Abstract
Background: Information on causes of death (CoD) is very poor in sub-Saharan Africa, although it provides vital information for planning health strategies. We aimed to analyze the CoD in a large series of autopsies conducted in Mozambique during one-year period.
Methods: All adult autopsies conducted at the Maputo Central Hospital (Mozambique) from January,1st to December 31st 2013 (12 month-long period) were analyzed, according to HIV status. Maternal and traumatic deaths were excluded from the study.
Results: Four hundred and forty-nine adult autopsies were performed (52% males, median age 42 years, range 15-93). HIV-positive patients comprised 37% (166), 19% (87) were HIV-negative, and in 44% (196) information on HIV status was unavailable. Infectious diseases were the leading CoD (249; 55%), followed by malignancies (76; 17%), cardiovascular (75;17%), other non-infectious diseases (46;10%), and nonconclusive CoD (3;1%). Infectious diseases were responsible for 64%, 51% and 50% of HIV-positive, -negative and -unknown patients, respectively. Tuberculosis was the leading infectious CoD, regardless of HIV status. Other common infections included pyogenic meningitis (42; 17%) and pneumonia (37;15%). Non-infectious cardiovascular diseases and malignancies comprised 33% of all CoD in HIV-negative, and 15% in HIV-positive patients.
Conclusion: The burden of infectious diseases, particularly of tuberculosis, remains high in Mozambique, even in HIV-negative patients. Apart from tuberculosis, pyogenic infections of the central nervous system and respiratory tract are also frequent and thus require introduction of new point-of-care tests and improvement of treatment strategies. Non-communicable conditions, mainly cardiovascular and oncologic diseases are becoming prevalent in Mozambique.
Keywords: Autopsy; Communicable Diseases; HIV; Cause of Death; Mozambique; Tuberculosis
Abbreviations: CoD: Cause of Death; LMIC: Low- and -Middle Income Countries; MCH: Maputo Central Hospital
Introduction
Many low- and middle-income countries (LMIC) face important challenges in maintaining reliable information on cause of death (CoD) due to the poor quality of their vital statistics and death registration systems [1]. Most of the scant information available in these countries is based on verbal autopsy and clinical records, two methods with important drawbacks due to the overlapping symptoms of many conditions, particularly of infectious diseases [2,3]. In LMIC, and particularly in sub-Saharan Africa, the accuracy of the clinical diagnoses is limited due to the lack of access to laboratory diagnostic tests and imaging techniques; a common obstacle even in tertiary, referral hospitals [4,5]. In addition, although some of the sub-Saharan African countries have a very high HIV prevalence, reliable data on CoD in HIV-positive patients are particularly scarce. Unfortunately, the HIV-related in-hospital mortality remains high in sub-Saharan Africa despite the increased availability of antiretroviral therapy [6]. Indeed, many studies carried out in sub-Saharan Africa have shown a high burden of opportunistic infections associated with HIV [7,8], especially of active tuberculosis [9]. The clinical autopsy is the gold standard method for CoD determination, and an important tool for assessing the quality of clinical practice [10,11].
In many LMIC, where access to health system is limited and mortality surveillance is generally weak, autopsy data would be particularly important to complete the CoD picture which is key for health planning and prioritization [12,13]. In addition, clinical autopsy is a useful teaching tool for clinicians, vital to evaluate and improve the quality of care and the health outcomes. However, the high costs of the autopsy procedure, the lack of pathologists and of adequate pathology laboratories, as well as cultural concerns continue to be main obstacles for its expansion in LMIC [14]. In this prospective one-year study we aimed to explore the CoDs in a large series of adult deaths occurring in a tertiary referral hospital located in Maputo, the capital of Mozambique, using complete autopsy as the gold standard. Additionally, we analyzed the clinical and laboratory information on HIV status and compared the distribution of the CoDs between HIV-positive, and –negative and in patients with unknown HIV status.
Methods
Study Setting and Case Selection
This study was part of an observational study conducted at the Maputo Central Hospital (MCH), a 1500-bed government-funded quaternary care facility. The hospital is located in the capital of Mozambique and serves mainly the population of the Maputo urban and peri-urban area but is also the referral center for other hospitals in Southern Mozambique.
From the 1st of January to the 31st of December of 2013 (12-months study period), we included all cases fulfilling the following criteria:
1) An autopsy requested by the clinician and
2) Written or verbal informed consent to perform the
autopsy given by the relatives.
Exclusion criteria were:
1) Perinatal, neonatal and pediatric (0-15 years) deaths,
2) Maternal deaths (deaths occurring during pregnancy,
delivery or puerperium, i.e., within 42 days of termination of
pregnancy), and
3) Traumatic deaths.
The study received the approval of the National Bioethics Committee of Mozambique (Mozambique; approved, Ref. 342/ CNBS/13).
Autopsy Procedure
In all cases a full autopsy was performed as soon as possible after consent from the next-of-kin was obtained. The autopsy was carried out by a pathologist assisted by a technician. During the autopsy, all the thoraco-abdominal organs, as well as the central nervous system were eviscerated and dissected for detailed gross examination. A sample was obtained for histological analysis from the main organs (both lungs, liver, brain, heart, kidneys, spleen and bone marrow). The sampling was directed to any grossly evident lesion, if detected, or from normally appearing tissues if not identified. In addition, samples of any other abnormality identified in other areas (e.g. lymph nodes, bowel, skin, etc.) were obtained.
