Abstract
We report a case of giant frontal intraparenchymal schwannoma in a 17 years old male who had initial symptoms of partial seizure without neurological deficit. Bone remodelling manifested as thinning of cortical bone overlying the tumour was noted which was not reported in previous intraparenchymal schwannomas.
Keywords: Intraparenchymal schwannoma; Frontal schwannoma; Huge schwannoma; Bone remodelling
Introduction
Intracranial schwannomas account for 8% of all primary brain tumours [1] and are derived from Schwann cells in the peripheral nervous system. Schwannomas constitute more than 80% of cerebellopontine angle tumours and are derived from the vestibular portion of the VIII cranial nerve. However, Intraparenchymal schwannomas that are not associated with cranial nerves are extreme rare. The symptoms in patients with intraparenchymal schwannoma include seizure, headache or focal neurologic deficits. Mostly, patients with intracranial schwannomas are diagnosed in the first or second decade of life. The surgical outcome is relatively good and curative. The most common location of the intraparenchymal schwannoma is over the frontal and tem-porooccipital area from previous case reports [2]. We report a case of a giant frontal intraparenchymal schwannoma in a 17-year-old male.
Case report
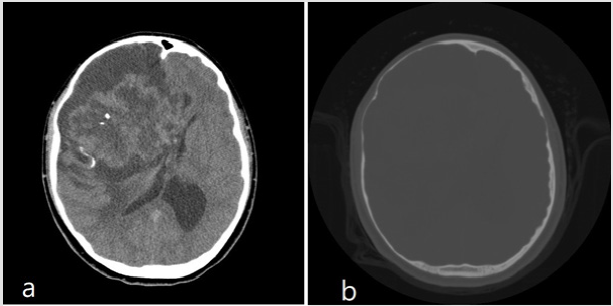
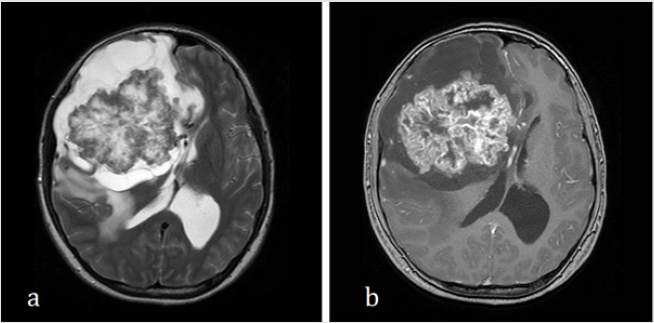
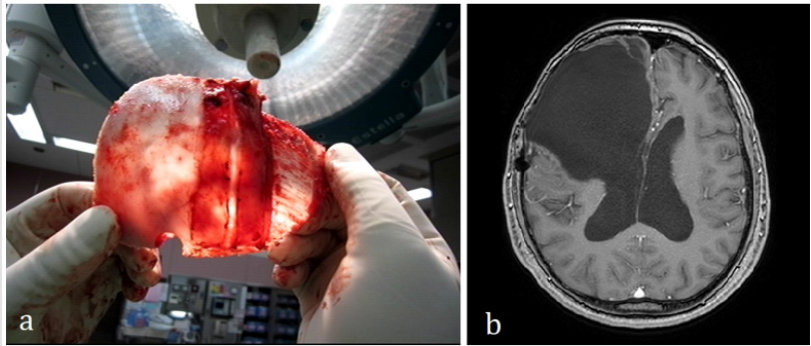
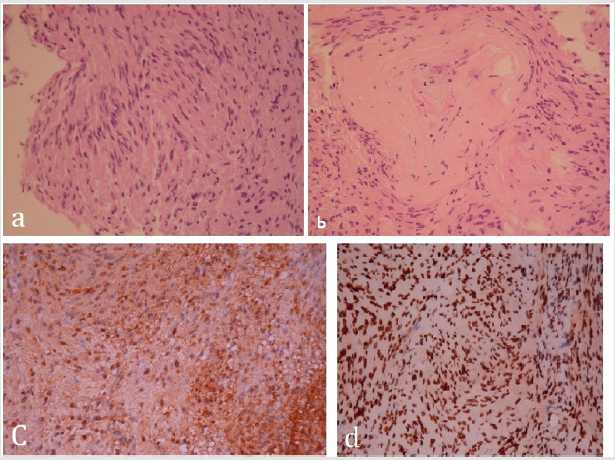
This 17-year-old male patient encountered three episodes of partial seizures over a period of one month with upward gaze, tonic posture over left side and saliva drooling. He was admitted to our institute for evaluation. Physical examination did not reveal neurological deficit, neurocutaneous markers or other physical abnormality. He and his family members denied a history of neurofibromatosis. Brain CT showed a large lobulated mass in the right frontal lobe with intra-tumoral calcification causing right-toleft shift of midline structure (Figure 1). T2-weighted MRI showed a 13 x 10 x 10 cm tumour with septate cystic part surrounding the main tumour with significant perifocal edema, the solid component enhanced heterogeneously with gadolinium which invaded into the corpus callo-sum at the genu of body (Figure 2) The patient received right frontal craniotomy and total excision of tumour with iCT navigation and CUSA aid. The skull bone overlying the tumour was noted to be very thin during craniotomy (Figure 3). Cysts with multiple septa filled with xantho chromic fluid and gel-like material was noted at the periphery of the tumour. After removal of the cystic part of the tumour, the tumour plane was well identified. The solid portion of the tumour was soft in consistency, white in colour, and had moderate vascularity and scattered calcifications. Follow up MRI at 4 years post-surgery showed no recurrence or residual tumour (Figure 3). Histopathological examination of the resected material disclosed the tumour cells that are s-100 protein (+), neurofilament (+), vimentin (-), EMA (-), GFAP (Equivocal), and MIB-1 (Trace) (Figure 4). Microscopically the tumour displayed areas of antoni A and antoni B, therefore, it is consistent with schwannoma.
