Abstract
Esophageal perforation (EP) remains a life-threatening condition despite the progress in modern medicine. Morbidity and mortality rates are still high especially in delayed diagnosed cases. Interventional gastroenterology is an alternative to high-risk surgical procedures and offers satisfactory results especially in elder and comorbid patients. We report such a case of a late clinical presentation of complicated spontaneous EP treated by a combination of two OTSCs and a SEMS in order to close the defect.
Keywords: Esophageal Perforation; Boerhaave’s Syndrome; Interventional Endoscopy
Introduction
Esophageal perforation (EP) remains a life-threatening condition despite the advancements of surgery, interventional gastroenterology and intensive care medicine. The most common causal factor is Iatrogenic - upper GI endoscopy, nasogastric tube insertion, surgery, endotracheal intubation, etc. [1]. A transmural EP may also occur after excessive vomiting. Such a “spontaneous” perforation is known as Boerhaave’s syndrome as first described by Dr. Herman Boerhaave in 1724 [2]. EP is associated with high mortality rate reaching 10% for all cases and even 50% when the diagnostics have been delayed [3]. The treatment scheme consists of patient resuscitation and broad-spectrum antibiotics followed by surgical repair [4]. Surgery on its turn is associated with high morbidity and mortality as well as prolonged hospital stay. Recent progress in interventional endoscopy introduced minimally invasive approaches - over-the-scope clips, stenting, endoscopic suturing devices, etc. [4-9].
Case Presentation
A 71 -year old man was admitted to the surgical department
of another hospital with deteriorating clinical condition, chest pain
and fever. The patient reported severe vomiting 2 weeks before
admission, but there was no subcutaneous emphysema as one of
the features in the classic Mackler’s triad. Thoracic X-ray discovered
massive right pleural effusion and CT-scan confirmed right pleural
empyema. Thoracotomy achieved empyema evacuation and pleural
space debriding, but the patient condition did not improve. Gastric
content was secreted from the pleural drainages on 3. Day after
surgery. A follow-up CT-scan suspected EP since it discovered a
contrast leakage. The patient was referred to our institution for
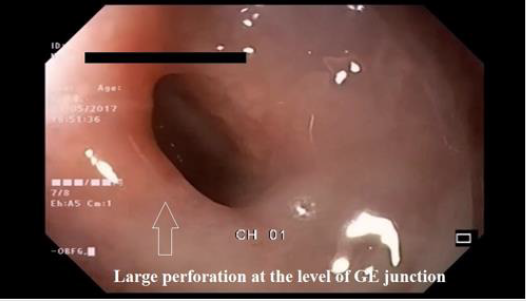
further treatment. An upper endoscopy documented a complete wall
laceration measured 25/10 mm with tight edges and granulations
at the esophagogastric junction (Figure 1). The CT scan found a
distal EP as the contrasting substance leaked in the right pleural cavity. OTSC /Ovesco, Tubingen, Germany/ placement was the first
method of choice attempting to close the defect. The perforation
was too large and a single OTSC did not achieve a satisfactory result.