Histological Laboratory Procedure and Diagnostic Methods
Tissue samples for histological analysis were fixed in 10% neutral buffered formalin for 24-48 hours and routinely embedded in paraffin. Four-micron thick sections were stained with H&E and evaluated using an Olympus BX41 light microscope. In all the H&E slides a thorough search of hemozoin in macrophages and of malaria parasites was conducted. When deemed necessary, ancillary histochemical (e.g. Zieh-Neelsen, Gram, Periodic-Acid Schiff, Grocott stains, etc.) and/or immunohistochemical (e.g., Cytomegalovirus, Herpes, etc.) stains were performed on selected paraffin blocks.
Review of the Clinical Charts
The available clinical information was reviewed to collect diagnostic evidence for each case by one local investigator (FF). In all cases, the HIV status of the deceased patients, antiretroviral treatment, CD4 count data and the time from admission to death were abstracted from clinical charts.
Determination of the CoD
The main cause of death, all associated conditions and any
underlying diseases, were codified following the International
Classification of Diseases, tenth revision (ICD-10). The CoD were
classified into five major groups:
1) Infectious diseases,
2) Malignant tumors,
3) Non-infectious cardiovascular diseases,
4) Other non-infectious diseases, and
5) Non-conclusive
The main autopsy diagnosis was used to define the disease
category. Malaria was considered as the main CoD when massive cerebral parasitization was identified. The autopsy diagnosis
integrated all the findings from the gross and microscopic
examination together with the clinical information. In HIV infected
patients, the final CoD and not the underlying HIV infection was
considered as the main CoD (e.g., Pneumocystosis). The infectious
and neoplastic CoD (e.g., tuberculosis, fungal or bacterial infections,
etc.) were further sub-classified into localized (respiratory, central
nervous system, digestive, genitourinary, etc.) or disseminated;
Kaposi’s sarcoma and lymphoid neoplasms were always classified
as disseminated. The non-infectious cardiovascular diseases
included cardiovascular and cerebrovascular diseases. Other noninfectious
diseases were classified by system (respiratory, central
nervous system, digestive system, genitourinary, etc.) or as nonclassifiable.
Finally, when no CoD was identified after a thorough
exam, the case was classified as non-conclusive.
Statistical Methods
Data were analyzed using the SPSS program version 20.0. The proportions were compared by chi-square test. The ANOVA test was used to compare the means between three different categories. p-values <0.05 were considered as significant
Results
General Characteristics of the Series
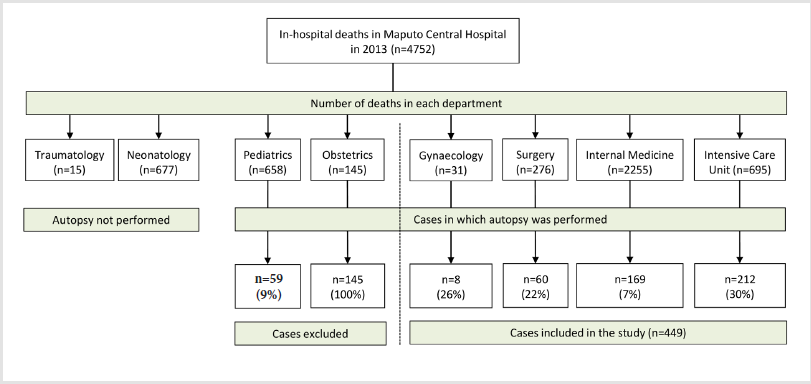
Figure 1: Number of deaths in the different departments of the hospital, the total number and the percentage of the autopsies performed from each department, as well as the excluded cases.
During the study period 4752 in-hospital non-traumatic deaths were registered at the MCH. Four hundred and forty-nine autopsies of adult patients were performed (9.4% of the non-traumatic deaths). Two hundred and twelve autopsies (47%) were requested from the intensive care unit, 169 (38%) from internal medicine, 60 (13%) from surgery and 8 (2%) from the department of gynecology. (Figure 1) shows the number of deaths in the different departments of the hospital, the total number and the percentage of the autopsies performed from each department, as well as the excluded cases. Two hundred and thirty-four patients were male (52%) and 215 were female (48%). The median age of the patients was 42 years (range 15-93 years). The median admission time prior to death was 4.4 days; 198 (44%) patients died within the first 24 hours of admission to the hospital. Overall, 166 (37%) patients were HIV-positive, 87 (19%) were HIV-negative, and in 196 (44%) cases the HIV status was not known or not documented in the clinical records. Ninety-five of the 166 HIV-positive patients (57%) were on antiretroviral treatments. The last CD4 count was available in 15 HIV-positive patients, with a median count of 46 cells/mL (range 3-329 cells/mL). Mean age (± standard deviation) of the HIV-positive, -negative and -unknown patients was 38±14, 45±19 and 52±18 years, respectively (p<0.001) and the mean time of admission was 6.3 ± 8.3, 6.3 ± 6.6 and 2.1 ± 4.5 days, respectively (p<0.001).
