Abstract
Background: Bacterial conjunctivitis represents the major part of infectious conjunctivitis and, although it generally shows a spontaneous resolution, antibiotics speed the elimination of bacteria from the conjunctiva thus limiting the duration of the disease. The addition of anti-inflammatory drugs may potentiate the effectiveness of antibiotics in eradicating bacterial conjunctivitis. Aim of the present study is to compare the efficacy of two different eye drops based on ofloxacin without or with dexamethasone against bacterial conjunctivitis induced by Staphylococcus aureus or Pseudomonas aeruginosa.
Methods: S. aureus or P. aeruginosa were inoculated in the palpebral conjunctiva of New Zealand rabbits. Twenty-four hours after bacteria inoculation, rabbits started treatment with eye drops containing saline, 0.3% ofloxacin or 0.3% ofloxacin/0.1% dexamethasone (5 times a day for 3 days). Animals were evaluated for pathology at specific times post infection using a clinical score. Tear levels of two inflammatory cytokines, interleukin (IL)-6 and (TGF)-ß, were quantified by ELISA.
Results: Saline-treated rabbits showed a slow regression of the infection that was still present 96 hours after bacteria inoculation. On the contrary, in ofloxacin-treated rabbits, infective processes completely disappeared 72 hours after starting the treatment with a major efficacy of ofloxacin eye drops added with dexamethasone. Ofloxacin eye drops also reduced the infection-induced increase in tear levels of IL-6 and TGF-ß with greater effectiveness in the presence than in the absence of the corticosteroid.
Conclusion: The addition of dexamethasone to ofloxacin results in a significative reduction of the bacterial infection indicating that the combination of a fluoroquinolone with a corticosteroid may accelerate disease resolution thus helping to minimize the potentially dangerous effects of bacterial conjunctivitis. Although results in animals cannot be directly translated to humans, the stringency of the rabbit model proposed here to the human disease supports the translatability of these findings to clinical settings.
Introduction
The conjunctiva is a highly vascularized and innervated layer of mucosal tissue playing an important role in eye lubrication and protection through the production of mucus and tears, and the prevention of microbial entrance [1]. A number of pathologic conditions affects the conjunctiva, the most common being conjunctivitis. Among the different forms of conjunctivitis, bacterial conjunctivitis, which contributes for about 50-70% of infectious conjunctivitis, is one of the most commonly observed diseases in ophthalmic clinics [2]. Many types of pathogens may cause bacterial conjunctivitis. Staphylococcus aureus is a Gram-positive organism mainly involved in acute conjunctivitis, although Pseudomonas aeruginosa, a Gram-negative bacterium, may also be responsible for acute forms of the disease [3]. Patients developing conjunctivitis also develop an inflammatory status leading to the production of high levels of inflammatory cytokines in tears, including interleukin (IL)-6, and Transforming Growth Factor (TGF)-ß [4-6]. Generally, acute bacterial conjunctivitis is a self-limiting disease, with spontaneous resolution within 7-10 days after infection, although in some cases the disease may go on to become chronic [7].
Therapies using antibiotics have been shown to limit the duration of the disease and to speed the elimination of bacteria from the conjunctiva [3]. Presently, the treatments for bacterial infections of the ocular surface, including conjunctivitis, are largely empirical. Antibiotics such as fluoroquinolones because of their broad-spectrum antibacterial activity, documented safety and lack of toxicity are well suited to treat bacterial conjunctivitis [8]. Among fluoroquinolones, ofloxacin, a second-generation fluoroquinolone, is used as eye drops in the treatment of this disease, although additional fluoroquinolones of third or fourth generation with higher activity in respect to ofloxacin have been introduced in the market [9]. Combining antibiotics with additional drugs counteracting inflammatory processes associated to bacterial infection may be useful to potentiate the treatment. In this respect, corticosteroids, which are already extensively used against inflammatory ocular diseases, show the potential to treat acute conjunctivitis in combination with approved therapies, and formulations of antibiotics with dexamethasone are in clinical use or under clinical investigation [10]. In the present study, we compared the efficacy of two different eye drops based on ofloxacin without or with dexamethasone against bacterial conjunctivitis induced by S. aureus or P. aeruginosa in a rabbit model. In particular, a qualitative evaluation of the infection progression was performed on photograph images of the rabbit eyes taken at different time points after infection, while semi-quantitative assessment was made using a previously reported clinical score [11]. Whether the addition of dexamethasone may potentiate the anti-inflammatory activity of ofloxacin was also investigated by evaluating IL-6 and TGF-ß levels in tears.
