Case Report
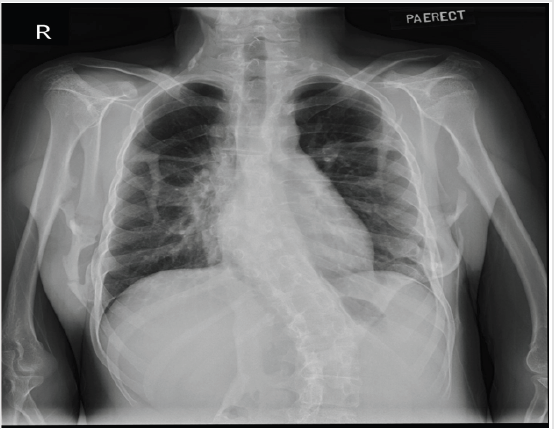
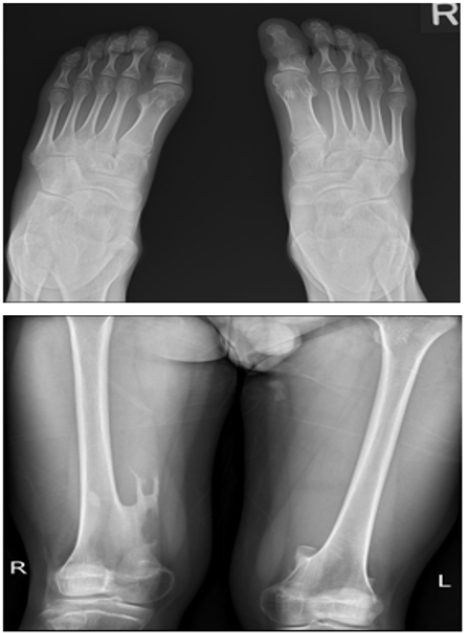
A 15-year-old boy presents with a history of multiple lumps since the age of 3 which are slowly progressing. He was the second child of non-consanguineous parents with no past medical history. The lumps were first noted on his head, and subsequently on his neck and back. By the age of 6, the lumps on his upper back had increased in size to the point where he became permanently kyphotic. By the time of presentation at age 13, his neck lumps had limited neck rotation to 20-30 degrees to either side. Upon examination, there were multiple lumps along the right axilla, posterior neck, back and extremities. He had kyphosis and levoscoliosis as well as limitation of movement, particularly in the axial skeleton. A series of radiographs taken are shown in Figures 1A-1C, illustrating the constellations of findings typical of FOP. Fibrodysplasia ossificans progressiva is a rare and disabling genetic condition characterized by congenital malformation of the great toes and by progressive heterotopic ossification in specific anatomic patterns [1]. The worldwide prevalence is approximately 1 in 2 million people with no ethnic, racial, gender or geographic predilection.
Figure 1A: Erect chest radiograph showing multiple ossifications arising from the ribs, scapula and chest wall. Focal ossification was seen in the right paraspinal region resulting in scoliotic deformity at the lower thoracic vertebrae. There is also an associated fracture of the ossifications in the right lateral chest wall.
Figure 1B: Lateral neck radiograph showed the typical appearance of the cervical spine in FOP, characterised by large spinous processes and pedicles, tall and narrow vertebral bodies as well as fusion of the facet joints between C2 and C5. Thickening and ossification of the nuchal ligament also noted.
The majority of cases are due to sporadic mutation of the ACV1 protein, although autosomal dominant inheritance pattern with variable penetrance has also been reported. The ACV1 protein aids in controlling the growth and development of bones and muscles, including the gradual replacement of cartilage by bone [2]. Deformities of the great toes, characterised by short and monophalangic great toe are distinctive and are usually the only abnormality that is seen at birth [3]. This will then be followed by sporadic episodes of painful soft tissue swelling over the first decade of life as experienced by our patient. These flareups transform skeletal muscles, tendons, ligaments, fascia and aponeuroses into the heterotypic bone which over time will impose restrictions of normal movement. These heterotopic ossifications in the soft tissues would follow an expected anatomic and temporal pattern with sternocleidomastoid muscle often being the initial site. It will usually then progress to shoulder girdle, upper arms, spine and pelvis. The main differential diagnosis for FOP is that of Klippel-Feil syndrome, as most patients present with neck stiffness and decreased range of motion of the cervical spine in the first decade of life. Although both FOP and Klippel-Feil patients display malformations of the cervical spine, they do not exhibit the same defects. A previous study by Schaffer and colleagues [4] has shown that the cervical spine of FOP patients consists of narrow vertebral bodies, enlarged pedicles and large spinous processes, as well as fusion of the facet joints between C2 and C7.
FOP patients have a progressive degree of fusion of the posterior elements with no occipitalization observed (fusion between the occiput and C2). Klippel-Feil syndrome is characterised by cervical fusion, low hairline and short neck. It results from disruption of vertebral segmentation in a variable manner. The findings of small vertebral bodies with large pedicles and spinous processes are not seen. There has been a previous study which suggested up to 90% misdiagnosis of these patients and up to 67% of patients being subjected to potentially harmful invasive diagnostic procedures that can cause lifelong disability in these patients [5]. Differentiating between cervical spine findings of FOP and Klippel Feil syndrome would also reduce the risk of misdiagnosis in these patients. This case serves as a good reminder of this rare diagnosis and the importance of recognizing its clinical features and radiological findings to aid in its early diagnosis, thus prevent invasive diagnostic or therapeutic interventions which would be harmful to the patient. Unfortunately, to date there is no cure for the disease with a median life expectancy of 40 years [1] and death is usually due to respiratory compromise. Treatment currently is targeted to minimize the formation of new ossification during a flare-up.
References
- Kaplan FS, Xu M, Glaser DL, Collins F, Connor M, et al. (2008) Early diagnosis of fibrodysplasia ossificans progressiva. Pediatrics 121: e1295-e1300.
- Bauer AH, Bonham J, Gutierrez L, Hsiao EC, Mohamedi D (2018) Fibrodysolasia ossificans progressiva: A current review of imaging findings. Skeletal Radiol 47(8): 1043-1050.
- Maftei C, Rypens F, Thiffault I, Dube J, Laberge AM, et al. (2015) Fibrodysolasia ossificans progressiva: Bilateral hallux valgus on ultrasound a clue for the first prenatal diagnosis for this condition-clinical report and review of the literature. Prenat Diagn 35(3): 305-307.
- Schaffer AA, Kaplan FS, Tracy MR, O’Brien ML, Dormans JP, et. al. (2005) Developmental anomalies of the cervical spine in patients with Fibrodysplasia Ossificans Progressive are distinctly different from those in patients with Klippel-Feli Syndrome. Spine 30(12): 1379-1385.
- Kitterman JA, Kantanie S, Rocke DM, Kaplan FS (2005) Iatrogenic Harm Caused by Diagnostic Errors in Fibrodysplasia ossificans Progressiva. Paediatrics 116(5): 654-661.

 Case Report
Case Report