Overall Cause of Death Distribution
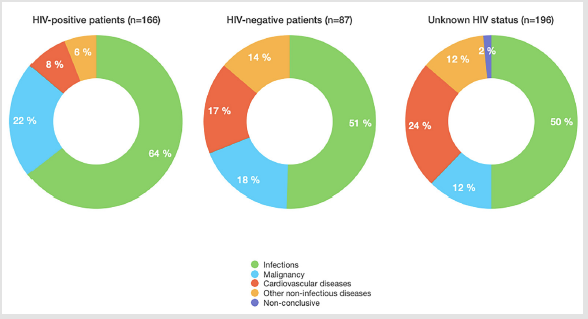
Infectious diseases were the most frequent CoD (249/449; 55%), followed by malignant tumors (76/449; 17%), cardiovascular diseases (75/449; 17%) and other non-infectious diseases (46/449; 10%). In three cases (1%) the autopsy findings were nonconclusive. The five-category CoD distribution was significantly different in HIV-positive group in comparison with HIV-negative or HIV-unknown groups (p=0.01, and p<0.001, respectively), but no differences were observed between the HIV-negative and HIVn unknown groups (p=0.40). These differences were due to the higher frequency of infectious diseases and malignancies in HIVpositive patients and of non-infectious cardiovascular diseases and other disorders in HIV-negative and -unknown patients. (Figure 2) shows the five-category CoD distribution in HIV-positive, - negative and –unknown patients.
Figure 2: Distribution of the main groups of causes of death according to the HIV status of the patients.
Specific Causes of Death
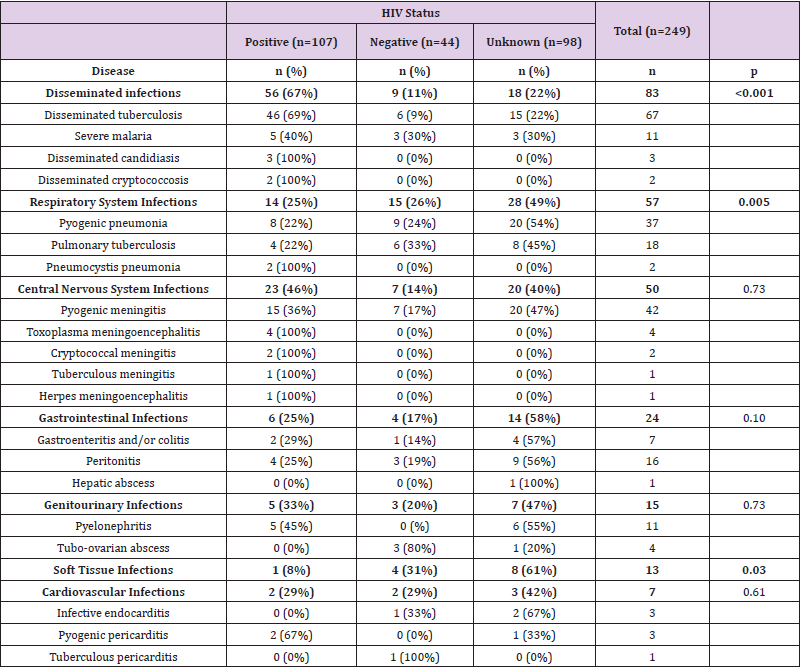
Infectious diseases accounted for 249 deaths. Disseminated infections were the most frequent infectious CoD (83; 33%), followed by respiratory (57; 23%), central nervous system (50; 20%), gastrointestinal (24; 10%), genitourinary (15; 6%), soft tissue (13; 5%) and cardiovascular infections (7; 3%). Most disseminated infections were caused by opportunistic microorganisms (mainly tuberculosis, candidiasis and cryptococcosis), and were much more frequent in HIV-positive patients than in the other two groups (p<0.001). (Table 1) shows the distribution of infectious CoD in HIVpositive, HIV-negative and patients with HIV-unknown status. The most common infectious CoD in all groups (HIV-positive, -negative and -unknown) was tuberculosis, representing 48%, 29%, and 23% of CoD, respectively. The most frequent form of tuberculosis was miliary tuberculosis (67/76; 88%), which was more common in HIV-positive than in HIV-negative or -unknown patients (p<0.001). Other frequent infectious CoD included pyogenic meningitis (42 cases; 17%) and pneumonia (37 cases; 15%). Severe malaria was considered as the cause of death in 11 adults. The mean age of the patients who died from malaria was 40 years (range 31-65).
Table 1: Infectious diseases as main causes of death (CoD) in HIV-positive, -negative and -unknown patients.
