Summary
Introduction: The cryptogenic organizing pneumonia (COP) forms part of the interstitial lung diseases that are rare in pediatrics.
Clinical case: We report the case of a six-month-old female infant with respiratory symptoms of 2 months of evolution after a lower respiratory tract infection. The clinical, radiologic and histopathologic correlations are presented.
Conclusion: The COP is uncommon in pediatrics; therefore, the proper approach during the admission helps us to differentiate from other interstitial diseases that are difficult to diagnose at this age.
Keywords: Pneumonia; Organizing; Cryptogenic; Computerized Axial Tomography; Biopsy
Abbreviations: COP: Cryptogenic Organizing Pneumonia; CAT: Computerized Axial Tomography; ARI: Acute Respiratory Infection; BAL: Bronchoalveolar Lavage
Introduction
Cryptogenic Organizing Pneumonia (COP) is a rare disease in pediatrics. It was described in 1985 as organizing pneumonia and its origin is cryptogenic because it has diverse etiologies; usually its presentation is subacute manifested with tachypnea, cough, dyspnea and hypoxemia. The disease is considered as a diagnosis of exclusion since the tomographic findings are variable. Also, the histopathology is important as it is required to confirm the diagnosis.
Clinical Case
This report presents the case of a six-month-old female patient, product of the first pregnancy of her 18-year-old mother, with complete immunizations up to two months of age. Between the second and the third month of life, the patient stopped gaining weight gain, and presented dyspneic and wheezing events with diaphoresis associated with recurring breastfeeding. Because of this, she is taken toa first-level consultation where she received treatment with antitussives, expectorants, antipyretics, antiviral drugs and antibiotics on three occasions. At the fourth month, the patient is hospitalized due to the presence of wheezing without fever and respiratory difficulty treated with bronchodilators and inhaled steroids. Because the intermittent tachypnea and wheezing persisted, adding cyanotic events, she was taken to urgent care at six months of age. The physical examination showed the following parameters: weight 5 kg, height 60cm, heart rate 170 bpm, respiratory rate 52 bpm, temperature 36.6°C, 87% saturation, peripheral cyanosis, thorax with intercostal retractions, suprasternal retractions, nasal flaring, bilateral bronchoalveolar rales, expiratory wheezing, dynamic precordium with systolic murmur Grade II/VI, hepatomegaly 2x2x1cm, and capillary refill of 2 seconds. Upon her admission a chronic lung disease approach is performed as well as laboratory tests that reported Hemoglobin 15.5 g/dl, Hematocrit 43% Leukocytes 8800 x103/ml, Neutrophils 46%, Lymphocytes 25%, Monocytes 11%, Platelets 245,000. IgG 1020 mg/dl, IgM, 114 mg/dl, IgA 60mg/dl, PCR 0.34 mg/dl, antinuclear antibodies and negative anticytoplasmic antibodies, HIV-negative. Thorax Radiography (Figure 1).
Figure 1: AP Thorax Radiography, which shows increased density and thickness of the parahilar bilateral region; in addition to parahilarbilateral consolidation zones predominant on the right side.
Electrocardiogram with biventricular growth, echocardiogram with interatrial septum growth of 4mm, pulmonary pressure of 26 mmHg. Gastroesophageal reflux approach with negative pH metry for reflux. The patient persisted with increased work of breathing and wheezing episodes in spite of bronchodilators and inhaled steroids; therefore, a thoracic CAT scan is performed (Figures 2-4).
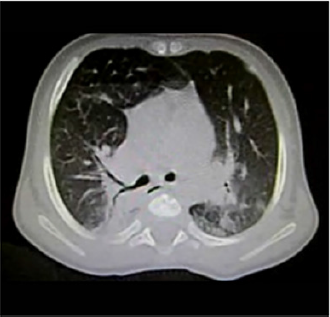
Figure 2: Axial cut in single phase tomography, with lung parenchyma window, showing the presence of groundglass areas toward the upper segment of the left lower lobe and rightparahilar consolidation zones with air bronchogram.
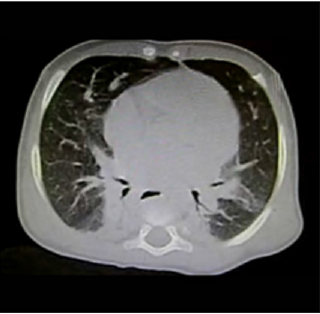
Figure 3: Ground-glass pattern is observed toward the apical segment of the right upper lobe, with adjacent consolidation; on the left-hand side it is worth the attention the reversed halo sign or the atoll sign, considered as the most specific sign for cryptogenic pneumonia.
