Abstract
Objective: To compile the current knowledge of the surgical approach performed in the treatment of scoliosis in Ehlers-Danlos patients.
Summary of Background Data: Ehlers-Danlos syndrome (EDS) has a low incidence in the population and is often associated with the development of scoliosis during the growth. Few articles are reported in the literature describing the effectiveness and the risks associated with the surgical treatment of scoliosis in EDS patients. Such approach has been shown to increase life expectancy but is largely controversial because of the high rate of complications and morbidity. Due to the lack of knowledge about this disease, appropriate recommendations are needed to propose an efficient approach for this kind of surgery.
Methods: A literature search was conducted using PubMed (MEDLINE) database. The Medical Subject Headings keywords used in this research were “Ehlers-Danlos syndrome” associated with a combination of the following terms “spine”, “scoliosis” or “ktphoscoliosis”, “spinal fusion”, ‘spinal surgery”, “surgery”. Articles reporting the surgical management of scoliosis in EDS patients and the associated were selected and analyzed individually.
Results: On 10 articles reviewed, 9 were mentioning surgical complications. These articles were about 41 patients. Orthopedic treatment has failed, with a rapid degradation of scoliosis in puberty in all cases. A stable arthrodesis has been achieved in 35 of 41 patients, which represents a rate of surgical success of 90%. Vascular lesions occurred in 13 of 41 patients (33%). Paraplegia occurred in 5 patients, which represents 12%. There has been high rate of blood loss in every surgery performed, with an average of 3101 mL.
Conclusion: Surgery of scoliosis in EDS patients gives encouraged results, with a good correction of deformity and a stable fusion. However, it presents a high risk of neurological and vascular complications. Some precautions are mandatory for the surgery.
Keywords: Ehlers-Danlos Syndrome; Scoliosis; Surgical Procedure; Spine
Introduction
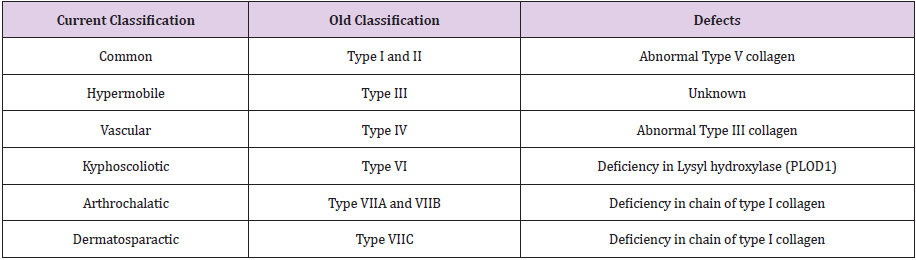
Ehlers-Danlos syndrome (EDS) is an uncommon genetic disease affecting the connective tissue during the growth and is related to a wide range of complications. EDS patients are characterized by a high degree of skin hyperextensibility associated with joint hypermobility and various vascular disorders. During the childhood, EDS patients are mainly susceptible to develop a severe spinal deformity such as progressive kyphoscoliosis, one of the most observable musculoskeletal disorder associated with this disease. Historically, first cases of patients with joint hyperlaxity and scares defects were described by Hippocrates in 400 BC. In the 1660s, other cases of patients with skin hyperextensibility and abnormal flexibility were presented byJob Janszoon van Meek’ren to the Leyde Academy. Before and during the late nineteenth century, many cases of patients with such cutaneous and musculoskeletal features were observed and considered as performers around the world [1]. In the 20th century, 2 physicians, Danish dermatologist Edward Lauritz Ehlers, and French dermatologist Henri-Alexandre Danlos, were the first to officially describe and publish a review of patients presenting skin hyperextensibility, joints laxity and skin fragility. As an evidence, the syndrome was rapidly named Ehlers- Danlos Syndrome by the scientific society. Many groups of patients were then observed and categorized depending on the severity of their joints mobility, skin laxity and musculoskeletal conditions. Classification of EDS syndrome was proposed in the 1960s with nine subcategories. Since 1997 the new nosology of Villefranche distinguishes 6 types of EDS presented in (Table 1) [2].
