Research Article
Magnitude of poor Sleep Quality and Associated
Factors among Health Sciences Students in Jimma
University, Southwest Ethiopia, 2017
Mebrahtom Zeru1, Hiwot Berhanu1* and Andualem Mossie2
Author Affiliations
1Department of Biomedical Sciences, Institute of Health, Ethiopia
2Department of Biomedical Sciences, College of Medicine and Health Sciences, Ethiopia
Received: January 29, 2020 | Published: February 07, 2020
Corresponding author: Hiwot Berhanu, Department of Biomedical Sciences, Institute of Health, Jimma University, Ethiopia
DOI: 10.26717/BJSTR.2020.25.004202
Background: Sleep disorders have been notified as one of the main health problems
in the society. Most university students suffer from poor sleep quality which is a direct
cause for daytime malfunction. There is a scarcity of data about sleep quality and its
associated factors among university students in Ethiopia. The main aim of this study is
to determine the magnitude of poor sleep quality and its associated factors among health
sciences students in Jimma University, Southwest Ethiopia.
Methods: A cross-sectional study was conducted from May27 to June 27; 2017.Multistage
sampling technique was used to select 422 students. Data were collected using a
semi-structured, pre-tested, self-administered questionnaire. EpiData version 3.1 and
SPSS Version 20 for Windows were used for data entry and data analyses respectively.
Frequencies, means, and proportions were used for descriptive data analysis. Multiple
logistic regression was used to assess the association between poor sleep quality and
independent variables. Statistical significance was taken at P< 0.05.
Results: A total of 404 students completed and returned the questionnaires making
a response rate of 95.74%. More than half of the respondents (54.2%) were classified as
having poor sleep quality. More males (66.7%) were found to have poor sleep quality than
females (33.3%). However, the difference was not statistically significant (p-value=0.62).
Multiple logistic regression analysis revealed that as student’s mean cumulative grade
point average (CGPA) increases by one point, the probability to have poor sleep quality
decreased by about 52% (OR=0.48). Alcohol consumers were 2.5 times more likely to
have poor sleep quality compared to their counterparts [AOR = 2.5, CI (1.37-4.60) p =
0.003]. Similarly, khat chewers were 2.5 times more likely to have poor sleep quality
than non-chewers [AOR = 2.5, CI (1.26-4.93) p =0.008]. Those who use an electronic
device for more than 2 hours a day were 3.9 times more likely to have poor sleep quality
compared to those who use <1 hour a day[AOR = 3.9, CI (1.33-11.64) p = 0.013].
Conclusion: Poor sleep quality was highly prevalent among Jimma University
health science students. Alcohol consumption, khat chewing, academic performance, and
electronic device use were the independent factors associated with poor sleep quality.
Keywords: Poor Sleep Quality; University
Students; Pittsburgh Sleep Quality Index
Sleep is a naturally recurring state characterized by
unconsciousness, relatively suspended sensory activity, and
inactivity of nearly all voluntary muscles [1]. It is very important for
growth and repair, memory consolidation and restorative processes
to occur in the body [2,3]. Getting sufficient sleep is one of the crucial
things that we can do to keep our body healthy [4]. It is required for
optimal wellbeing and function of key cognitive functions related
with academic performance in school [5,6]. However, the standard
of living and environmental factors are causing sleep disturbance
[7]. The National Sleep Foundation’s recommend adolescents to get 8.5– 9.25 hours of sleep and adults to get 7-9 hours of sleep
[5,6]. When students join university, they begin new living styles
and most students modify their sleeping time and sleeping habits
[8,9]. Which could be as a predisposing factor, for the increment of
poor sleep quality among university students [10].
A study conducted to characterize sleep patterns and
predictors of poor sleep quality in a large population of college
student’s shows over 60% were categorized as poor sleepers by
the PSQI measurement [11]. The finding of different studies shows
the prevalence of poor sleep quality among Asian medical student
range from 19- 74.2% [12-16]. Other studies conducted among
Nigerian medical student shows the prevalence of sleep quality
were 70% [17]. The prevalence of poor sleeps quality among
colleges Ethiopian student by Lemma et al has been reported to be
55.8% [18]. Another study conducted in Debre Berhan University
shows the prevalence of insomnia was 61.6% [19]. According to the
findings of different studies female students get poor sleep quality
relative to male students [3,10,12,20,21]. Another study showed
that there was no statistically significant difference in sleep quality
between males and females [22].