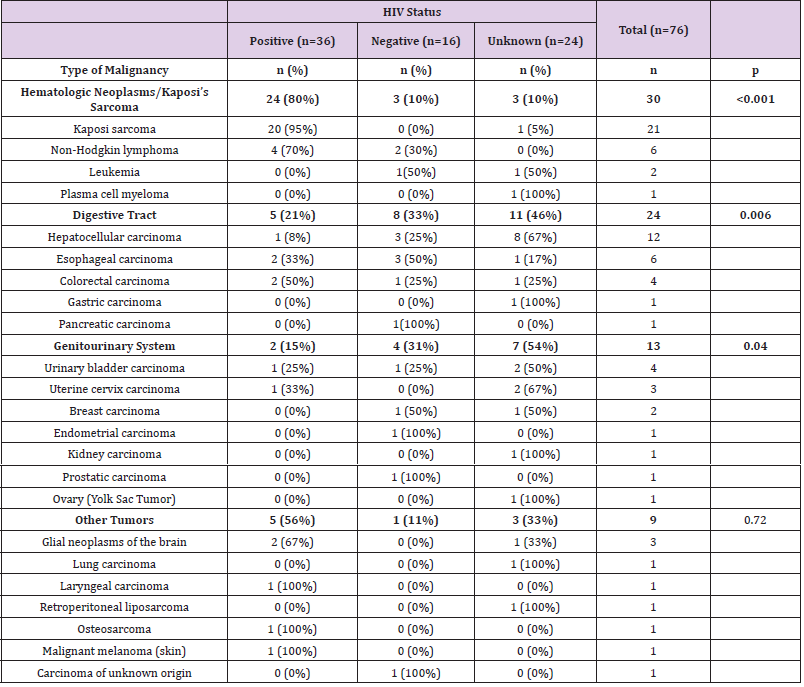
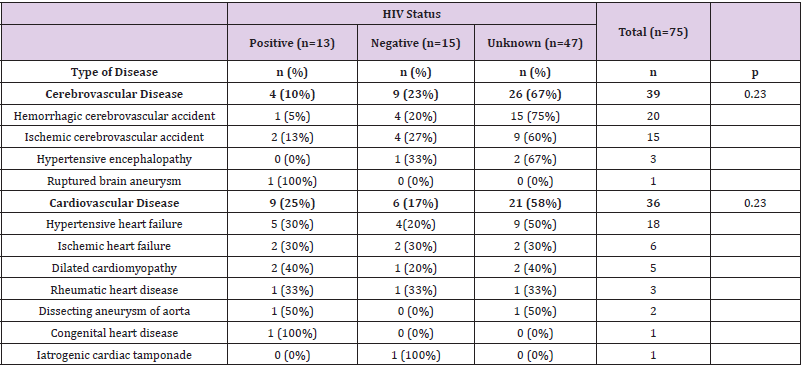
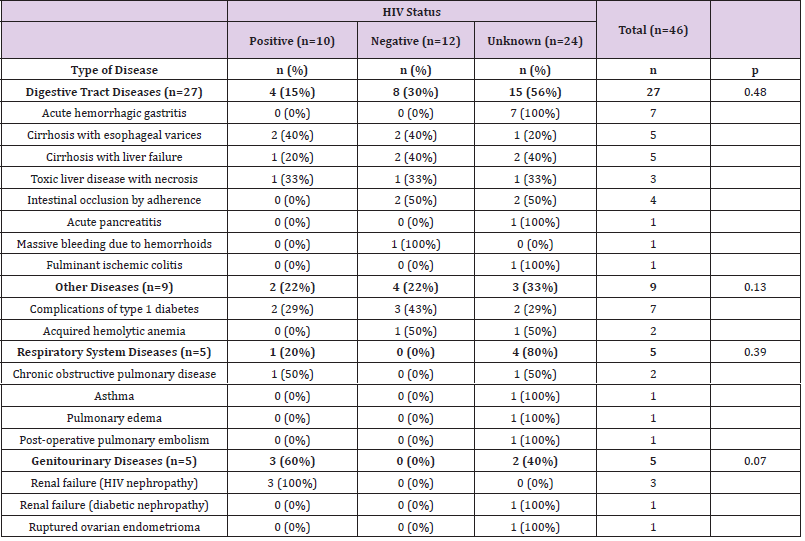
Malignant tumors accounted for 76 deaths. (Table 2) shows the distribution of main malignant disease-related CoD in HIVpositive, -negative and -unknown patients. Malignant lymphomas and Kaposi’s sarcoma, which were predominantly diagnosed in HIV-positive patients, were the most frequent tumors (30; 39%), followed by tumors of the digestive (24; 31%), genitourinary system (13; 17%) and other tumors (9; 12%). Hepatocellular carcinoma was the second most frequent malignancy, with most cases (91%) diagnosed in HIV-negative or –unknown patients. Non-infectious cardiovascular diseases accounted for 75 deaths. (Table 3) shows the distribution of these diseases in HIV-positive, -negative and -unknown patients. Cerebrovascular conditions accounted for 39 deaths (52%) and heart diseases for 36 (48%). The distribution of both groups of cardiovascular CoD was similar between HIV-positive, HIV-negative and HIV-unknown groups (p=0.23). Half of cardiovascular CoD were due to hypertensive heart failure (18; 50%), whereas ischemic heart failure was diagnosed in a small proportion of cases (6; 17%). Other non-infectious diseases accounted for 46 deaths. Table 4 shows the other non-infectious CoD in HIV-positive, -negative and -unknown patients. The diseases of gastrointestinal system comprised more than half of all diseases in the overall group (26; 56%). No differences were observed between HIV categories.
Table 2: Malignant tumors as main causes of death (CoD) in HIV-positive, -negative and -unknown patients.
Table 3: The main non-infectious cardiovascular diseases as main causes of death (CoD) in HIV-positive, negative and -unknown patients.
Table 4: The main other non-infectious diseases as main causes of death (CoD) in HIV-positive, -negative and -unknown patients.
