ABSTRACT
Cushing’s syndrome is a hormonal disorder that affects multiple systems of the body. It is caused by excessive cortisol production. Cortisol is the hormone produced by adrenal gland. Its secretions varies with circadian rhythm and its peak can be seen in the morning, however, during night it is produced in very low quantity. The pituitary gland is responsible for the secretion of adreno-corticotropic hormone, which stimulates the secretions of adrenal gland. So, if tumor develops in the pituitary gland or in adrenal gland, the secretions of cortisol ultimately increases. However, its common cause is idiopathic but it may also be caused by the excessive or prolonged intake of synthetic glucocorticoids. The disease is found 3 to 5 times more in females than in males. Menstrual irregularities, hirsutism, psychosis, plethora, fatigue and weight gain (especially centripetal obesity) are the most common clinical features. The diagnosis is normally made upon detailed history of intake of steroids and physical examination. The treatment includes both medical and surgical modalities depending upon the cause of the disease and the systems involved. This article gives an illustrative review of the disease, its causes, and diagnosis, treatment, comorbidities, complications and case reports.
Keywords: Cushing’s syndrome, associated manifestation, diagnosis of Cushing syndrome
Abbreviations: CS: Cushing’s Syndrome; ACTH: Adrenoorticotrophic Hormone; CRH: Corticotrophin Releasing Hormone; UFC: Urinary Free Cortisol; PCOS: Poly Cystic Ovary Syndrome; GIP: Gastric Inhibitory Polypeptide; ONDST: Overnight Dexamethasone Suppression Test; UFC: Urinary Free Cortisol; LDDST: Low Dose Dexamethasone Suppression Test
Introduction
Cushing’s Syndrome (CS) is a disease caused by excessive cortisol production. Cushing’s syndrome is due to excessive Adrenoorticotrophic Hormone (ACTH) secretion (either from ectopic tumor or pituitary glands, or independently produced by zona fasciculata of the adrenal cortex. Stress and low levels of blood glucocorticoids are stimulator of cortisol release [1,2]. It causes hyperglycemia via gluconeogenesis. It is involved in metabolism of fat, proteins, and carbohydrates. Hypothalamus controls the release of cortisol. ACTH (Adrenocorticotropic hormone) is secreted into the blood and stimulates the adrenal gland to release cortisol. Lower limit for cortisol is 140 mm/L and upper limit is 700 mm/L at 9:00 am. Lower limit for plasma cortisol is 80 mm/L and 350 mm/L at midnight. It has been observed that patients with hypercortisolism need an accurate evaluation of adrenal gland function after remission to prevent the occurrence of subclinical or clinical hypercorticism [3,4]. Cushing’s syndrome is a serious endocrine disorder [3]. The limbs remain relatively thin or really wasted, the whole impression giving rise to the term buffalo obesity [5]. Cushing’s disease in infants is rare and has been reported secondary to pituitary macroadenoma [3]. The diagnosis and management of the syndrome remain a challenge [3,6-9].
Actions of Glucocorticoids
Increased or stimulated level of corticosteroid is characterized by circulating neutrophils, uric acid production, free water clearance, potassium loss, sodium retention, fat deposition, protein catabolism, and glycogen deposition. Decreased or inhibited level of corticosteroids is characterized by circulating eosinophils, circulating lymphocytes, delayed hypersensitivity, lymphocyte transformation and protein synthesis [10].
Some Therapeutic Uses of Glucocorticoids
Glucocorticoids are used in diseases such as lymphoma [11], eczema, pemphigus, cerebral edema, vasculitis, temporal arteritis [12], polymyalgia rheumatica [13], systemic lupus erythematous [14], ulcerative colitis [15], hay fever [16], sarcoidosis [17], chronic bronchitis [1], emphysema [18], asthma [1] and rheumatoid arthritis [19].
Side Effects of Steroids
Side effects of steroids include buffalo hump, easy bruising and cataract [20,21].
Etiology
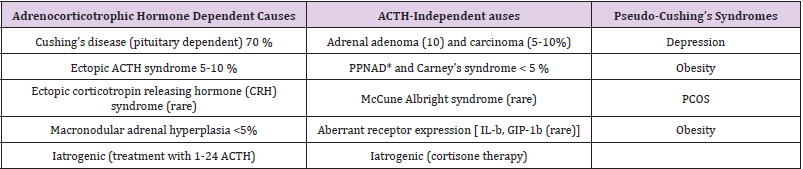
Administration of glucocorticoids for treatment of nephrotic syndrome [22], asthma [23] and immune diseases, adrenal tumor (adenoma/ carcinoma), adrenal hyperplasia, pituitary tumor cause Cushing’s syndrome. Table 1 [1].