A study that evaluated the relationship between poor sleep
quality and consumption of substances such as, alcohol, khat and
cigarette showed a statistically significant association with poor
sleep quality [20]. A study conducted in Jimma Ethiopia shows that
chat chewers are more predisposed for poor sleep quality than
non-chewers [23] Similarly, khat chewer students were classified
as poor sleepers compared to those who did not chew khat. Khat
chewing, especially at a higher quantity, also increased the risk
of poor sleep quality, long sleep latency, poor sleep efficiency and
sleep medicine use [20]. Students who reported the use of caffeinecontaining
drinks per week were 1.48-times more likely to report
long sleep latency compared to nonusers [20]. Smoking was
positively correlated with poor sleep quality, Students who reported
smoking cigarette had long sleep latency, poor sleep efficiency and
sleep medicine use compared to nonsmokers [12,24].
Research conducted on the association of sleep quality and
academic performance so far shows that poor quality sleep is
associated with lower academic performance [25,26]. A study
reported that there was statistically significant association between
the use of electronic devices and poor sleep quality [8]. Prolonged
Users of social networking, such as Face book had poorer sleep
quality than Non-users [22]. Another study also found a positive
relationship between the use of a mobile phone for playing games
and chatting in bed with long sleep latency and severity of sleep
disorders [24]. Limited number of studies was done to determine
sleep quality and associated factors among medical students
in Africa particularly in Ethiopia, there is scarcity of data that
determine the magnitude and predictors of poor sleep quality,
Therefore, we conduct this study so that it could fill the mentioned
gaps by determining the prevalence of poor sleep quality and its
associated factors among medical students.
The study was conducted at Jimma University, which is located
in Jimma town 352 km Southwest of Addis Ababa, using a crosssectional
study designs to determine the magnitude of sleep
quality and associated factors among health science undergraduate
regular students from May 27-June 27, 2017. The sample size
was determined using the single population proportion formula,
taking the following assumptions based on the previous study in
the country that estimated prevalence of poor sleep quality among
university students to be 52.7% [20], with confidence of 95%,
margin of error 5%, and non-response rate of 10% were leading
the final study sample of 422 student subjects. To reach at this
sample the researchers deployed a Multi-stage sampling technique
following which students from all courses of graduation were
included in the study in order to maintain the representativeness
of the sample. Students were stratified by field of study and batch
(year of study).
After allocation of proportionate to size, the study subjects
were selected by simple random sampling. Data were collected
using a semi-structured, pre-tested, self-administered
questionnaire developed by reviewing relevant literature and
standard questionnaire used previously in similar studies (PSQI)
and students’ CGPAs were obtained from students’ self-report
and checked in the office of the registrar. Data were collected by
BSc nursing who have training on data collection and previous
experience of data collection under close supervision of two
experienced supervisors. The questionnaire was initially prepared
in English, translated to local languages Afaan Oromo and Amharic,
and retranslated to English by another person who was blind to
the original questionnaire for consistency check. Pretesting of the
questionnaire was made on 5% of sample size among students of
another university which is Walkite University (which was out of
the main study area having (similar characteristics).
Data were edited, coded, and entered into Epi-Data version3.1
and exported to and analyzed by SPSS version 20. Frequencies,
means, and proportions were used for the descriptive analysis of
data. Tables and charts were used for data presentation. During an
evaluation of association, P-value < 0.05 was considered statistically
significant for final result where 0.25 p-values was indicated to
consider variables at screening stage for multi variable logistic
regression. To make a research ethically safe & acceptable, letter
of permission was obtained from the Ethical clearance Committee
of Jimma University. Similarly, at participant level the objectives
of the study was explained to the participants and followed by
written consent after the student agreed to participate with further
confidentiality of the response by changing them anonymous.
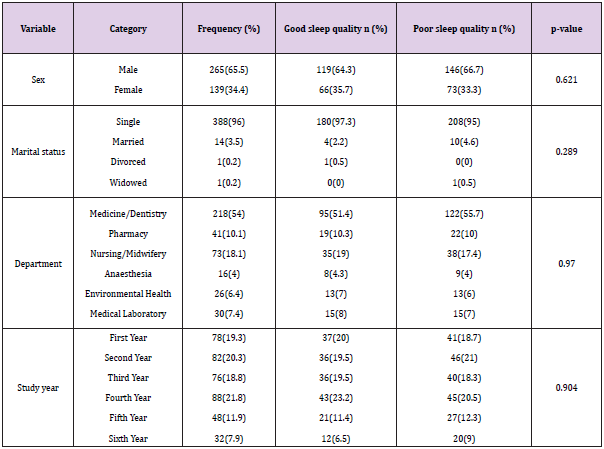
Socio-Demographic Characteristics
Out of 422 study subjects, 404 fully responded to the
questionnaire making a response rate of 95.74%. Majority of the participants were males (65.6%), with a mean age of 22.15 years
(SD± 2.1). More males (66.7%) were found to have poor sleep
quality than females (33.3%). However, the difference was not
statistically significant (p-value=0.62).In relation to their ethnicity,
Oromo 41.6% (n=168) account for highest proportion followed by
Amhara 26.7 % (n=108). Regarding the religion of the participants,
Orthodox Christians account for highest proportion (44.3%)
followed by Protestant (28%), Muslim (18.1%), Catholic (5.7%) and
Traditions (3%). Majority of the participants were single (96%).