Methods
Strains
S. aureus strain ATCC 6538, isolated from a human lesion, and P. aeruginosa strain ATCC 9027, isolated from outer ear infection, both ofloxacin sensitive, were obtained by ATCC (Manassas, VA, USA). Strains were stored at -80°C in Luria Bertani (LB) broth (Fisher Scientific, Rodano, Milan, Italy) supplemented with 40% glycerol (v/v), and sub-cultured on LB agar (Fisher Scientific, Rodano, Milan, Italy) at 37°C when necessary. Bacterial pre-inoculum was prepared in 5 mL of fresh LB broth, by picking a single colony which was incubated at 37°C under agitation at 220 rpm overnight. Next day, overnight bacterial culture was diluted in fresh LB broth and then grown for 3 hours to reach the exponential phase.
Experimental Conjunctivitis
New Zealand white rabbits (n = 18) were purchased from Azienda Agricola Pampaloni (Fauglia, Italy). All animals were maintained in agreement to institutional guidelines of the ARVO Statement for the Use of Animals in Ophthalmic and Vision Research, the European Communities Council Directive (2010/63/UE) and the Italian guidelines for animal care (DL 26/14). The experimental protocol was approved by the Commission for Animal Wellbeing of the University of Pisa. Before bacteria inoculation, rabbits were anesthetized with Zoletil 50 (Tilentamin + Zolazepam; Virbac Laboratories, Carros, France). Bacteria in exponential phase were grown to 2 × 107 colony forming units (CFU)/mL. The palpebral conjunctiva of both eyes was injected with 100 μL of 2 × 106 CFU of either S. aureus or P. aeruginosa diluted in sterile phosphate buffered saline (n = 9 per group). Twenty-four hours after bacteria inoculation, rabbits started treatment with saline, 0.3% ofloxacin or 0.3% ofloxacin/0.1% dexamethasone (n = 3 per group, inoculated with either S. aureus or P. aeruginosa). Rabbits received 30 μL eye drops per eye 5 times a day (every 2 hours, starting at 9 o’clock) for 3 days. Animals were evaluated for pathology at specific times after bacterial inoculation. At the same times, tear samples were collected from each eye and stored at -80°C for subsequent ELISA analyses.
Clinical Score
A semi-quantitative evaluation of the infection progression was performed by using a previously published clinical score with minor modifications [11]. Briefly, 2 parameters, hyperemia and the presence of purulence, were considered. For each parameter, a grading scale ranging from 0 to 3 (0, absence of symptom; 1, detectable; 2, intermediate; 3, maximal) was used. The sum of average scores for each eye at each time point was plotted to generate the clinical index.
Enzyme-Linked Immunosorbent Assays
Quantification of IL-6 and TNF-β protein levels was performed using commercially available kits (MyBioSource, San Diego, CA, USA) according to the manufacturers’ instructions. ELISA plates were evaluated spectrophotometrically (Microplate Reader 680 XR, Bio-Rad Laboratories, Hercules, CA, USA). Data were expressed as pg/mL. All experiments were performed in duplicate.
Statistical Analysis
Statistical significance was evaluated with Prism 8.02 (GraphPad Software, Inc., San Diego, CA, USA) using Two-way analysis of variance (ANOVA) followed by Bonferroni’s multiple comparison post-test. After statistical analysis, the data from different experiments were plotted and averaged in the same graph. Results were expressed as the mean ± S.E.M. of the indicated n values. Differences with P<0.05 were considered significant.
Results
Effects of Ofloxacin on Bacterial Conjunctivitis
The effectiveness of two different ofloxacin-based eye drops, formulated without or with dexamethasone, was investigated in rabbit models of bacterial conjunctivitis induced by either S. aureus or P. aeruginosa. As shown in Figure 1, eye infection could be observed 12 hours after bacteria inoculation. Twenty-four hours after bacteria inoculation, rabbits were treated with sterile saline or the antibiotic in the absence or in the presence of dexamathasone. In sterile saline-treated rabbits the infection slowly regressed but was still present 96 hours after inoculation (i.e. 72 hours after starting the treatment), while ofloxacin-containing eye drops caused a faster regression of infective processes that completely disappeared 72 hours after starting the treatment. The qualitative analysis was supported by the evaluation of a clinical score. The clinical indexes are shown in Figures 2 (S. aureus) & 3 (P. Aeruginosa). At 72 hours after inoculation of S. aureus or P. aeruginosa (i. e. 48 hours after starting the treatment) ofloxacin was more effective in the presence than in the absence of dexamethasone in reducing the clinical index independently on the bacterium used to induce eye infection.