Table 1: Classification of causes of Cushing’s Syndrome
Note: *PPNAD, Primary pigmented nodular adrenal hyperplasia
Pituitary Adenoma
Cushing’s syndrome can be caused by pituitary adenoma [24]. Pituitary adenoma secretes an increased amount of Adrenocorticotropic hormone. Cushing’s syndrome affects women more frequently (five times) than men [1].
Ectopic ACTH Syndrome
Some tumors develop outside the pituitary gland and secrete ACTH. This condition is called ectopic ACTH syndrome [25]. Fifty percent of cases are due to lung cancer. This condition occurs in men 3 times more than in women [26].
Clinical features
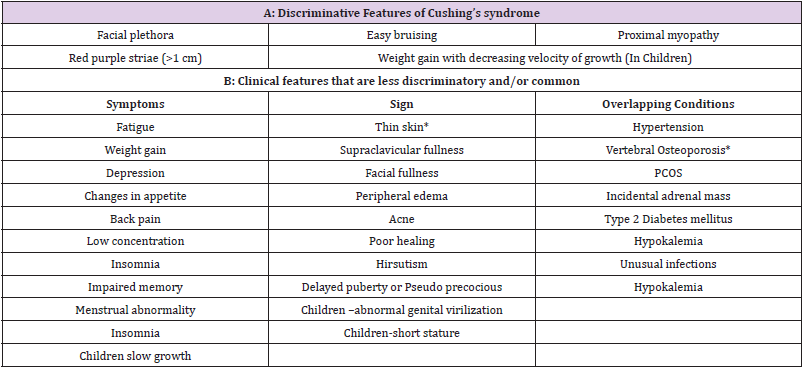
Clinical signs of Cushing’s disease include truncal obesity, moon faces, plethora, increased fragility of the skin with ecchymosis and striae, muscle atrophy, easy fatigability and weakness, mild acne, hirsutism, amenorrhea, nephrolithiasis, hypertension, leukocytosis with lymphopenia and eosinophilia, glucose intolerance and osteoporosis [4]. However, these gross clinical manifestations are not always present. Purple shaped striae of greater than 1 cm in width proximal myopathy, facial plethora, and easy bruising are the main features. All of these signs are the hallmark of protein wasting that is specific to Cushing’s disease. Central obesity and weight gain is the common feature of Cushing’s syndrome. Besides central obesity, deposition of fat also occurs in parts like temporal region, cheeks, supra-clavicular region, and thoracic-cervical spine results in moon like round face. Plethora and bruising over the face occurs due to thinning of skin in these areas because of hyper-cortisolemia. Typically, striae are normally present over abdomen, arms, breasts, and upper thighs. In case of Adrenocorticotropic hormone dependent Cushing’s disease, skin pigmentation is usually present. Increased tendency for fractures due to unexplained osteoporosis is another clinical feature of protein wasting. Presence of these discriminative signs guides us to be doubtful and to investigate more. They also help to differentiate pseudo-Cushingoid states (i.e. alcoholism, obesity, depression, and metabolic syndrome with or without diabetes and hypertension) from Cushing’s state. In case of exogenous Cushing’s syndrome, the common clinical manifestations are cataract, glaucoma, pancreatitis, intracranial HTN (benign), and head of the femur necrosis. (Table 2).