Concerning field of study: medicine (53.2%), pharmacy (10.6%),
nursing (18.1%), anesthesia (4.2%), environmental health (6.4%),
and medical laboratory (7.4%).The proportion of poor sleep
quality was highest among medicine students (56%) followed by
pharmacy students (53.7%). In terms of study year, there were a
high proportion of students who were studying in the fourth year
(21.8%) and second year (20.3%). The proportion of participants
categorized to have poor sleep quality was highest among sixthyear
students (65.5%) followed by the fifth year (56%) and secondyear
students (56%). (SD=±0.48) (Table 1).
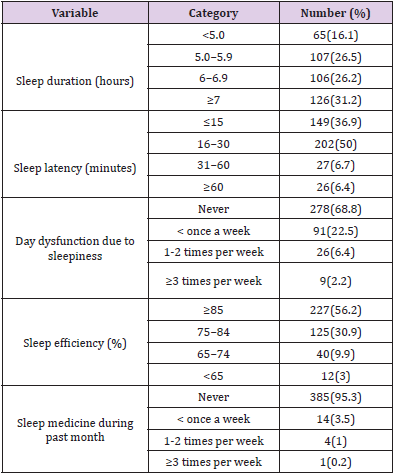
Sleep Quality Parameters
The average bedtime of the students, as reported on the PSQI,
was at 11:40 PM (SD± 1:25 hour) and they wake up at 6:40 AM
(SD±00:55 hour). The mean total time to fall asleep was 24 minutes
(SD±14.78). Participants’ reported time in bed ranged from 3:30
to 13 hours with a mean time in the bed of 7:04 hours (SD±1.50).
Hours of reported actual sleep ranged from 3 to 12 hours with
a mean total sleep time of 6.03 hours (SD±1.46). Majority of the
participants 227(56.2%) had habitual sleep efficiency of >85%
with a calculated mean score of 85.6% (SD±10.82). Nearly all
385(95.3%) of the participants had not taken medications to help
them sleep in the past month. Two hundred seventy-eight (68.8%)
participants had no problems during the day due to their sleepiness
(further measures of sleep quality are reported below as seen in
Table 2. The global PSQI score of the participants ranged from 0 to
15. More than half of the respondents 54.2% (219) were classified
as having poor sleep quality (PSQI >5); at 95%CI with a mean (SD)
global score of 5.52(SD ±2.67).
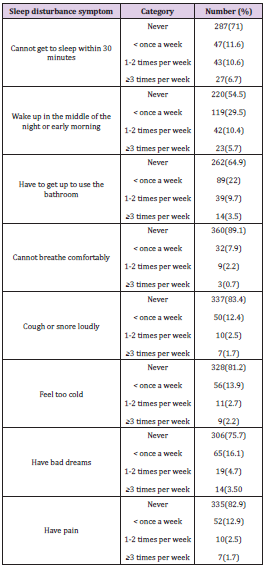
Most of the participants (87%) reported their sleep quality
to be either very good or fairly good. When comparing subjective
measures of self-rated sleep quality (87%) reported either good
or fairly good. Approximately 24.2% of the very good and 63% of
the fairly good self-ratings for overall sleep quality had PSQI scores
greater than five. Nearly all (90%) of those who self-rated their
sleep quality as fairly bad and all of those who self-rated their sleep
quality as very bad were classified as having poor sleep quality
using the PSQI scale (Figure 1). In the area of sleep disturbance,
the study participants reported that, 11.6% (n=47) can’t get asleep within 30 minutes, 29.5%(n=119) wake up in the mid night, 22%
( n=89)get up to use the toilet, 7.9%(n=32 ) can’t take breaths
comfortably, 12.4% (50) cough or sleep with harsh, 13.9%( n=56 )
feel too cold, 16.1% (n=65)experience bad dreams, and 52 (12.9%)
had pain/discomfort during sleep less than once a week (Table 3).