Figure 1: Representative pictures of rabbit eyes infected with either Staphylococcus aureus or Pseudomonas aeruginosa and treated with sterile saline or ofloxacin without or with dexamethasone. Saline treatment caused a slow regression of the infection, while ofloxacin-containing eye drops, without or with dexamethasone, determined a regression of infective processes that completely disappeared 72 h after starting the treatment (96 h after bacteria inoculation).
Figure 2: Evaluation of the clinical index in rabbits infected with S. aureus. Ofloxacin improved infection regression with a greater effectiveness in the presence of dexamethasone. Circles, saline; squares, ofloxacin; triangles, ofloxacin/dexamethasone. *P<0.001 ofloxacin or ofloxacin/dexamethasone versus saline; #P<0.001 ofloxacin/dexamethasone versus ofloxacin (Two-way ANOVA followed by Bonferroni post-hoc test).
Figure 3: Evaluation of the clinical index in rabbits infected with P. aeruginosa. Ofloxacin improved infection regression with a greater effectiveness in the presence of dexamethasone. Circles, saline; squares, ofloxacin; triangles, ofloxacin/dexamethasone. *P<0.001 ofloxacin or ofloxacin/dexamethasone versus saline; #P<0.001 ofloxacin/dexamethasone versus ofloxacin (Two-way ANOVA followed by Bonferroni post-hoc test).
Effects of Ofloxacin on Inflammatory Cytokines
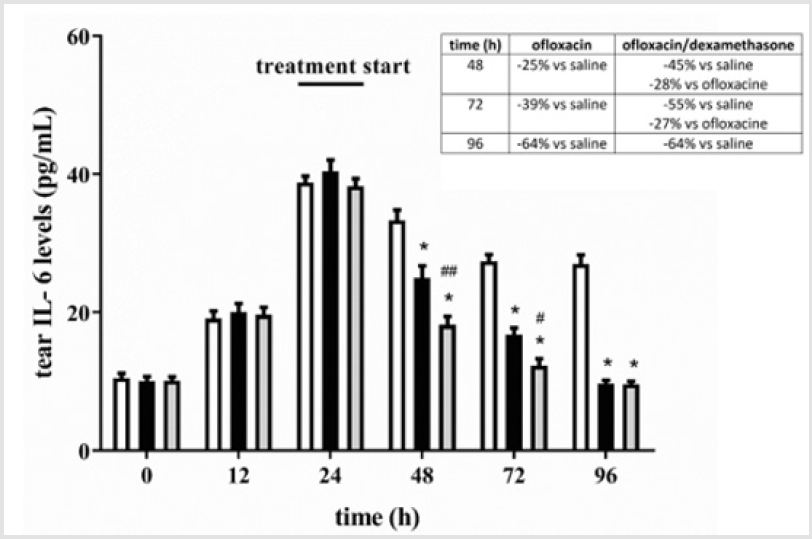
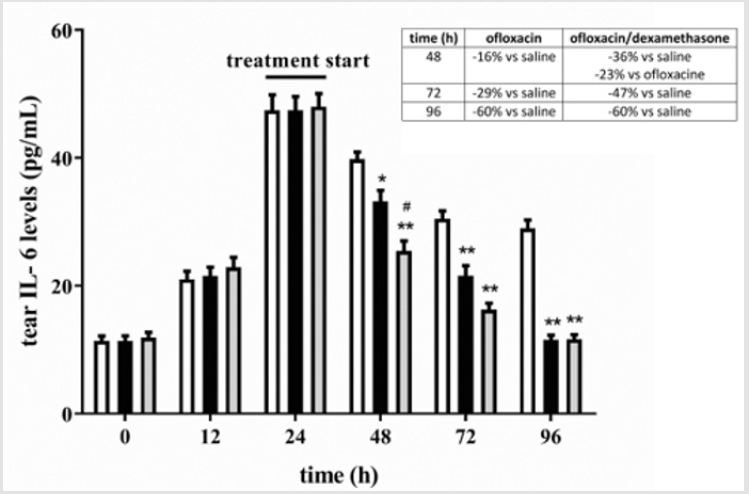
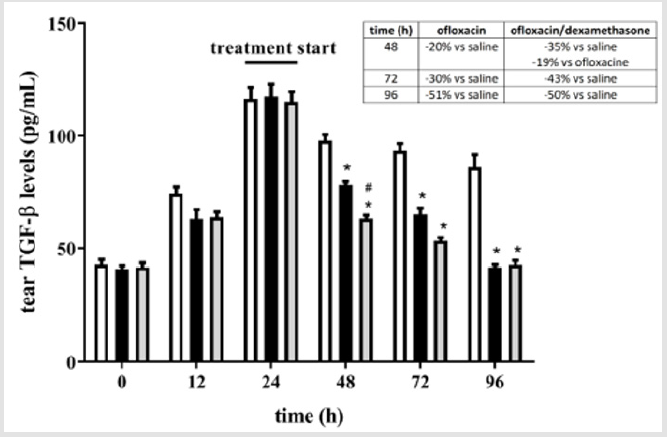
At the end of the treatment with oxofloxacin without or with dexamethasone, tears were collected and used to evaluate protein levels of two inflammatory cytokines, IL-6 and TGF-β, by ELISA assay. Results in Figures 4-7 show that eye infection developed in parallel with a gradual increase in the levels of both IL-6 (Figures 4 & 5) and TGF-β (Figures 6 & 7), independently on the bacterium used to induce eye infection. In respect to saline, ofloxacin, either without or with dexamethasone, reduced levels of inflammatory cytokines, with greater effectiveness in the presence than in the absence of the corticosteroid.
Figure 4: Levels of IL-6 in tears from rabbits inoculated with S. aureus. In respect to saline, ofloxacin, either without or with dexamethasone, reduced levels of IL-6 with a greater effectiveness in the presence of dexamethasone. White bars, saline; black bars, ofloxacin; grey bars, ofloxacin/dexamethasone. *P<0.0001 versus saline; #P<0.05 and ##P<0.001 versus ofloxacin (Twoway ANOVA followed by Bonferroni post-hoc test).
