Abstract
Pregabalin is a very potent drug used against the treatment of epilepsy, anxiety, and neuropathic pain, and therefore is a commonly prescribed drug. Apart from producing beneficial effects, this drug also has a greater tendency to cause dependency, which can often lead to its abuse. The drug is often bought illegally from the online black market and taken along with other CNS depressants such as antihistamine, anticonvulsants, cannabis, amphetamines, amphetamines, zopiclone, cocaine, antipsychotics, alcohol, opiates, opioids, and antidepressants, which can lead to serious adverse effects such as coma and death. In 93 postmortem cases, an LC-MS-MS test was established and applied to assess the presence of pregabalin in blood. These cases included drug-related deaths, alternative death causes, and deaths where pregabalin was the known cause of death. The postmortem blood plasma concentration of pregabalin varied from case to case but was often found in a higher range than the usual maximum recommended dose (600 mg / L) by doctors. These findings provide additional data to assist in determining the importance of concentrations of postmortem pregabalin and a concentration of 25 mg/L is suggested toxicologically important. Pregabalin poses a significant toxicological risk, especially with concomitant use of other CNS depressant drugs, and current laboratory protocols should be checked in order to detect the presence of pregabalin.
Keywords: Toxicology; Post-Mortem; Pregabalin; Liquid Chromatography–Mass Spectrometry; Gamma-Aminobutyric Acid; Substance of Abuse
Introduction
Pregabalin, developed as a structural successor of gabapentin, is a drug that was initially used for treating epilepsy, but later on, it was also found to be effective against neuropathic pain, generalized anxiety disorder, and fibromyalgia. Pregabalin is an analog of Gamma-Aminobutyric Acid (GABA) or gabapentinoid, which enhances the expression of an enzyme known as L-Glutamic Acid Decarboxylase (GAD) [1]. This enzyme is responsible for the synthesis of GABA in the body and, thus leads to an increase in the level of GABA in the brain. This produces GABAergic actions such as anticonvulsant, anxiolytic and analgesic [2].Pregabalin is marketed under the brand name ‘Lyrica’ which can be purchased in the form of 25-300 mg tablets, as per the direction laid by the British national formulary, and depending on the patient’s condition, it can be prescribed up to 600 mg daily. The commonly adverse effects observed due to consumption of pregabalin may include headaches, restlessness, disorientation, somnolence, and dizziness, as well as hypersensitivity reactions (angioedema, skin rash, and anaphylaxis). With an estimated half-life in the range of 4.6 to 6.8 hours, pregabalin takes only 1.5 hours to achieve its peak plasma condition and it only takes 1-2 days to reach a steady state condition [3]. But, owing to the chemical framework and the nature of pregabalin is not readily detectable by most of the available analytical techniques used by the toxicology laboratories and thus does not tend to appear in the laboratory screening procedures, and routines.
Although a few methods have been published for specific analysis of pregabalin, there is still a paucity of available literature about the concentrations found in the clinical and forensic reports. Under normal circumstances (where 600 mg is the maximum recommended dose), the blood plasma concentration of pregabalin is found within the range of 2.8 to 8.3 mg/L [4]. However, in epileptic patients, the average steady state concentration of pregabalin in plasma was found to be 1.3 mg / L, as they generally take lower daily doses of 150 mg (Deeb et al., 2014). Pregabalin was approved in 2004 in the United Kingdom (UK), since then it has become a widely prescribed drug [5]. In the UK only, there was a 350 % increase in the prescription of pregabalin from 2010 to 2015, and the very first death due to pregabalin was reported within 2 years of its birth [6].
The abuse of Pregabalin
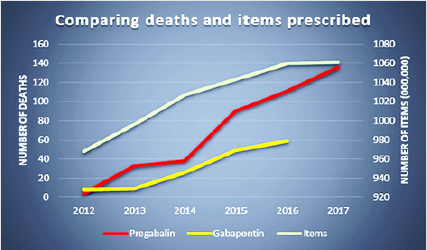
Even though pregabalin is a very potent drug for the treatment of epilepsy or anxiety but still its use has been restricted as it was being more abused then prescribed. A representation of pregabalininduced pleasure is shown in Figure 1. It was found that pregabalin was been purchased illegally [7,8] without prescription from the online pharmacies available on the black market and people were found to be taking up to 5000 mg of dose, which is very high in comparison to the maximum recommended doses of 600 mg. People were found to take pregabalin along with opiates to enhance the euphoric effect. Pregabalin is also abused for the development of recreational feelings such as relaxation, calmness, euphoria (which also include increasing the euphoric effects of drugs like opiates) and eventually sedation. The biggest concern behind the abuse of pregabalin is that its overdose can lead to serious adverse effects that ranges from drowsiness related accidents to coma and death. A case of atrioventricular blockage was also reported in a study, but the serum concentration of pregabalin was not reported [9,10]. Figure 2 shows the year wise comparison of the deaths associated with pregabalin, gabapentin and other drugs [11].