EDS Type VI referred as the kyphoscoliotic form which is related to an autosomal recessive form of lysyl hydroxylase-1 deficiency involved in the stabilization of collagen. PLOD1 gene mutation coding for lysyl hydroxylase 1 is then responsible of the abnormal production of rich-collagen tissues such as ligaments, skin, joints and vessels. This molecular collagen disorder can lead to several symptoms like cutaneous and articular hyperlaxity, muscular hypotonia in newborns, fragility of the cornea. EDS Type VI is also the most interesting form for orthopedic surgeons due to the development of a severe spinal deformity beginning in utero or in the first years of life. Typically, spinal disease corresponds to a scoliosis or a kyphoscoliosis in both thoracic and lumbar spine. The progression of this kind of deformity is rapid in EDS patients with a high rate of respiratory and vascular complications (breaking of small and medium vessels) confirming the need of a surgical therapy [3]. Surgical treatment of scoliosis in non-EDS patients often consists in a posterior elective thoracolumbar arthrodesis associated with a vertebral derotation. However such technical approach performed to treat idiopathic scoliosis has to be reconsidered for EDS patients. Cautions have to be taken regarding the reduction of scoliosis observed in EDS patient type VI due to tissues abnormalities and musculoskeletal conditions. Otherwise a large range of severe or irreversible complications could be developed postoperatively [4-6]. Up to date, few publications have been published regarding the surgical treatment used for scoliosis in patients with EDS. There is a lack of recommendations on the surgical approach that should be performed in these cases and when it should be done, even if it has clearly been shown that surgery potentially increases life expectancy in EDS patients. The aim of this literature review is to summarize all the relevant publications about the surgical management of scoliosis in EDS patients. Complications related to the surgical procedure performed to treat such spinal deformity in patients with some connective tissues disorders are also presented in this article.
Methods
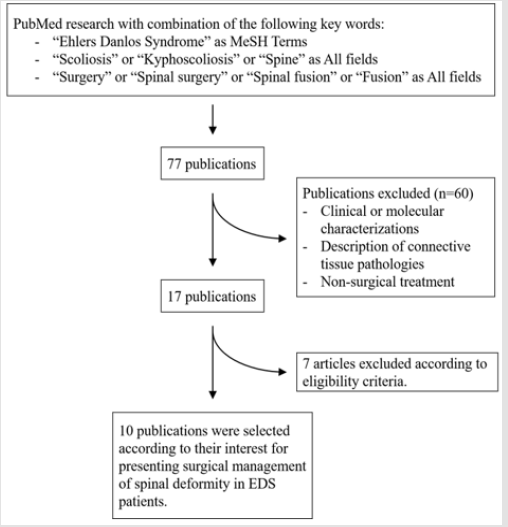
A literature review using the Pubmed database was performed using a combination of the following formula: ((Ehlers Danlos syndrome[MeSH Terms]) AND Scoliosis) AND Surgery; ((Ehlers Danlos Syndrome[MeSH Terms]) AND Scoliosis) AND Spinal surgery; ((Ehlers Danlos syndrome[MeSH Terms]) AND Scoliosis) AND Spinal fusion; (Ehlers Danlos syndrome[MeSH Terms]) AND Spinal fusion; (Ehlers Danlos syndrome[MeSH Terms]) AND Spinal surgery; ((Ehlers Danlos syndrome[MeSH Terms]) AND Spine) AND Surgery; ((Ehlers Danlos syndrome[MeSH Terms]) AND Spine) AND Fusion; ((Ehlers Danlos syndrome[MeSH Terms]) AND Kyphoscoliosis) AND Surgery; ((Ehlers Danlos syndrome[MeSH Terms]) AND Kyphoscoliosis) AND Spinal Fusion. A total of 77 publications were found according to the above criteria. After excluding molecular and genetic-related publications, 37 articles were selected. After internal peer review with all authors of this article and additional research including citation tracking associated with the surgical management of spinal deformity in EDS patients, only 10 articles of interest were finally selected (Figure 1).