Discussion
This is one of the largest autopsy-based studies conducted
in sub-Saharan Africa. The main strength of this study is that it
covers a full year, providing a good picture of the causes of death in
adults occurring at a single quaternary referral institution in sub-
Saharan Africa. Our data show that infectious diseases (55% of all
deaths) continue to be highly prevalent in Mozambique. This data
is in keeping with our previous studies on adult deaths in the same
institution [15,16], which revealed an even higher prevalence of
infectious CoD (71%), and HIV infection (>60% compared with the
37% observed in the current study).The high percentage of patients
in whom the HIV status was not known, in an area such as urban
Mozambique with high prevalence of HIV infection [17] reveals the
limited accessibility to laboratory tests occurring in most LMIC,
particularly sub-Saharan Africa, even in tertiary health institutions
[4,17]. However, the distribution of CoDs in this HIV-unknown
group, markedly different from the HIV-positive and similar to
the HIV-negative group, suggests that most of these patients were
probably HIV-non infected. Remarkably, the admission time prior
to death in this specific group was significantly shorter, indicating
that the absence of testing was likely due to the short timeframe
between admission and death.
The distribution of main CoD categories was markedly different
in HIV-positive compared with HIV-negative or -unknown patients.
Similar differences were observed in our previous study conducted
at the MCH [15] and in another autopsy series in Uganda [7].
Interestingly, the burden of infectious CoD was also high in patients
with HIV-negative or unknown status (51 and 50%, respectively).
Another autopsy study conducted in Zambia reported even higher
prevalence of infection in seronegative cases (79%) [9]. In contrast,
our previous postmortem study in Mozambique [15,16] and an
Ugandan series have reported lower number of infectious diseases
in HIV-negative patients (27%) [7]. As expected, and similarly to
other post-mortem series in sub-Saharan Africa [7-9,15,18,19],
India [20] and Brazilian Amazon [3], tuberculosis was the leading
infectious CoD in HIV-positive patients, contributing to onethird
of all CoD in this group. These findings are clearly different
from studies conducted in other geographic areas that reported
Cytomegalovirus as the leading CoD in HIV-positive patients,
whereas tuberculosis accounted for a small percentage of cases
(<3%) [21]. In our series, disseminated (miliary) tuberculosis
was the predominant form of the disease, which is in keeping
with the findings of other reports [7,9,20]. This high proportion
of disseminated tuberculosis probably reflects the high degree of
immunosupression of HIV-positive patients included in the study
[22]. However, tuberculosis was also a frequent CoD in HIV-negative
and -unknown patients, comprising up to 15% of all deaths in
these groups. These findings are in contrast with other autopsy
studies in sub-Saharan Africa, in which tuberculosis was rare in
HIV-negative and -unknown patients [7,9,16,19,23]. These results
highlight the need of expanding the use of the point-of-care tests for
tuberculosis, such as the Xpert MTB/RIF and Xpert MTB/RIF ultra
[24,25], which, although already introduced in Mozambique [26]
and other LMIC [27], are probably underutilized. As in many other
autopsy series, other frequent infectious CoD included pyogenic
pneumonia and central nervous system infections [7,8].
Notably, pyogenic pneumonia was more frequent in HIVnegative
and –unknown patients, in keeping with other studies
in sub-Saharan Africa [19,23]. These results highlight the need of
continued introduction of rapid point-of-care tests [28] for nontuberculous
bacterial infections in LMIC. Point-of-care tests already
introduced in Mozambique for some specific conditions (Xpert
MTB/RIF and Xpert MTB/RIF ultra for tuberculosis, cryptococcal
antigen assays, birth HIV testing [26]) could serve as successful
examples to encourage implementation of a new sensitive and
specific molecular automated next generation tests for other
infectious diseases. Surprisingly, severe malaria was low but
much more frequent than expected in an adult population from
an endemic country (2%). Most patients who died of malaria were
middle-aged (mean age, 40), which is in contrast with the older age
of patients dying of malaria in adulthood reported in other series
[29]. Although the low immunity acquired by the population of
Maputo City and Province, an area that has successfully reduced
the burden of malaria [30], can be the cause of this unexpected
mortality, further studies on the true burden of severe malaria in
this particular age group are warranted.
Another curious finding in this series is that we did not identify
any case of Cytomegalovirus infection. This infection has been
reported in Ugandan, Kenian and Zambian series, but with a low
frequency [7,9,23]. However, the unavailability of microbiological
testing or immunohistochemistry may explain, at least in part,
the absence of any identified case, because the viral inclusions in
H&E stained slides are usually scarce and unevenly distributed
and, consequently, difficult to detect [31]. Similarly to other LMIC, Mozambique shows a dual burden of malignant diseases. Indeed, a
high incidence of malignancies of infectious etiology was identified,
including the typically HIV-associated neoplasms (Kaposi’s sarcoma
and malignant lymphomas), hepatocellular carcinoma, associated
with hepatitis B virus and bladder cancer, related to Schistosoma
infection. Kaposi’s sarcoma was the most frequent malignancy in
this series, which is in accordance with the cancer registry reports
from Beira [32], the second biggest city in Mozambique [33], and
with other autopsy studies conducted in sub-Saharan Africa [7,9].