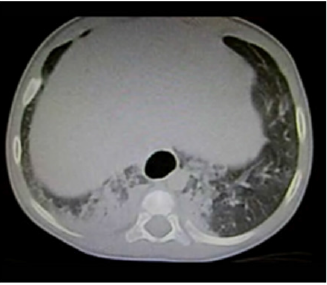
Figure 4: Thick consolidation zones of right subpleural predominance in addition to ground-glass areas, which confer a crazy paving pattern.
Because of the persistent clinical findings of poor response and the observed results in the imaging as an approach for chronic lung disease with interstitial condition, it was decided to perform a bronchoscopy and a lung biopsy. These tests reported hypersecretion of mucus, negative cytology of Bronchoalveolar Lavage (BAL) for lipophages, negative bronchial culture, and bronchial brushing with no specific pattern. From the histopathological standpoint, collapsed and over-distended lungs with epithelial hyperplasia were observed as well as regional desquamation of alveolar macrophages with no specific pattern of lung damage. The immunohistochemistry in biopsy showed CD68+ in macrophages and CD34+ in vessels. The patient was dispatched to her home being with oxygen therapy, prednisolone 0.5mgk ioand inhaled therapy.
Discussion
The COP belongs to the group of interstitial lung diseases characterized by abnormal remodeling of the distal airway that can cause alterations in the ventilation and gas diffusion, it is the idiopathic form of an organizing pneumonia [1]. While the prevalence in pediatrics [2] is unknown, the incidence series of adults has been observed from 2%occupying up to 7% of pulmonary interstitial diseases [3,4].
It can be associated with viral infections that play an etiologic role in lung transplants, radiation, chemotherapy, medications, and autoimmune diseases [5-7]; In this clinical case, the patient presented at two months of age ARIs of undetermined origin, likely viral. There are isolated cases of COP due to broncho aspiration associated with gastroesophageal reflux disease [8], but this was ruled out in our patient because of the negative pH metry for reflux and the absence of lipid-loaded macrophages in the BAL. The increase in the work of breathing is the most common manifestation that may occur in 75-93% of cases. On the other hand, cough, dyspnea and hypoxemia are more common suggestive data in patients with interstitial lung disease, and pulmonary insult [2]. In this case, due to the chronic respiratory symptoms the patient was approached for a chronic lung disease from the interstitial [9] sphere. There are isolated fulminant COP cases described that have come to require ventilation with extracorporeal membrane oxygenation machine as part of the treatment [10]. The BAL usually show an increase in the cellularity with predominance of lymphocytes and a slight elevation of neutrophils [11]. From the histopathological standpoint, it is characterized by myofibroblasts deposits and peribronchial connective tissue involving the small airways, alveolar ducts and chronic inflammation with cellular infiltration of the alveolar wall [12]. The immunohistochemistry reported the expression of CD34+, a cell with a potentialized surface in angiogenesis [13,14] processes and macrophages with expression of CD68+ observed in pediatric patients with severe pneumonias [15] and in macrophages of idiopathic interstitial pneumonias [16]. The Computed Axial Tomography is indispensable and the best diagnostic tool in patients with interstitial disease with increased work of breathing of torpid evolution. There is no specific tomographic pattern; the dominant pattern are multiple areas of consolidation or ground-glass located in the subpleural and peri bronchovascular areas, predominantly in both bases [17] such as in the present case. The tomographic patterns can have migration tendencies and affect other lobe [18] sites. The differential tomographic diagnosis includes lymphoma, eosinophilic lung diseases, vasculitis, and sarcoidosis [3]. There are cases described with spontaneous resolution [19], but immunosuppresive pharmacotherapy has been reported to be useful in intersticial lung deseases in child [2] as in our case.
Conclusion
Criptogenic organizing pneumonia is uncommon in pediatrics, its etiology is diverse, being the post infectious origin the most common cause. The clinical case represents the approach for chronic lung condition with interstitial disease, observing the most frequent respiratory interstitial symptoms in infants, and correlating with the CAT and the histopathological report. The utility of steroids in early stages can decrease interstitial damage and improve prognosis. Interstitial diseases should be suspected in healthy infant patients with unfavorable evolution.
Conflict of Interest
The authors declare they have no conflict of interest.