Results
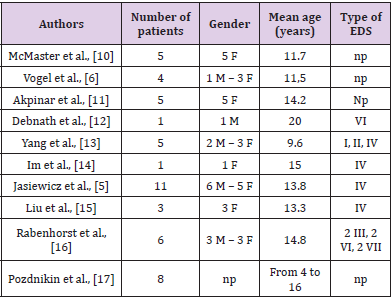
According to our research criteria only 10 articles published within the last 20 years reporting the surgical management of spinal deformities in EDS patients were selected. Most of these publications refer to complications associated with the surgical treatment of kyphoscoliosis in EDS patients (n = 9) and report 41 cases of operated patients. The mean age of the global population was 13 years old with respectively 13 males and 28 females (Table 2). Ehlers-Danlos syndrome has a low prevalence (from 1 to 9 cases per 100 000 newborns) making it a rare disease and limits the number of reported cases. Therefore few articles have been written about spinal arthrodesis in scoliotic EDS patients . In 1969, a cohort of 100 EDS patients with a severe spinal deformity was presented by P. Beighton et al. Among 18 scoliotic subjects observed in this population, only 6 of them reported back pains [7]. Surgical treatment of EDS patients is recognized to be related to the type of the disease. EDS type IV and VII patients have a high rate of non-healing wounds, hematoma and infections, in relation with capillary fragility whereas bone consolidation is not modified by the disease [8]. Then surgical treatment of scoliotic patients with EDS is a real challenge according to the rate of complications and the benefits of the surgery. Natajaran et al. demonstrated that the natural development of a scoliosis in an EDS patient and its progression curve progressed rapidly (leading to early respiratory complications, muscular and articular hypotonia during the puberty period), unless an appropriate surgical treatment is realized.
Then it was highly recommended to closely follow-up EDS patients presenting a spinal deformity and to set up an appropriate management of the disease to avoid fatal morbidities [9]. One of the best solution to stabilize the progression of the scoliosis should be to propose a surgical treatment to the patient in order to decrease the potential risk of scoliosis-related complications. On the contrary, considering the high rate of bleedings and wound healing disorders, Leatherman and Dickson have published that surgery has to be avoid in EDS patients with no evidence of that. Nowadays, there are no recommendations on the need or the time when the surgery should be performed, but it has been clearly demonstrated that it increases life expectancy in EDS patients.
Efficacy of Surgical Treatment
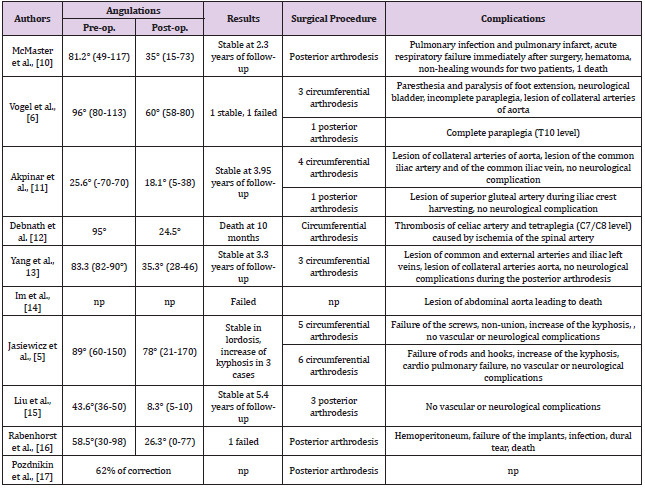
In this literature review, most of the patients had an orthopedic treatment during childhood, at the time when they started walking. This treatment consisted in wearing a brace or traction. For each case, this treatment has failed with a rapid progression of scoliosis during the puberty period requiring a surgical approach. Then a stable arthrodesis has been achieved in 35 of 39 patients, which represents a rate of surgical success of 90% with an improvement of sagittal and coronal parameters of 57.7% (Table 3) [5,6,10-17].
Vascular Complications
Vascular fragility is a part of EDS and is critical for the prognostic of this disease: EDS patients have a high risk of spontaneous breaking of medium and large vessels due to an abnormal type III collagen (different from Marfan’s syndrome) which is the most important constituent part of vessels wall. Iatrogenic vascular wall injury seems to be unavoidable, and more difficult to manage in a lumbar anterior approach. In this review, vascular injuries occurred in 13 of 39 patients (33%): superficial hematoma, tears in aorta, iliac arteries, thrombosis of coeliac artery, hemoperitoneum (Table 3).