Diagnosis
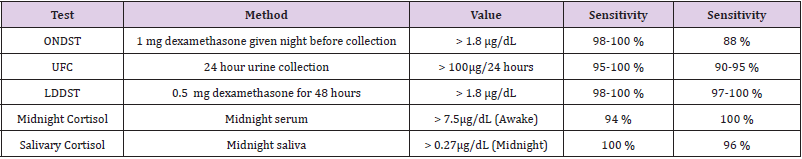
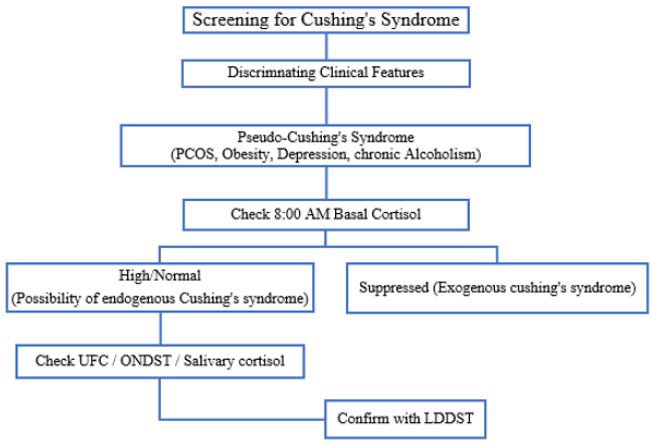
The diagnosis is based on the patient’s medical history, physical examination and laboratory tests [27]. Often, X-ray examinations of the adrenal or pituitary glands are useful for identifying tumors [28]. Screening is necessary to differentiate true Cushing’s syndrome from pseudo- Cushing’s syndrome. As in pseudo- Cushing’s syndrome over activity of hypothalamic pituitary axis may results in hypercortisolism, abnormal suppressibility of dexamethasone and a slight rise of Urinary Free Cortisol (UFC) [29]. Dexamethasone suppression test followed by Corticotrophin Releasing Hormone (CRH) stimulation is usually the test of choice for this purpose. After CRH stimulation test patients with Cushing’s syndrome have a cortisol value > 1.4 μg/dL, whereas patients with pseudo-Cushing’s syndrome have no effect on their cortisol level [29]. Now the next step is to exclude the exogenous cause from endogenous cause of Cushing’s syndrome. Apart from clinical history, level of basal (8:00 am) cortisol differentiates these two causes. Cushingoid features with suppressed level of cortisol are suggestive of exogenous cause except for cyclic Cushing’s syndrome in which decreased level of cortisol is present. Various tests are used for the screening purposes as depicted in Table 3.
Laboratory tests
24-hour Urinary Free Cortisol Levels
Overnight low dose dexamethasone suppression test
It is observed that cortisol level decreases after administration of dexamethasone in normal person. However, in case of patient with Cushing’s syndrome, cortisol level does not decrease. In this test, dexamethasone 1 mg is administered at 11 pm. and cortisol level is checked at 8 am. Level of plasma cortisol level more than 5 μg/dl indicates hypercorticism (Cushing syndrome) [29].
Concentration of cortisol in urine reflects the concentration of cortisol in the blood [30]. The level of urinary free cortisol between 300-1000 μg/24 hours indicates Cushing’s syndrome.
CRH Stimulation Test and Direct Imaging of Endocrine Glands
Lithoeidous sinus sampling [31]. The dexamethasone-CRH test. After confirmation of hypercortisolism (Cushing syndrome), the initial step is to differentiate non-ACTH dependent Cushing’s syndrome from ACTH dependent. Level of ACTH is measured for this purpose. After the confirmation of dependent Cushing’s syndrome, further test are performed to distinguish ectopic or pituitary cause. In the presence of undetectable ACTH and excessive cortisol secretion, which are indicators of tumor of the adrenal gland, therefore CT scan for detection of adrenal tumor is performed. If ACTH is normal or raised, it shows ectopic ACTH syndrome or pituitary tumor. MRI is performed for detection of pituitary tumor. For detection of ectopic source, CT chest, chest X-ray and CT abdomen is done to find out the source (Figure 1).
Complications
Complications of Cushing syndrome include high blood pressure [32], diabetes mellitus [33], serious infections [34], enlargement of pituitary tumor [31], fractures due to osteoporosis [35] and kidney stones [33].
Treatment of Cushing Disease
Medical Treatment
Fluconazole inhibits adrenal steroid formation [1] and is used preoperatively before surgery is undertaken for adrenal tumor [1]. Hypertension is also managed by prescribing antihypertensive drugs [36]. Patients who are not a candidate for surgery are given ketoconazole 200 mg 6- hourly [37].
Surgical Treatment
Pituitary lesion: Transphenoidal surgery is the first choice for treatment of pituitary tumor. Function of pituitary gland restores but corticotrophin level suppresses and that requires 6-36 months to recover normal function. Hydrocortisone treatment is given during this period [38]. Patients who fail to have remission after pituitary surgery can be treated by laparoscopic removal of both adrenal glands [1] (Tables 1-3).
Case Reports
Herbal Formulation and Cushing’s Syndrome
A case of Cushing’s syndrome was reported in a 69-year-old woman that was using the herbal formulation, Sinatren. This drug was analyzed and it was found that Sinatren contain steroids. The patient was advised not to use this drug in future. After discontinuation of this drug, she developed adrenal insufficiency, for which she needed substitution of steroids. Traditional medicine practitioners should be aware of the presence of corticosteroids in herbal formulation that are not mentioned on the instruction leaflet [39].