Figure 5: Levels of IL-6 in tears from rabbits inoculated with P. aeruginosa. In respect to saline, ofloxacin, either without or with dexamethasone, reduced levels of IL-6 with a greater effectiveness in the presence of dexamethasone. White bars, saline; black bars, ofloxacin; grey bars, ofloxacin/dexamethasone. *P<0.05 and **P<0.0001 versus saline; #P<0.01 versus ofloxacin (Two-way ANOVA followed by Bonferroni post-hoc test).
Figure 6: Levels of TGF-β in tears from rabbits inoculated with S. aureus.. In respect to saline, ofloxacin, either without or with dexamethasone, reduced levels of IL-6 with a greater effectiveness in the presence of dexamethasone. White bars, saline; black bars, ofloxacin; grey bars, ofloxacin/dexamethasone. *P<0.05 and **P<0.0001 versus saline; #P<0.01 versus ofloxacin (Two-way ANOVA followed by Bonferroni post-hoc test).
Figure 7: Levels of TGF-β in tears from rabbits inoculated with P. aeruginosa.. In respect to saline, ofloxacin, either without or with dexamethasone, reduced levels of TGF-β with a greater effectiveness in the presence of dexamethasone. White bars, saline; black bars, ofloxacin; grey bars, ofloxacin/dexamethasone. *P<0.0001 versus saline; #P<0.05 versus ofloxacin (Two-way ANOVA followed by Bonferroni post-hoc test).
Discussion
Whether the addition of corticosteroids to fluoroquinolones may have a beneficial role in treating bacterial conjunctivitis is a matter of debate, although formulations of antibiotics with dexamethasone are in clinical use or under clinical investigation [10]. As shown by the present findings, both S. aureus and P. aeruginosas induce an acute form of bacterial conjunctivitis in the rabbit characterized by hyperemia and purulence that spontaneously regresses. This is in line with previous findings demonstrating that almost 60% of affected people show a spontaneous regression of acute bacterial conjunctivitis within 1-2 weeks [12,13]. The conjunctiva has host defence capability mediated by goblet cells, which may counteract bacterial infections [14]. For instance, the injection of S. aureus in the rabbit conjunctiva fails to produce significant conjunctivitis due to the activation of host defences [15]. On the other hand, compared to placebo, topical application of broad-spectrum antibiotics as eye drops improves the rate of clinical remission in patients suffering from acute bacterial conjunctivitis [16]. In particular, ofloxacin is recommended in the treatment of external eye infections, including bacterial conjunctivitis, as also reported by the World Health Organization [17].