This necessitated an additional second clip that managed a
successful complete defect closure (Figure 2). A gastrografin study
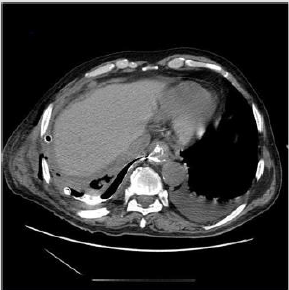
right after the procedure revealed no leakage. However, a control CTscan
on 8. Day after the procedure (oral contrast in-take) showed a
low debit persisting leakage at the level of the clips into the pleural
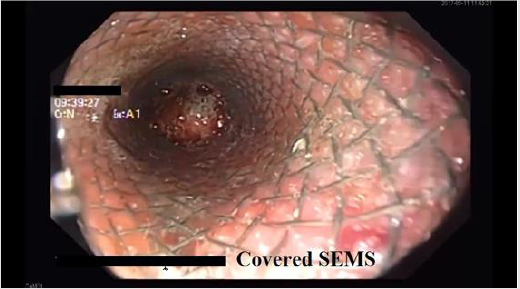
cavity (Figure 3). Second endoscopy was performed confirming
a small defect between the two OTSCs. (Figure 4). A covered selfexpandible
metal stent /Wallstent; Boston Scientific, Marlborough,
Massachusetts, USA/ was placed at the clips level (Figure 5). A
follow-up gastrografin study showed no contrast leakage. The
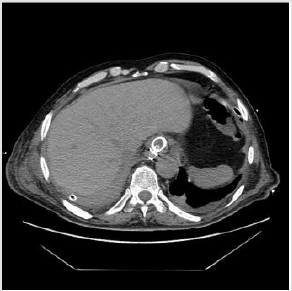
patient condition rapidly improved. Follow up CT scan on 13. Day
showed almost complete resolution of the pleural effusion. The
patient started oral in-take on 14. Day and was discharged on 18.
Day. Due to severe comorbidities /COPD, HCV liver cirrhosis/ we
decided not to remove the esophageal SEMS. Follow up chest X-ray
and esophagogram 2 months later did not show any pathologic
findings.
Figure 3: CT- scan with peroral contrast showing small leak at the level of the clips into the right pleural cavity.
Figure 5: Follow up CT-scan on the 13th day showing almost complete resolution of the pleural effusion.
Discussion
EP is a dramatic emergency with poor prognosis, especially in cases of delayed diagnosis. Surgery in these cases is related with high morbidity and mortality especially in elderly and multimorbid patients. Endoscopic treatment is a suitable option for early recognized perforations [6-9]. The case is unusual because of the late presentation of complicated spontaneous perforation of the esophagogastric junction of an elderly multimorbid patient. We used a combination of two OTSCs and a SEMS in order to close the defect. A single clip was not sufficient to close the ruptured area, so we used a second one achieving complete closure. Due to the severe inflammation and the rigidity of tissues there was a minor persistent defect between the two clips, successfully managed with the SEMS. We also believe that we reduced the risk of SEMS migration causing stenosis by the two OTSC.
References
- Maurya VK, Sharma P, Ravikumar R, Bhatia M (2016) Boerhaave's syndrome. Med J Armed Forces India 72(Suppl 1): S105-S107.
- Adams BD, Sebastian BM, Carter J (2006) Honoring the Admiral: Boerhaave-van Wassenaer's syndrome. Dis Esophagus 19(3): 146-151.
- Klin B, Berlatzky Y, Uretzky G (1989) Boerhaave's syndrome: case report and review of the literature. Isr J Med Sci 25(2): 113-115.
- White RK, Morris DM (1992) Diagnosis and management of esophageal perforations. Am Surg 58(2): 112-119.
- Costamagna G, Marchese M (2010) Management of esophageal perforation after therapeutic endoscopy. Gastroenterol Hepatol (NY) 6(6): 391-392.
- Li Y, Wu J, Meng Y, Zhang Q, Gong W, et al. (2016) New devices and techniques for endoscopic closure of gas- trointestinal perforations. World J Gastroenterol 22(33): 7453-7462.
- Paspatis G, Dumonceau JM, Barthet M, Meisner S, Repici A, et al. (2014) Diagnosis and management of iatrogenic endoscopic perforations: European Society of Gastrointestinal Endoscopy (ESGE) Position Statement. Endoscopy 46(8): 693-711.
- Van Boeckel PGA, Dua KS, Weusten BALM, Schmits RJH, Surapaneni N, et al. (2012) Fully covered self-expandable metal stents (SEMS), partially covered SEMS and self-expandable plastic stents for the treatment of benign esophageal ruptures and anastomotic leaks. BMC Gastroenterol 12: 19.
- Ono H, Tanaka M, Takizawa K, Kakushima N, Kawata N, et al. (2015) Utility of the over-the-scope-clip system for treating a large esophageal perforation. Esophagus 12(3): 336-339.

 Case Report
Case Report