Chinese Medicine and Cushing Syndrome
Traditional medicines are prescribed for chronic arthritis including gout [1]. Modern herbal formulations that are available in the form of capsules or tablets may contain corticosteroids [40]. A 60-year-old Chinese man came to a hospital in Singapore with gastro-enteritis. From the history and physical examination, it was found that the patient is suffering from Cushing’s syndrome. He had been previously told that he was suffering from gouty arthritis and Trado-medical physicians had prescribed Chinese medicine for him. On analysis of the medicine, it was found that it contained corticosteroids. Doctors should observe and take note of herbal drug contents such as this Chinese medicine that may contain cortisol with side effects such as Cushing’s syndrome [41].
Total Bilateral Adrenalectomy due to Cushing’s Syndrome and Pre-Eclampsia
A case has been reported of pre-eclampsia during the eighth month of pregnancy in a woman with total bilateral adrenalectomy due to Cushing’s syndrome. During this illness, it was observed that there was less amount of cortisol in the blood. Aldosterone level in urine was also less as compared to normal pregnancies in adrenalectomized women after withdrawal of steroid therapy. Hypertension remained a specific sign of preeclampsia. These events cast doubt on the etiologic role of the adrenal steroids in toxemia of pregnancy [42].
Cutaneous Alternariosis in Association with Scabies or Iatrogenic Cushing’s Syndrome
Cutaneous alternariosis is not common. Infectious diseases are common in immunocompromised patients. Three cases have been reported from Taiwan. Patients suffering from this disease were living in Tainan and by occupation were farmers. Crusted papules were developed over the extensor aspect of the forearms or hands of these patients. Biopsy specimens showed pure colonies of Alternaria sp. Pleomorphic fungal elements in the dermis within suppurative, granulomatous infiltrates were detected. Seven common antigens were administered intradermal and these patients showed negative reaction to these antigens. Iatrogenic Cushing’s syndrome was found in case 2 and 3. Extensive scabies had case 1 and 3; Norwegian type was in case 1. In this study, the author was reporting for the first time, scabies associated with alternariosis. When intralesional amphotericin B was administered then the infection spontaneously subsided in Case 1 but in Case 2, infection regressed after seven weeks [43]. It was concluded that cutaneous alternariosis may occur in association with scabies or iatrogenic Cushing’s syndrome.
Cushing’s Syndrome and Diabetes Mellitus
Diabetes mellitus may occur as complication of Cushing’s syndrome that usually occurs due to excess amount of glucocorticoids 1 Clinical feature are weakness in proximal muscles, central obesity, cane, purple ribs, neuropsychological disorders and hirsutism. Diabetes is a metabolic disorder that occurs due to relative or absolute deficiency of insulin resulting in hyperglycemia and glycosuria [44]. However, there is excess amount of cortisol that is responsible for diabetes mellitus. Woods et al, 2014 studied the interrelationship of diabetes and Cushing syndrome [1].
Conclusion
Cushing’s syndrome occurs due to increased levels of cortisol in the blood. This disease is associated with various diseases such as systemic hypertension, diabetes, osteoporosis, decreased immune function and impaired development, visceral obesity, insulin resistance. Cushing’s syndrome occurs when the body is exposed to high levels of the hormone cortisol or other steroid hormones. This disease can be prevented by organizing awareness programs about Cushing’s syndrome. It is recommended that prophylaxis against chronic diseases should also be used. The development of new drugs provides the clinicians with several choices to treat patients with residual cortisol excess. However, the long-term effects and comorbidities associated with hypercortisolism need continuous care for patients affected by this challenging syndrome, Improvements in diagnosis and management of Cushing’s disease have raised patients’ survival rate.
Funding
There is no funding for this work.
Conflict of Interest
Authors declare that there is no conflict of interest.
References
- Woods JA, Wheeler JS, Finch CK, Nathan A Pinner (2014) Corticosteroids in the treatment of acute exacerbations of chronic obstructive pulmonary disease. International journal of chronic obstructive pulmonary disease 9: 421-430.
- Fancourt D, Aufegger L, Williamon A (2015) Low-stress and high-stress singing have contrasting effects on glucocorticoid response. Frontiers in psychology 6: 1242.
- Lahera MV, César Varela da Costa (2009) Prevalence, etiology and clinical findings of Cushing's syndrome. Endocrinologia y nutricion: organo de la Sociedad Espanola de Endocrinologia y Nutricion 56(1): 32-39.