This is in line with the present results demonstrating a regression of the clinical sign of infection within 72 h after starting the treatment with 0.3% ofloxacin indicating the high effectiveness of fluoroquinolones in eradicating Gram-positive and Gram-negative bacteria from the conjunctiva. In this respect, some studies have revealed a more rapid bacterial eradication in patients treated with fluoroquinolones than in patients treated with more traditional antibiotics [18]. In addition to their antimicrobial properties, fluoroquinolones exert indeed a predominant anti-inflammatory activity [19]. For instance, besifloxacin has been shown to inhibit the production of several cytokines in human corneal epithelial cells after inflammatory damage with IL-1ß [20]. In addition, in a rat model of conjunctivitis, gatifloxacin used as ophthalmic solution significantly reduces the production of tumor necrosis factor α [21]. The present results demonstrate for the first time that the addition of 0.1% dexamethasone to 0.3% ofloxacin accelerates the resolution of conjunctiva infection indicating that corticosteroids may potentiate the antibacterial properties of fluoroquinolones. This finding is in line with the assumption that corticosteroids are widely used in the treatment of inflammatory ocular diseases [22] thus supporting their use in the treatment of bacterial conjunctivitis. In this respect, the American Academy of Ophthalmology guidelines on treatment of conjunctivitis include corticosteroids as a treatment option, also in association with additional drugs [23]. For instance, the association of the aminoglycoside antibiotic tobramycin with 0.1% dexamethasone may be used when a risk of bacterial ocular infection exists, while the association of the antiseptic povidoneiodine with 0.1% dexamethasone is under investigation for the treatment of inflammatory conditions associated with ocular infections, including conjunctivitis [10].
Among cytokines produced by immune resident cells and goblet cells in the conjunctiva and collected in tears, IL-6 levels are associated with several diseases of the anterior segment of the eye including conjunctivitis [5]. TGF-ß is a cytokine acting as a multifunctional growth factor that induces unfavorable inflammatory responses and tissue fibrosis and is involved in several pathologies of the eye [24]. As shown here, dexamethasone potentiates the ofloxacin-induced reduction of both IL-6 and TGF-ß, suggesting that corticosteroids potentiate the anti-inflammatory properties of fluoroquinolones. In ocular diseases, the combination between moxifloxacin and dexamethasone has been proven to be effective in reducing infection and inflammation associated with bacterial blepharitis in humans [25]. In addition, moxifloxacin added with dexamethasone prevents postoperative inflammation and infection following cataract surgery [26].
Most of all cases of bacterial conjunctivitis worldwide is represented by the acute form of the disease. To the best of our knowledge, this is the first demonstration that the addition of dexamethasone to ofloxacin potentiates the anti-inflammatory and anti-microbial effects of the antibiotic in a rabbit model of conjunctivitis induced by either Gram-positive or Gram-negative bacteria, thus representing a possible step forward for the use of fluoroquinolones in treating acute bacterial conjunctivitis. In particular, the fact that in the first days after starting the treatment with ofloxacin the addition of dexamethasone results in a significant reduction of the bacterial infection suggests that combining fluoroquinolones with corticosteroids may accelerate the disease resolution thus helping to minimize potential dangerous effects of bacterial conjunctivitis. The stringency of the rabbit model proposed here to the human disease supports the potential translatability of these findings to clinical settings.
Acknowledgment
The authors thank Dr. Maurizio Cammalleri and Dr. Filippo Locri for technical assistance, and Prof. Paola Bagnoli for critical reading of the manuscript. The study was supported by a grant of Sooft Italia SpA to MDM. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results.
References
- Shumway CL, Motlagh M, Wade M (2019) Anatomy, Head and Neck, Eye Conjunctiva. StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing.
- Buznach N, Dagan R, Greenberg D (2005) Clinical and bacterial characteristics of acute bacterial conjunctivitis in children in the antibiotic resistance era. Pediatr Infect Dis J 24(9): 823-828.
- Teweldemedhin M, Gebreyesus H, Atsbaha AH, Asgedom SW, Saravanan M (2017) Bacterial profile of ocular infections: a systematic review. BMC Ophthalmol 17(1): 212.
- Pelikan Z (2014) Cytokines in tears during the secondary keratoconjunctival responses induced by allergic reaction in the nasal mucosa. Ophthalmic Res 52(1): 32-42.
- Fodor M, Facskó A, Rajnavölgyi E, Hársfalvi J, Bessenyei E, et al. (2006) Enhanced release of IL-6 and IL-8 into tears in various anterior segment eye diseases. Ophthalmic Res 38(4): 182-188.