Patient
Case Report
Figure 1: a. Non-enhanced brain CT showed a right frontal tumour with internal calcification and right-to-left shift of midline
structure.
b. bone window showed right frontotemporal cortical bone scalloping.
Figure 2: a. T2-weighted MRI showed septate cystic part surrounding solid part tumor with perifocal edema. b. T1-weighted gadolinium-enhanced MRI showed heterogenous enhancement of the solid part tumor.
Figure 3: a. Paper thin cortical bone. b. Follow up post-operative T1-weighted MRI 4 years later showed no recurrence of tumor.
Figure 4: Photomicrography showed a. spindle cell elongated nuclei and fibrillary cytoplasms (antoni A). b. Paucicellular with loose edematous and mucinous stroma (antoni B). C. S-100 diffusely positive d. Positive in neurofilament.
Discussion
Intraparenchymal schwannomas have been reported in the
cerebral hemisphere, sub-frontal, cerebellum, brainstem, sella
and in the fourth ventricle [3]. To our knowledge, this giant
intraparenchymal schwannoma measuring 13 x 10 x 10cm is the
largest volume compared with reported articles [4]. Currently the
origin of intraparenchymal schwannoma remains controversial.
Menku et al. divided these theories into 2 categories according
to histogenesis: developmental and non-developmental groups
[5]. Developmental theories postulate that tumour develops from
aberrant neural crest cells within the central nervous system or
ectodermal Schwann cells transformed from mesenchymal pial
cells [6]. Non-developmental theories assume that Schwann cells
from adjacent structures give rise to intracranial schwannoma [7].
Despite of the large tumour size and attack of seizure, our patient
did not have neurological deficits. The skull bone surrounding this
tumour had remodelled into paper-thin cortical bone possibly
due to long term compression by the tumour and this finding has
not been reported in previous intraparenchymal schwannomas.
We assume that these phenomena are due to the slow growing
characteristic of this large intraparenchymal schwannoma.
Skull bone remodelling and thinning has rarely been reported
due to intraparenchymal tumour, smooth cortical expansion and
remodelling with cortical thinning is usually associated with
benign slow growing processes [8] such as, porencephalic cysts or
arachnoid cysts. Like in previous report, intracranial schwannomas
mostly occur in children and young adults [9], which when coupled
with the slow growing process, it might be congenital in nature,
although current evidence remain uncertain. In comparison of our
case to those reported, the developmental theory is more likely, due
to the young age of diagnosis and cortical bone scalloping from the
chronic increase in intracranial pressure and tumour compression
[10], however, there are only few molecular and histological
evidence to support this theory, thus further studies are warranted.
References
- Rotondo M, Pascale M, Scuotto A (2013) Giant frontal intraparenchymal schwannoma: unexpected diagnosis. BMJ case reports.
- Paredes I, Jimenez Roldán L, Ramos A, Lobato RD, Ricoy JR (2012) Intraparenchymal schwannomas: report of two new cases studied with MRI and review of the literature. Clinical neurology and neurosurgery114(1):42-46.
- Luo W, Ren X, Chen S, Liu H, Sui D, et al. (2013) Intracranial intraparenchymal and intraventricular schwannomas: report of 18 cases. Clinical neurology and neurosurgery 115(7):1052-1057.
- Gao Y, Qin Z, Li D, Yu W, Sun L, et al. (2018) Intracerebral schwannoma: A case report and literature review. Oncology letters16(2):2501-2510.
- Menku A, Oktem IS, Kontas O, Akdemir H (2009) intracerebral schwannoma mimicking glial tumor: case report. Turkish neurosurgery 19(1):82-85.
- Tsuiki H, Kuratsu J, Ishimaru Y, Nakahara T, Kishida K, et al. (1997) Intracranial intraparenchymal schwannoma: report of three cases. Acta neurochirurgica139(8):756-760.
- Viale E PA, Turtas S M(1973) Olfactory groove neurinomas. Journal of Neurosurgical Sciences17:193-196.
- Raut AA, Naphade PS, Chawla A (2012) Imaging of skull base: Pictorial essay. The Indian journal of radiology & imaging 22(4):305-316.
- Khursheed N, Rumana M, Ramzan A, Furqan N, Abrar W, et al. (2011) Frontal intraparenchymal schwannoma. Journal of Clinical Neuroscience 18(3):411-413.
- Eric MHorn JMZ, GuiseppeLanzino, Stephen WCoons (2006) Intracerebral Schwannomas: Case Report and Review of the Literature. Barrow Quarterly22(2).

 Case Report
Case Report