- Nieman LK (2015) Cushing's syndrome: update on signs, symptoms and biochemical screening. European journal of endocrinology 173(4): M33-M38.
- Hewagalamulage S, Lee T, Clarke I, B A Henry (2016) Stress, cortisol, and obesity: a role for cortisol responsiveness in identifying individuals prone to obesity. Domestic animal endocrinology 56: S112-S120.
- Malek M, Esfehanian F, Amouzegar A, Farzaneh Sarvghadi, Zohreh Moossavi (2016) A survey of clinical practice patterns in diagnosis and management of Cushing's disease in Iran. Medical journal of the Islamic Republic of Iran 30: 334.
- Hartmann K, Koenen M, Schauer S, Sebastian Schauer, Stephanie Wittig Blaich, et al. (2015) Molecular actions of glucocorticoids in cartilage and bone during health, disease, and steroid therapy. Physiological reviews 96(2): 409-447.
- Alexandraki KI, Grossman AB (2010) The ectopic ACTH syndrome. Reviews in endocrine and metabolic disorders 11(2): 117-126.
- Yin L, Lucas S, Maurer F, Uli K, Rolf W, et al. (2012) Novel imidazol-1-ylmethyl substituted 1, 2, 5, 6-tetrahydropyrrolo [3, 2, 1-ij] quinolin-4-ones as potent and selective CYP11B1 inhibitors for the treatment of Cushing’s syndrome. Journal of medicinal chemistry 55(14): 6629-6633.
- Ramamoorthy S, Cidlowski JA (2016) Corticosteroids: mechanisms of action in health and disease. Rheumatic Disease Clinics 42(1): 15-31.
- Weller M (1999) Glucocorticoid treatment of primary CNS lymphoma. Journal of neuro-oncology 43: 237-239.
- Rahman W, Rahman FZ (2005) Giant cell (temporal) arteritis: an overview and update. Survey of ophthalmology 50(5): 415-428.
- Cimmino MA, Parodi M, Montecucco C, Roberto C (2011) The correct prednisone starting dose in polymyalgia rheumatica is related to body weight but not to disease severity. BMC musculoskeletal disorders 12: 94.
- Amissah Arthur MB, Gordon C (2010) Contemporary treatment of systemic lupus erythematosus: an update for clinicians. Therapeutic advances in chronic disease 1(4): 163-175.
- Khan HMW, Mehmood F, Khan N (2015) Optimal management of steroid-dependent ulcerative colitis. Clinical and experimental gastroenterology 8: 293-302.
- Østergaard MS, Østrem A, Söderström M (2005) Hay fever and a single intramuscular injection of corticosteroid: a systematic review. Primary Care Respiratory Journal 14(3): 124-130.
- Nagai S, Yokomatsu T, Tanizawa K, Kohei Ikezoe, Tomohiro Handa, et al. (2014) Treatment with methotrexate and low-dose corticosteroids in sarcoidosis patients with cardiac lesions. Internal Medicine 53: 427-433.
- Shaker SB, Dirksen A, Ulrik CS, Marianne Hestad, Trine Stavngaard, et al. (2009) The effect of inhaled corticosteroids on the development of emphysema in smokers assessed by annual computed tomography. COPD: Journal of Chronic Obstructive Pulmonary Disease 6(2): 104-111.
- Van der Goes MC, Jacobs JW, Bijlsma JW (2016) Rediscovering the therapeutic use of glucocorticoids in rheumatoid arthritis. Current opinion in rheumatology 28(3): 289-296.
- James ER (2007) The etiology of steroid cataract. Journal of Ocular Pharmacology and Therapeutics 23(5): 403-420.
- Büttner A, Thieme D (2010) Side effects of anabolic androgenic steroids: pathological findings and structure–activity relationships. Doping in Sports: Biochemical Principles, Effects and Analysis. Springer 195: 459-484.
- Bagga A (2008) Revised guidelines for management of steroid-sensitive nephrotic syndrome. Indian journal of nephrology 18(1): 31-39.
- Krishnan JA, Davis SQ, Naureckas ET, Peter G, Brian H Rowe (2009) An umbrella review: corticosteroid therapy for adults with acute asthma. The American journal of medicine 122(11): 977-991.
- Pu J, Wang Z, Zhou H, Ailing Z, Kai Z, et al. (2016) Isolated double adrenocorticotropic hormone-secreting pituitary adenomas: A case report and review of the literature. Oncology letters 12(1): 585-590.