Liver carcinoma was the second most frequent malignancy in our
series and was predominantly identified among non-HIV-infected
male patients. Despite the reduction in its frequency, recent data
has shown that liver cancer is the third most frequent cancer in
Maputo in males [34]. Interestingly, in the first half of 20th century,
Mozambique showed the highest incidence of this cancer among
other sub-Saharan countries, especially in young black African
males living in the capital [35,36]. The carcinogens responsible
for this high incidence included mainly chronic hepatitis B virus
infection, but also hepatocarcinogenic toxins and dietary iron
overload [35]. However, in addition to these infection-related
cancers characteristic of LMIC, an increasing incidence of cancers
typical of western populations, like colorectal or breast carcinoma
[37] was observed, which is likely due to the westernization of
the lifestyles of the population living in the Maputo urban area, a
phenomenon occurring in other African countries [38,39].
Cardiovascular diseases accounted for a quarter of the
CoD in HIV-negative and -unknown patients. The World
Health Organization estimated that by 2020, 80% of the global
cardiovascular disease burden will occur in LMIC countries [40-
46]. The urbanization and westernization of the lifestyles in
Mozambique might be responsible for the increasing incidence
of cardiovascular diseases [47], in particular increasing alcohol
use, together with highly caloric diet with high salt intake [48]
and low fruit and vegetable consumption in urban areas [49,50].
Furthermore, the high burden of non-infectious digestive deaths in
our study reminisces the overall high prevalence of this digestive
fatal conditions in high-income countries [51]. Notably, many
LMIC are not prepared to manage this new burden [52,53]; lack
of clinical protocols, algorithms for risk stratification and poor
access to essential care have been recently identified as critical
gaps in the management of hypertension in Mozambique [54].
Other studies have recently highlighted the increasing prevalence
of hypertension and cerebrovascular diseases in African LMIC [40],
including Mozambique [41,42], especially in urban areas [43,44].
Interestingly, the deaths caused by heart failure were mostly due
to hypertensive heart disease, and not to ischemic cardiopathy,
which is in line with the accumulated evidence that the burden of
coronary artery disease remains low in the black Africans [45].
The main limitation of this study is the complete absence of any
microbiological testing in blood, cerebrospinal fluid and tissues.
Thus, we were not able to establish the diagnosis of sepsis as the
bloodstream infection should be demonstrated in multiples organs
mainly by microbiology as histological findings alone are highly
unspecific to diagnose sepsis. Moreover, lack of microbiological
testing precluded us from confirming or establishing HIV status
in our series and identifying the infectious agent(s) associated to
certain infectious diseases and infection-related malignancies. A
second limitation is the possible bias introduced by the selection
of the patients, as autopsy was performed in a reduced percentage
(9%) of all adult deaths occurring at the MCH. However, this is
one of the largest autopsy studies in the sub-Saharan area and its
results are in keeping with other studies conducted in the region.
Conclusion
The burden of infectious diseases associated to HIV infection, such as tuberculosis remains high in Mozambique. The HIV testing rates should be improved during the clinical evaluation of the patients. Apart from tuberculosis, and regardless of HIV status, pyogenic infections of the lungs and the central nervous system (most likely bacterial) are also prevalent and require improvement of the diagnostic and treatment strategies. Mozambique is also struggling with non-communicable diseases, mainly cardiovascular and oncologic conditions. Consequently, health strategies should be focused, not only on prevention and management of common infectious diseases such as HIV, tuberculosis and malaria [37], but also on the increasing burden of malignant and cardiovascular conditions. Finally, our study stresses the need of conducting regularly large autopsy-based studies in LMIC countries to adequately monitor the burden of infectious, neoplastic and cardiovascular diseases. These studies should ideally include additional microbiological analysis, to allow better classification of the different infectious diseases and the HIV status.
Conflicts of Interests
The authors have no conflicts of interest to declare.
Funding
Funded by the Bill & Melinda Gates Foundation (Global Health grant numbers OPP1067522 and OPP1128001), and by the Spanish Instituto de Salud Carlos III (FIS, PI12/00757; CM, Acciones CIBER). ISGlobal receives support from the Spanish Ministry of Science and Innovation through the “Centro de Excelencia Severo Ochoa 2019-2023” Program (CEX2018-000806-S), and support from the Generalitat de Catalunya through the CERCA Program.
References
- Setel PW, Macfarlane SB, Szreter S, Mikkelsen L, Jha P, et al. (2007) A scandal of invisibility: making everyone count by counting everyone. Lancet 370(3-9): 1569-1577.
- Ordi J, Castillo P, Garcia Basteiro AL, Moraleda C, Fernandes F, et al. (2019) Clinico-pathological discrepancies in the diagnosis of causes of death in adults in Mozambique: A retrospective observational study. PLoS One 14.
- Palhares AEM, Ferreira L, Freire M, Castillo P, Martinez MJ, et al. (2019) Performance of the Minimally Invasive Autopsy tool for Cause of Death Determination in Adults Deaths from the Brazilian Amazon: An Observational Study. Virchows Arch 475: 649-658.
- Wilson ML, Fleming KA, Kuti MA, Looi LM, Lago N, et al. (2018) Access to pathology and laboratory medicine services: a crucial gap. Lancet 391(10133): 1927-1938.
- Sayed S, Cherniak W, Lawler M, Tan SY, El Sadr W, et al. (2018) Improving pathology and laboratory medicine in low-income and middle-income countries: roadmap to solutions. Lancet 391(10133): 1939-1952.