- Cook EB (2004) Tear cytokines in acute and chronic ocular allergic inflammation .Curr Opin Allergy Clin Immunol 4(5): 441-445.
- Pippin MM, Le JK (2019) Bacterial Conjunctivitis. StatPearls [Internet]. Treasure Island (FL): StatPearls publishing.
- Andriole VT (2005) The quinolones: past, present, and future. Clin Infect Dis 41 Suppl 2: S113-S119.
- Mah FS, Sanfilippo CM (2016) Besifloxacin: Efficacy and Safety in Treatment and Prevention of Ocular Bacterial Infections. Ophthalmol Ther 5(1): 1-20.
- Holland EJ, Fingeret M, Mah FS, Murray OD (2019) Use of Topical Steroids in Conjunctivitis: A Review of the Evidence. Cornea 38(8): 1062-1067.
- Langford MP, Foreman BD, Srur L, Ganley JP, Redens TB (2013) Bilateral acute pyogenic conjunctivitis with iritis induced by unilateral topical application of bacterial peptidoglycan muramyl dipeptide in adult rabbits. Exp Eye Res 116: 324-336.
- Rose PW, Harnden A, Brueggemann AB, Perera R, Sheikh A, et al. (2005) Chloramphenicol treatment for acute infective conjunctivitis in children in primary care: a randomised double-blind placebo-controlled trial. Lancet 366(9479): 37-43.
- Sheikh A, Hurwitz B (2001) Topical antibiotics for acute bacterial conjunctivitis: a systematic review. Br J Gen Pract 51(467): 473-477.
- McGilligan VE, Gregory Ksander MS, Li D, Moore JE, Hodges RR, et al. (2013) Staphylococcus aureus activates the NLRP3 inflammasome in human and rat conjunctival goblet cells. PLoS One 8(9): e74010.
- McCormick CC, Caballero AR, Balzli CL, Tang A, Weeks A, et al. (2011) Diverse virulence of Staphylococcus aureus strains for the conjunctiva. Curr Eye Res 36(1): 14-20.
- Sheikh A, Hurwitz B (2006) Antibiotics versus placebo for acute bacterial conjunctivitis. Cochrane Database Syst Rev 19(2): CD001211.
- (2020) World Health Organization. 19th Expert Committee on the Selection and Use of Essential Medicines. Essential Medicines Selection. Section 21 Ophthalmological Preparations. Ofloxacin – Addition.
- Hutnik C, Mohammad Shahi MH (2010) Bacterial conjunctivitis. Clin Ophthalmol 4: 1451-1457.
- Dalhoff A (2005) Immunomodulatory activities of fluoroquinolones. Infection 2(S2): 55-70.
- Zhang JZ, Cavet ME, Ward KW (2008) Anti-inflammatory effects of besifloxacin, a novel fluoroquinolone, in primary human corneal epithelial cells. Curr Eye Res 33(11): 923-932.
- Wada T, Kida T, Inoue T, Tokushige H, Naka H, et al. (2008) Immunomodulatory effect of gatifloxacin on mouse peritoneal macrophages in vitro and in models of endotoxin-induced rat conjunctivitis and rabbit bacterial keratitis. Ophthalmic Res 40(2): 54-60.
- Cáceres del Carpio J, Costa RD, Haider A, Narayanan R, Kuppermann BD (2016) Corticosteroids: Triamcinolone, Dexamethasone and Fluocinolone. Dev Ophthalmol 55: 221-231.
- Varu DM, Rhee MK, Akpek EK, Amescua G, Farid M, et al. (2019) Conjunctivitis Preferred Practice Pattern®. Ophthalmology 126(1): 94-169.
- Saika S (2006) TGFbeta pathobiology in the eye. Lab Invest 86(2): 106-115.
- Belfort R Jr, Gabriel L, Martins Bispo PJ, Muccioli C, Zacharias Serapicos PC, et al. (2012) Safety and efficacy of moxifloxacin-dexamethasone eyedrops as treatment for bacterial ocular infection associated with bacterial blepharitis. Adv Ther 29(5): 416-426.
- Espiritu CR, Sy ME, Tayengco TL (2011) Efficacy and tolerability of a combined moxifloxacin/dexamethasone formulation for topical prophylaxis in phacoemulsification: an open-label single-arm clinical trial. J Ophthalmol 2011: 769571.

 Research Article
Research Article