About 316 deaths have been reported due to the overconsumption of pregabalin and postmortem blood concentration of this drug in these cases were found to be 15 mg / L, which is very high when compared with reported 5.8 mg/L of pregabalin blood concentration in normal cases [12]. In a series of cases where pregabalin was present [13], an additional study found an 8.0 mg/L median post-mortem blood pregabalin concentration. The postmortem blood concentrations of 48, 110, 25, and 180 mg/L were reported in those recorded deaths involving pregabalin along with other drugs, with the latter two cases involving concentrations of at least one other drug [14].Importantly, pregabalin does not appear to be susceptible to postmortem redistribution following analysis was done previously [15] central and peripheral blood concentrations. The average fatal dose of pregabalin was found to be different centrally (54.1 mg/L) and peripherally (45.3, and 206.7 mg/L). Even in some non-fatal pregabalin overdose cases the serum concentration of this drug was found to be varied depending upon the condition of the person such as 20.8 mg/L was found when a person is drowsy but with no toxic symptoms founds, 60 mg/L was found after 24 hours of the pregabalin ingestion and 66.5 mg/L was found at the time of coma [16-20]. One of the major problems that are found with this drug is difficulty in the detection of this drug by several analytical techniques in a person due to its nature and chemical structure. Consequently, to figure out the involvement of this drug in a casework has been very challenging for forensic toxicologist thus methods with high accuracy are needed.A casework reported presence of pregabalin in 93 postmortem cases out of which 71 were deaths which were directly related to drug where the median concentration of the drug was found to be 7.0 mg/L (< 0.6 mg/L to 21.6 mg/L) and 13 cases were found to be due to alternative reasons and in such people the median concentration was 2.6 mg/L (< 0.6 mg/L to 4.9 mg/L). In 9 cases, where pregabalin was the major contributor of the fatalities, the median concentration of this drug was found to be 57.0 mg/L (28 mg/L to 182 mg/L). Antihistamine, anticonvulsants, cannabis, amphetamines, amphetamines, zopiclone, cocaine, antipsychotics, alcohol, opiates, opioids, and antidepressants, are some of the very common drug types found in the blood of these cases along with pregabalin.
Discussion
It is very rare to detect pregabalin alone in the blood sample instead is usually detected in conjunction with opiates or any other CNS depressants making it difficult to measure its precise concentration which might lead to the toxicity. While some methods for detailed pregabalin analysis [21] have been published, there is still a lack of documented literature in clinical and forensic casework concentrations.Among the fatal, the high prevalence of pregabalin abuse among morphine/heroin users indicates that this drug produced synergistic action with other CNS depressants drugs, thereby leading to coma and death. Hence, it is observed that pregabalin reduces the threshold value of other CNS depressants drugs at which they produce fatal adverse effects. Among the 93 postmortem cases, the cases which occurred due to alternative reason the concentration of pregabalin did not exceed 22 mg/L. This highlighted 9 such cases in which the concentration of the drug was higher than 22 mg/L with lowest being 28 mg/L in one of the cases where alcohol was also found in the blood, which might also have contributed towards pregabalin toxicity.The highest concentration of pregabalin was found to be 182 mg/L which lead to head trauma. In other cases, the concentration of pregabalin along with other drugs ranged in between 30 mg/L to 156 mg/L and it was inferred that in such cases death might even not have occurred if pregabalin was not used. Nevertheless, in the instances, there was evidence of improper use of pregabalin, whether prescribed or abused. Based on all the findings, the concentrations of pregabalin greater than 25 mg/L in blood could, therefore, be considered significant, especially in the presence of opiate / opioid drugs. This is also confirmed by the blood levels found under the influence of drug cases in the somewhat limited number of driving, where a median concentration of 4.6 mg/L was calculated that would be compatible with medicinal use.
Conclusion
Developing and applying a system for the identification and quantitation of pregabalin in the blood has made it possible to recommend a 25 mg/L toxicological sense threshold for pregabalin concentrations. However, very few studies support this value and thus more studies are needed to identify or generalize the toxic range of pregabalin. Until the suspicion of the presence of pregabalin is made early, this drug is not specifically analyzed in the forensic toxicology. Since pregabalin is sometimes illegally obtained, it this therefore important to develop a specific method to detect and quantify this drug in the laboratory during forensic casework studies.