Neurological Complications
Literature suggests that EDS patients have a higher risk of neurological complications. Given the few cases reported, the rate of such complications is difficult to evaluate even if it seems to be higher than 0,7% of the iatrogenic paralysis in classic scoliosis surgery in the global population. Paraplegia occurred in 5 patients, which represents 12% of the population (Table 3). Vogel et al. suggests that type IV EDS patients have a higher risk to develop several neurological complications due to the laxity of bones and muscles, which allows a higher correction of deformation, more than the vascular and neurologic tissue can support [6]. It is also supposed that EDS patients have a higher risk of scoliosis angulation than the other scoliotic patients, which induces a higher risk of neurological complications.
Choice of Surgical Approach and Technique
In non-EDS patients, lumbar anterior approach has a low risk of vascular complications. But due to vessels fragility, EDS patients are often exposed to vascular injuries. Yang et al. have described a high risk of injuries of the common iliac and extern iliac arteries and veins, and lesion of segmentary arteries of the abdominal aorta using this approach which has higher vascular risks than posterior surgical procedures. But the posterior approach have a higher neurological risk. Yang et al. suggest that the posterior approach is sufficient to treat scoliotic EDS patients [13]. However, Rabenhorst et al. have experimented vascular complications in their 6 patientscohort treated by the posterior approach [16].
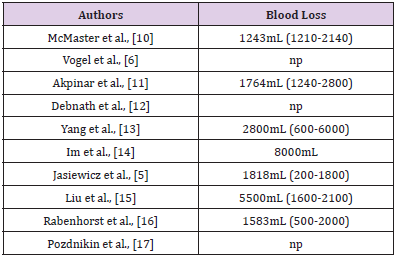
Blood Loss
According to the different approaches and the type of surgery performed, blood loss is a major risk of complication for EDS patients. An average of 3101mL was reported in this literature review, despite every precautions taken by the operators to limit bleeding. However, authors mentioned that blood loss were properly managed in all surgical procedure (Table 4).
Discussion
Cases reported in the literature demonstrated how scoliotic EDS patients are difficult to treat due to the comorbidities related to the rapid progression of scoliosis and the surgical complications of the proposed procedure. There is no recommendations for the surgical management of EDS patients. It is highly recommended to closely follow-up the progression of the scoliosis during the first years of life. A surgical approach have to be considered when scoliotic angulation is too important to be supported by conventional methods. However, according to the previous procedures reported in the literature, some precautions have to be taken before and during the surgical procedure. Before the surgery, it is first mandatory to prescribe a complete preoperative evaluation to properly diagnose the type of EDS since the surgical approach will depends on the type of the disease. MRI and angiography are highly recommended for patients with vascular abnormalities in order to avoid per-operative pitfalls. Even for non-symptomatic patients, neuro-imaging will be helpful to detect preoperative spinal cord lesions which are mainly observed in patients with an important spinal deformity. In this case, a complete neurological evaluation including vesical and sphincters functions has to be performed by a neurologist before the surgery.
All of these steps allow the surgeon to plan the surgery in good circumstances and decrease the frequency of post-operative complications. During the surgical procedure, it is mandatory to consider muscles and articular hyperlaxity in order to reduce the spinal deformity but to not correct the entire scoliotic angulation. This steps is critical to avoid the development of severe neurological complications. Yang et al. conclude that the postoperative correction must be inferior to 50% of the correction obtained on preoperative bending X-rays [13]. Moreover, if needed, it is highly recommended to perform the discectomy carefully to avoid vascular structures. The procedure should not be as extensive as performed in the case of classic surgery. During the surgical procedure, a perfect management of the blood pressure have to be maintained to minimize blood loss. A lower pressure is recommended taking care of spinal cord ischemia in case of too low pressure. Electrostimulation is also a good way to decrease the risk of peroperative bleeding. In the lumbar region, segmentary vessels have to be precisely and carefully isolated and coagulated as far as possible from the aorta, which is the opposite of the conventional technique for scoliosis. In addition, to decrease the risk of blood complications, it is not recommended to perform a local injection of distilled adrenalin (1:400000), VIIa factor or desmopressin acetate. Even if some authors proposed the use of such products, it can easily lead to thrombosis during the surgical procedure and increase the risk of vascular complications. In terms of manipulations, before and during the surgery, some authors advised to perform a head traction before or after the surgery. According to the literature, no contraindication were found if these manipulations are only realized very carefully and taking care to the risk of lesion of brachial plexus.