- Wajanga BM, Webster LE, Peck RN, Downs JA, Mate K, et al. (2014) Inpatient mortality of HIV-infected adults in sub-Saharan Africa and possible interventions: a mixed methods review. BMC Health Serv Res 14: 627.
- Cox JA, Lukande RL, Nelson AM, Mayanja Kizza H, Colebunders R, et al. (2012) An Autopsy Study Describing Causes of Death and Comparing Clinico-Pathological Findings among Hospitalized Patients in Kampala, Uganda. PLoS One 7: e33685.
- Cox JA, Lukande RL, Lucas S, Nelson AM, Van Marck E, et al. (2010) Autopsy causes of death in HIV-positive individuals in sub-Saharan Africa and correlation with clinical diagnoses. AIDS Rev 12(4):183-194.
- Bates M, Mudenda V, Shibemba A, Kaluwaji J, Tembo J, et al. (2015) Burden of tuberculosis at post mortem in inpatients at a tertiary referral centre in sub-Saharan Africa: a prospective descriptive autopsy study. Lancet Infect Dis 15(5): 544-551.
- Liu D, Gan R, Zhang W, Wang W, Saiyin H, et al. (2018) Autopsy interrogation of emergency medicine dispute cases: how often are clinical diagnoses incorrect? J Clin Pathol 71(1): 67-71.
- Kuijpers CC, Fronczek J, van de Goot FR, Niessen HW, van Diest PJ, et al. (2014) The value of autopsies in the era of high-tech medicine: discrepant findings persist. JClinPathol 67: 512-519.
- Rampatige R, Gilks CF (2015) Autopsies and better data on causes of death in Africa. Lancet Infect Dis 15(5): 492-494.
- Ordi J (2020) Knowing the Causes of Death in Developing Countries : an Absolute Requirement to Reduce Mortality: 1-3.
- Bassat Q, Castillo P, Alonso PL, Ordi J, Menéndez C (2016) Resuscitating the Dying Autopsy. PLoS Med 13(1): e1001927.
- Castillo P, Martínez MJ, Ussene E, Jordao D, Lovane L, et al. (2016) Validity of a Minimally Invasive Autopsy for Cause of Death Determination in Adults in Mozambique: An Observational Study. PLOS Med 13: e1002171.
- Castillo P, Ussene E, Ismail MR, Jordao D, Lovane L, et al. (2015) Pathological Methods Applied to the Investigation of Causes of Death in Developing Countries: Minimally Invasive Autopsy Approach. PLoS One 10: e0132057.
- Korenromp EL, Gobet B, Fazito E, Lara J, Bollinger L, et al. (2015) Impact and cost of the HIV/AIDS national strategic plan for Mozambique, 2015-2019-projections with the spectrum/goals model. PLoS One 10.
- Garcia Basteiro AL, Hurtado JC, Castillo P, Fernandes F, Navarro M, et al. (2019) Unmasking the hidden tuberculosis mortality burden in a large post mortem study in Maputo Central Hospital, Mozambique. Eur Respir J 54 : 1900312.
- Ansari NA, Kombe AH, Kenyon TA, Mazhani L, Binkin N, et al. (2003) Pathology and causes of death in a series of human immunodeficiency virus-positive and -negative pediatric referral hospital admissions in Botswana. Pediatr Infect Dis J 22: 43-47.
- Lanjewar DN (2011) The spectrum of clinical and pathological manifestations of AIDS in a consecutive series of 236 autopsied cases in mumbai, India. Patholog Res Int 2011: 547618.
- Katano H, Hishima T, Mochizuki M, Kodama Y, Oyaizu N, et al. (2014) The prevalence of opportunistic infections and malignancies in autopsied patients with human immunodeficiency virus infection in Japan. BMC Infect Dis 14: 229.
- Jones BE, Young SMM, Antoniskis D, Davidson PT, Kramer F, et al. (1993) Relationship of the manifestations of tuberculosis to CD4 cell counts in patients with human immunodeficiency virus infection. Am Rev Respir Dis 148(5): 1292-1297.
- Rana FS, Hawken MP, Mwachari C, Bhatt SM, Abdullah F, et al. (2000) Autopsy study of HIV-1-positive and HIV-1-negative adult medical patients in Nairobi, Kenya. J Acquir Immune Defic Syndr 24(1): 23-29.
- Horne DJ, Kohli M, Zifodya JS, Schiller I, Dendukuri N, et al. (2019) Xpert MTB/RIF and Xpert MTB/RIF Ultra for pulmonary tuberculosis and rifampicin resistance in adults. Cochrane Database Syst Rev 6.
- García Basteiro AL, Saavedra B, Cobelens F (2017) The Good, the Bad and the Ugly of the Next-Generation Xpert Mtb/Rif® Ultra Test for Tuberculosis Diagnosis. Arch Bronconeumol 53(12): 665-666.
- Meggi B, Vojnov L, Mabunda N, Vubil A, Zitha A, et al. (2018) Performance of point-of-care birth HIV testing in primary health care clinics: An observational cohort study. PLoS One 13.
- Rajasingham R, Wake RM, Beyene T, Katende A, Letang E, et al. (2019) Cryptococcal meningitis diagnostics and screening in the era of point-of-care laboratory testing. J Clin Microbiol 57.
