J, Joseph J, Bitzer A, McFarland EG (2019) Incidence of clinically evident isolated axillary nerve injury in 869 primary anatomic and reverse total shoulder arthroplasties without routine identification of the axillary nerve. JSES Open Access 3(1): 48-53.
- See RH, Katirji B, Preston D, Shapiro B (2015) Mechanism for Proximal Median Neuropathy as a Complication of Reverse Shoulder Arthroplasty: Nerve Strain Calculated from a Computerized 3-D model Cadaver Brachial Plexus (P2.016). Neurology 84 (14 Supplement): P2.016

 Case Report
Case Report