Conclusion
Spinal surgery for scoliotic EDS patients demonstrated good clinical results, with a good correction of deformity and a stable fusion. This is supposed to be a best way to extant the quality of life of EDS patients. However, this kind of treatment presents a high risk of neurological and vascular injuries. Some precautions are mandatory before this surgery
Conflict of Interest
The authors declare that they have no conflict interests.
Funding
The authors declare that no funding or fees were received to conduct this study.
References
- LA Parapia, C Jackson (2008) Ehlers-Danlos syndrome - A historical review. Br J Haematol 141(1): 32-35.
- P Beighton, A De Paepe, B Steinmann, P Tsipouras, RJ Wenstrup (1997) Ehlers-Danlos Syndromes : Revised Nosology, Villefranche. Am J Med Genet 77(1): 31-37.
- HN Yeowell, B Steinmann (2000) Ehlers-Danlos Syndrome, Kyphoscoliotic Form. In GeneReviews: 342-349.
- A Busch, Julia Suellner, Friedrich Anger, Michael Meir (2014) Critical care of kyphoscoliotic type Ehlers-Danlos syndrome with recurrent vascular emergencies. Vasa 43(3): 216-221.
- B Jasiewicz, T Potaczek, M Tesiorowski, K Lokas (2010) Spine deformities in patients with Ehlers-Danlos syndrome, type IV - late results of surgical treatment. Scoliosis 5(1): 26.
- LC Vogel, JP Lubicky (1996) Neurologic and Vascular Complications of Scoliosis Surgery in Patients with Ehlers-Danlos Syndrome: A Case Report. Spine (Phila. Pa. 1976) 21(21): 2508-2514.
- P Beighton, F Horan (1969) Orthopaedic aspects of the Ehlers-Danslos Syndrome. J Bone Jt Surg Br 51(3): 444-453.
- P Beighton, FT Horan (1969) Surgical aspects of the Ehlers-Danlos Syndrome. A survey of 100 cases 56(4): 255-259.
- D Natarajan, D Samartzis, YW Wong, KDK Luk, KMC Cheung (2011) Natural history of spinal deformity in a patient with Ehlers-Danlos syndrome: case report with 20-year follow-up. Spine J 11(7): e1-e4.
- M Mc Master (2018) Spinal deformity in Ehlers-Danlos syndrome. Five patients treated by spinal fusion. J Bone Joint Surg Br 76(5): 773-777.
- S Akpinar, Abdullah Gogus, Ufuk Talu, Azmi Hamzaoglu (2003) Surgical management of the spinal deformity in Ehlers-Danlos syndrome type VI. Eur Spine J 12(2): 135-140.
- UK Debnath, H Sharma, D Roberts, N Kumar, S Ahuja (2007) Coeliac axis thrombosis after surgical correction of spinal deformity in type VI Ehlers-Danlos syndrome: A case report and review of the literature. Spine 32(18): E528-531.
- JS Yang, PD Sponseller, M Yazici, CE Johnston (2009) Vascular complications from anterior spine surgery in three patients with ehlers-danlos syndrome. Spine 34(4): E153-177.
- JS Im, YH Lim, JS Park, SS Lee, KM Kim (2010) Rupture of abdominal aortic aneurysm after spine surgery in the patient with Ehlers-Danlos syndrome -A case report. Korean J Anesthesiol 58(6): 555-559.
- Y Liu, R Gao, X Zhou, W Yuan (2011) Posterior Spinal Fusion for Scoliosis in Ehlers-Danlos Syndrome, Kyphoscoliosis Type. Orthopedics 34(6): 228.
- BM Rabenhorst, S Garg, JA Herring (2012) Posterior spinal fusion in patients with Ehlers-Danlos syndrome: A report of six cases. J Child Orthop 6(2): 131-136.
- II Pozdnikin, IP Ryzhakov (1990) Kyphotic-scoliotic deformities of the spine in children and adolescents with Ehlers-Danlos syndrome and their treatment]. Ortop Travmatol Protez 11: 5-10.

 Research Article
Research Article