References
- Aksakal E, Bakirci EM, Emet M, Uzkeser M (2012) Complete atrioventricular block due to overdose of pregabalin. The American journal of emergency medicine 30(9): 2101-e1.
- Berry D, Millington C (2005) Analysis of pregabalin at therapeutic concentrations in human plasma/serum by reversed-phase HPLC. Therapeutic drug monitoring 27(4): 451-456.
- Braga AJ, Chidley K (2007) Self‐poisoning with lamotrigine and pregabalin. Anaesthesia 62(5): 524-527.
- Button J, Berry D, Holt DW (2010) Two fatalities involving pregabalin. ToxichemKrimtech 77(03): 247-248.
- Deeb S, McKeown DA, Torrance HJ, Wylie FM, Logan BK (2014) Simultaneous analysis of 22 antiepileptic drugs in postmortem blood, serum and plasma using LC–MS-MS with a focus on their role in forensic cases. Journal of analytical toxicology 38(8): 485-494.
- Dworkin RH, Kirkpatrick P (2005) Pregabalin. Nature Review of Drug Discovery 4(6): 455-456.
- Gajraj NM (2007) Pregabalin: its pharmacology and use in pain management. Anesthesia & Analgesia 105(6): 1805-1815.
- Häkkinen M, Vuori E, Kalso E, Gergov M, Ojanperä I (2014) Profiles of pregabalin and gabapentin abuse by postmortem toxicology. Forensic science international 241: 1-6.
- Hamilton I, Sumnall H (2019) Prescription drugs pregabalin and gabapentin have been reclassified – but it will not stop problem use. The Conversation, Australia Edition.
- Karinen R, Vindenes V, Hasvold I, Olsen KM, Christophersen AS (2015) Determination of a selection of anti‐epileptic drugs and two active metabolites in whole blood by reversed phase UPLC‐MS/MS and some examples of application of the method in forensic toxicology cases. Drug testing and analysis 7(7): 634-644.
- Kostić N, Dotsikas Y, Jović N, Stevanović G, Malenović A (2015) Quantitation of pregabalin in dried blood spots and dried plasma spots by validated LC–MS/MS methods. Journal of pharmaceutical and biomedical analysis 109: 79-84.
- Launiainen T, Ojanperä I (2014) Drug concentrations in post‐mortem femoral blood compared with therapeutic concentrations in plasma. Drug testing and analysis 6(4): 308-316.
- Miljevic C, Crnobaric C, Nikolic S, Lecic Tosevski D (2012) A case of pregabalin intoxication. Psychiatrike Psychiatriki 23(2): 162-165.
- Mudiam MKR, Chauhan A, Jain R, Fatima G, Malhotra E (2012) Development, validation, and comparison of two microextraction techniques for the rapid and sensitive determination of pregabalin in urine and pharmaceutical formulations after ethyl chloroformate derivatization followed by gas chromatography–mass spectrometric analysis. Journal of pharmaceutical and biomedical analysis 70: 310-319.
- Priez Barallon C, Carlier J, Boyer B, Benslima M, Fanton L (2014) Quantification of pregabalin using hydrophilic interaction HPLC-high-resolution MS in postmortem human samples: eighteen case reports. Journal of analytical toxicology 38(3): 143-148.
- Schifano F (2014) Misuse and abuse of pregabalin and gabapentin: cause for concern? CNS drugs, 28(6): 491-496.
- Schifano F, D Offizi S, Piccione M, Corazza O, Deluca P (2011) Is there a recreational misuse potential for pregabalin? Analysis of anecdotal online reports in comparison with related gabapentin and clonazepam data. Psychotherapy and psychosomatics 80(2): 118-122.
- Spiller HA, Bratcher R, Griffith JR (2008) Pregabalin overdose with benign outcome. Clinical toxicology (Philadelphia, Pa) 46(9): 917.
- Stannard C (2013) Opioids in the UK: what is the problem? British Medical Journal 15: 347.
- Tjandrawinata RR, Setiawati E, Putri RSI, Gunawan VA, Ong F (2015) Pharmacokinetic equivalence study of two formulations of the anticonvulsant pregabalin. Clinical pharmacology: advances and applications, 7: 69-75.
- Wood DM, Berry DJ, Glover G, Eastwood J, Dargan PI (2010) Significant pregabalin toxicity managed with supportive care alone. Journal of medical toxicology 6(4): 435-437.

 Mini Review
Mini Review