- Peeling RW, Mabey D (2010) Point-of-care tests for diagnosing infections in the developing world. Clin Microbiol Infect 16(8): 1062-1069.
- Dhingra N, Jha P, Sharma VP, Cohen AA, Jotkar RM, et al. (2010) Adult and child malaria mortality in India: A nationally representative mortality survey. Lancet 376(9754): 1768-1774.
- Aide P, Candrinho B, Galatas B, Munguambe K, Guinovart C, et al. (2019) Setting the scene and generating evidence for malaria elimination in Southern Mozambique. Malar J 18: 190.
- Colina F, Juci NT, Moreno E, Ballestin C, Farina J, et al. (1995) Histological diagnosis of cytomegalovirus hepatitis in liver allografts. J Clin Pathol 48(4): 351-357.
- Carrilho C, Ferro J, Lorenzoni C, Sultane T, Silva Matos C, et al. (2012) A contribution for a more accurate estimation of the incidence of Kaposi sarcoma in Mozambique. Int J Cancer 132(4): 988-989.
- International Agency of Reasearch in Cancer: Globocan 2018 data in Mozambique.
- Carrilho C, Fontes F, Tulsidás S, Lorenzoni C, Ferro J, et al. (2019) Cancer incidence in Mozambique in 2015-2016. Eur J Cancer Prev 28(4): 373-376.
- Kew MC (2013) Epidemiology of hepatocellular carcinoma in sub-Saharan Africa. Ann Hepatol 12(2): 173-182.
- MD P, FO T (1965) A Cancer Survey in Lourenço Marques, Portuguese East Africa. J Natl Cancer Inst: 35(5).
- Lorenzoni C, Oliveras L, Vilajeliu A, Carrilho C, Ismail MR, et al. (2018) Weak surveillance and policy attention to cancer in global health: The example of Mozambique. BMJ Glob Heal 3(2): e000654.
- Stower H (2019) A disease transition in sub-Saharan Africa. Nat Med 25: 1647.
- Steyn NP, Mchiza ZJ (2014) Obesity and the nutrition transition in Sub-Saharan Africa. Ann N Y Acad Sci 1311(1): 88-101.
- Akinyemi RO, Owolabi MO, Ihara M, Damasceno A, Ogunniyi A, et al. (2019) Stroke, cerebrovascular diseases and vascular cognitive impairment in Africa. Brain Res Bull 145: 97-108.
- Adeloye D, Basquill C (2014) Estimating the prevalence and awareness rates of hypertension in Africa: a systematic analysis. PLoS One 9: e104300.
- Damasceno A, Padrão P, Silva Matos C, Prista A, Azevedo A, et al. (2013) Cardiovascular risk in Mozambique: who should be treated for hypertension? J Hypertens 31(12): 2348-2355.
- Fontes F, Damasceno A, Jessen N, Prista A, Silva Matos C, et al. (2019) Prevalence of overweight and obesity in Mozambique in 2005 and 2015. Public Health Nutr 22: 3118-3126.
- Jessen N, Govo V, Calua E, Machava M, Fabula A, et al. (2019) Blood pressure screening in Mozambique: The May Measurement Month 2017 project - Sub-Saharan Africa. Eur Hear Journal, Suppl 21: D80-82.
- Dokainish H, Teo K, Zhu J, Roy A, Alhabib KF, et al. (2016) Heart Failure in Africa, Asia, the Middle East and South America: The INTER-CHF study. Int J Cardiol 204: 133-141.
- WHO (2013) A global brief on hypertension WHO 2013.
- Amegah AK (2018) Tackling the Growing Burden of Cardiovascular Diseases in Sub-Saharan Africa: Need for Dietary Guidelines. Circulation 138(22): 2449-2451.
- Leyvraz M, Mizéhoun Adissoda C, Houinato D, Baldé NM, Damasceno A, et al. (2018) Food consumption, knowledge, attitudes, and practices related to salt in urban areas in five sub-saharan African countries. Nutrients 17(1): 35.
- Padrão P, Laszczyńska O, Silva Matos C, Damasceno A, Lunet N (2012) Low fruit and vegetable consumption in Mozambique: Results from a WHO STEPwise approach to chronic disease risk factor surveillance. Br J Nutr 107: 428-435.
- Gersh BJ, Sliwa K, Mayosi BM, Yusuf S (2010) The epidemic of cardiovascular disease in the developing world: global implications the epidemic of cardiovascular disease: a global phenomenon 31: 642-648.
- Countries Compared by Health (2020) Intestinal diseases death rate. International Statistics at NationMaster.com n.d.
- Gomes A, Damasceno A, Azevedo A, Prista A, Silva Matos C, et al. (2010) Body mass index and waist circumference in Mozambique: Urban/rural gap during epidemiological transition. Obes Rev 11(9): 627-634.
- Correia JC, Lachat S, Lagger G, Chappuis F, Golay A, et al. (2019) Interventions targeting hypertension and diabetes mellitus at community and primary healthcare level in low- And middle-income countries:a scoping review. BMC Public Health :19.
- Bay N, Juga E, Mac Uacua C, João J, Costa M, et al. (2019) Assessment of care provision for hypertension at the emergency Department of an Urban Hospital in Mozambique. BMC Health Serv Res 19: 975.

 Research Article
Research Article