- Alexandraki KI, Grossman AB (2016) Therapeutic strategies for the treatment of severe Cushing’s syndrome. Drugs 76(4): 447-458.
- Kamp K, Alwani R, Korpershoek E, G J H Franssen, W W de Herder, et al. (2016) Prevalence and clinical features of the ectopic ACTH syndrome in patients with gastroenteropancreatic and thoracic neuroendocrine tumors. European journal of endocrinology 174(3): 271-280.
- Findling JW, Raff H Diagnosis of Endocrine Disease: Differentiation of pathologic/neoplastic hypercortisolism (Cushing’s syndrome) from physiologic/non-neoplastic hypercortisolism (formerly known as pseudo-Cushing’s syndrome). European journal of endocrinology 176(5): R205-R216.
- Stratakis CA (2016) Diagnosis and clinical genetics of Cushing syndrome in pediatrics. Endocrinology and Metabolism Clinics 45(2): 311-328.
- Yanovski JA, Cutler Jr GB, Chrousos GP, Lynnette K Nieman (1998) The dexamethasone-suppressed corticotropin-releasing hormone stimulation test differentiates mild Cushing’s disease from normal physiology. The Journal of Clinical Endocrinology & Metabolism 83(2): 348-352.
- Kapoor N, Job V, Jayaseelan L, Simon Rajaratnam (2012) Spot urine cortisol–creatinine ratio–A useful screening test in the diagnosis of Cushing's syndrome. Indian journal of endocrinology and metabolism 16(2): S376-377.
- Oldfield EH, Doppman JL, Nieman LK, D L Miller, D A Katz, et al. (1991) Petrosal sinus sampling with and without corticotropin-releasing hormone for the differential diagnosis of Cushing's syndrome. New England Journal of Medicine 325(13): 897-905.
- Cicala MV, Mantero F (2010) Hypertension in Cushing’s syndrome: from pathogenesis to treatment. Neuroendocrinology 92(supl 1): 44-49.
- Pivonello R, De Leo M, Vitale P, Chiara Simeoli, Maria Cristina, et al. (2010) Pathophysiology of diabetes mellitus in Cushing’s syndrome. Neuroendocrinology 92(Suppl 1): 77-81.
- Bakker R, Gallas P, Romijn JWM (1998) Cushing’s syndrome complicated by multiple opportunistic infections. Journal of endocrinological investigation 21: 329-333.
- Khanine V, Fournier J, Requeda E, JP Luton, F Simon, et al. (2000) Osteoporotic fractures at presentation of Cushing's disease: two case reports and a literature review. Joint, bone, spine: revue du rhumatisme 67(4): 341-345.
- Karnes JH, Cooper-DeHoff RM (2009) Antihypertensive medications: benefits of blood pressure lowering and hazards of metabolic effects. Expert review of cardiovascular therapy 7(6): 689-702.
- Castinetti F, Guignat L, Giraud P, Marie Muller, Peter Kamenicky, et al. (2014) Ketoconazole in Cushing's disease: is it worth a try? The Journal of Clinical Endocrinology & Metabolism 99(5): 1623-1630.
- Hamid O, El Fiky L, Hassan O, Ali Kotb, Sahar El Fiky (2008) Anatomic variations of the sphenoid sinus and their impact on trans-sphenoid pituitary surgery. Skull base 18(1): 9-15.
- Oldenburg Ligtenberg P, Van Der Westerlaken M (2007) A woman with Cushing’s syndrome after use of an Indonesian herb: a case report. Neth J Med 65(4): 150-152.
- Fung FY, Linn YC (2017) Steroids in traditional Chinese medicine: what is the evidence? Singapore medical journal 58(3): 115-120.
- Edwards C, Lian T, Chng H (2002) Cushing's syndrome caused by treatment of gout with traditional Chinese medicine. Qjm 95(10): 705.
- Moses AM, Lobotsky J, Lloyd CW (1959) The occurrence of pre-eclampsia in a bilaterally adrenalectomized woman. The Journal of Clinical Endocrinology & Metabolism 19(8): 987-994.
- Chen H, Kao H, Hsu M, J Y Lee (1992) Cutaneous alternariosis in association with scabies or iatrogenic Cushing's syndrome. Journal of the Formosan Medical Association 91(4): 462-466.
- Al-Hassan N (2003) Definition of diabetes mellitus. The British Journal of General Practice 53(492): 567-568.

 Review Article
Review Article