References
- Cordier JF (2006) Cryptogenic organising pneumonia. Eur Respir J 28(2): 422-446.
- Kurland G, Deterding RR, Hagood JS, Young LR, Brody AS, et al. (2013) An official american thoracic society clinical practice guideline: Classification, evaluation, and management of childhood interstitial lung disease in infancy. Am J Respir Crit Care Med 188(3): 376-394.
- Petitpierre N, Beigelman C, Letovanec I, Lazor R (2016) Cryptogenic organizing pneumonia. Rev Mal Respir 33(8): 703-717.
- Pedraza-Serrano F, Jiménez-García R, López-de-Andrés A, Hernández-Barrera V, Sánchez-Muñoz G, et al. (2019) Characteristics and outcomes of patients hospitalized with interstitial lung diseases in Spain, 2014 to 2015. Medicine (Baltimore) 98(21): e15779.
- Elbahlawan L, Rains KJ, Stokes DC (2017) Respiratory care considerations in the childhood cancer patient. Respir Care 62(6):765-775.
- Mengoli MC, Colby TV, Cavazza A, Zanelli M, De Marco L, et al. (2018) Incidental iatrogenic form of collagenized organizing pneumonia. Hum Pathol 73: 192-193.
- Labarinas S, Gumy-Pause F, Rougemont AL, Baerlocher G, Leibundgut EO, et al. (2013) Is acute fibrinous and organizing pneumonia the expression of immune dysregulation? J Pediatr Hematol Oncol 35(2): 139-143.
- Liu JR, Xu XF, Zhou CJ, Yang HM, Zhao SY (2015) Bronchiolitis obliterans organizing pneumonia due to gastroesophageal reflux. Pediatrics 135(6): e1510-1513.
- Sansores Martínez R, Pérez Fernández L, Cuevas Schacht F (2004) First national consensus for the study of children with chronic lung disease. Mexican Society of Pneumology and Chest Surgery. Mexico Pediatric Act 25(3): 193-200.
- Sayad E, Coleman RD, Silva-Carmona MD (2020) Diagnosis and treatment of cryptogenic organizing pneumonia in a child on ECMO. Pediatr Pulmonol 55(1): 20-22.
- Hisatomi K, Sakamoto N, Mukae H, Hayashi T, Amenomori M, et al. (2009) Elevated levels of tenascin-C in patients with cryptogenic organizing pneumonia. Intern Med 48(17): 1501-1517.
- Lee JW, Lee KS, Lee HY, Chung MP, Yi CA, et al. (2010) Cryptogenic organizing pneumonia: Serial high-resolution CT findings in 22 patients. Am J Roentgenol 195(4): 916-922.
- Rakocevic J, Orlic D, Mitrovic-Ajtic O, Tomasevic M, Dobric M, et al. (2017) Endothelial cell markers from clinician’s perspective. Exp Mol Pathol 102(2): 303-313.
- Abe SI, Suzuki M, Cho KH, Murakami G, Cho BH, et al. (2011) Cd34-positive developing vessels and other structures in human fetuses: An immunohistochemical study. Surg Radiol Anat 33(10): 919-927.
- Cotoi CT, Turdean SG, Turcu ML, Pop OL, Baba DF, et al. (2019) Lung injury patterns in newborns, infants and young children-morphological and immunohistochemical approaches. Rom J Morphol Embryol 60(4): 1153-1161.
- Yamashita M, Saito R, Yasuhira S, Fukuda Y, Sasamo H, et al. (2018) Distinct Profiles of CD163-Positive Macrophages in Idiopathic Interstitial Pneumonias. J Immunol Res 2018:
- Verma N, Altmayer S, Hochhegger B, Barros MC, Rajderkar D, et al. (2020) ChILD: A Pictorial Review of Pulmonary Imaging Findings in Childhood Interstitial Lung Diseases. Curr Probl Diagn Radiol.
- Jara-Palomares L, Gomez-Izquierdo L, Gonzalez-Vergara D, Rodriguez-Becerra E, Marquez-Martin E, et al. (2010) Utility of high-resolution computed tomography and BAL in cryptogenic organizing pneumonia. Respir Med 104(11): 1706-1711.
- Abi-Khalil S, Fadel N, Menassa-Moussa L, Torbey PH, Haddad-Zebouni S (2016) Spontaneous resolution of cryptogenic organizing pneumonia in pediatrics: A case report. Arch Pediatr 23(5): 519-522.

 Case Report
Case Report