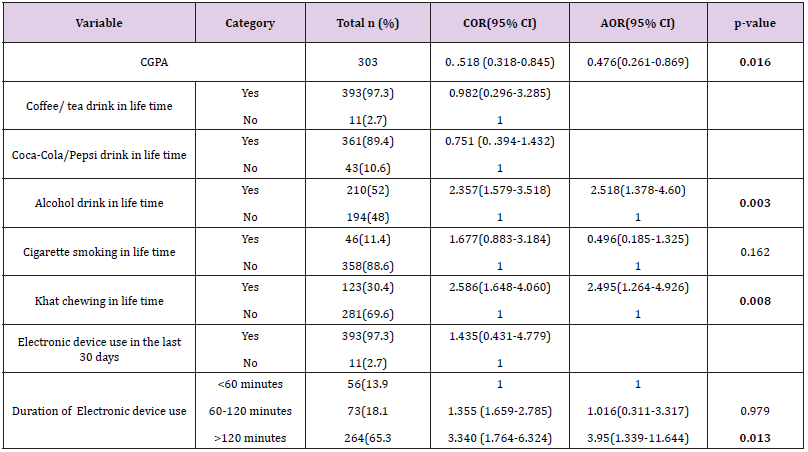
Substance Use and Electronic Device Use
Substance in lifetime were 97.3% coffee/tea, 89.4% Pepsi/
Coca-cola, 52% alcoholic beverages, 11.4% cigarette, and 28.5% khat; and the proportion of participants who reported substance
use in the last month were 95% coffee/tea, 70.5% caffeinated
cola products (Pepsi/Coca-cola), 30.9% alcoholic beverages, 7.7%
cigarette, and 18.6% reported khat. Caffeinated beverages are the
most frequently used substances; 67.3% respondents reported
daily Coffee/ tea and 42.1% reported weekly coca-cola/pepsi drink.
The proportion of participants categorized to have poor sleep
quality was higher among substance users in the last month; coffee/
tea (54.4%), coca-cola/pepsi (56.5%), alcohol (70.4%), cigarette
(80.6%), and khat (76%) users were poor sleepers. Regarding
electronic device, almost all 97.3% respondents reported electronic
device use and 264(65.3%) of the participants use for more than 2
hours with mean (SD) duration of 247 minutes +/- 164.35 per day.
Those who use an electronic device for more than 2 hours (63.2%)
had poorer sleep quality compared to those who use 1- 2 hours
(41%), and those who use less than 1 hour (34%) a day (Table 4).
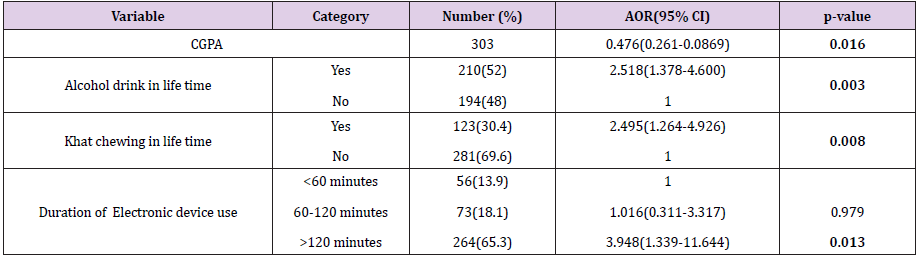
Association Variables
The odds of poor sleep quality according to participants’ sociodemographic
characteristics; substance use and an electronic
device use were examined in the study. From a total of 15 variables
initially considered to be probably associated with sleep quality;
bivariate logistic regression analysis found 7 variables which fulfill
the criteria (p<0.25). Age, monthly income, academic performance,
alcohol consumption, cigarette smoking, khat chewing, and
electronic device use were p-value<0.25 that enter to multiple
logistic regression (Table 5). Multiple logistic regression analysis
revealed that academic performance, Alcohol consumption, khat
chewing, and electronic device use were significantly associated
with sleep quality. Academic performance was negatively associated
with poor sleep quality, as student’s CGPA increases by one point,
the probability to have poor sleep quality decreased by about 52%
(AOR: 0.47 95%CI: 0.26-0.86). Alcohol consumers were 2.5 times
more likely to have poor sleep quality than non-consumers (AOR:
2.5 95%CI: 1.37-4.60). Similarly, khat chewers were 2.5 times more
likely to have poor sleep quality than their counterparts (AOR: 2.5
95%CI: 1.26-4.92). Those who use electronic device >2 hours per
day were 3.948 times more likely to be poor sleepers than those
who use <1 hour per day (AOR: 3.94 95%CI: 1.33-11.64) (Table 6).
In this study, approximately 54.2% of the students were
classified as poor sleepers. Overall, this finding agrees with prior
reports which show over half of the study participants among
university students had poor sleep quality according to PSQI
criteria. For instance, a survey conducted in the Universities of
Ethiopia (Gondar and Haramaya) reported that 52.7% of students
were poor sleepers [22]. Similarly, 51.8% of students in Chile [15]
and 58% of students in Hong Kong [8] had poor sleep quality. The
result of this study is lower than studies conducted in Nigeria where
poor sleep quality were 70% [17] among Pakistan students which
was 64.24% [27] Saudi Arabia. Students 76% [28]. The reported
variations between different studies may be influenced by different
socioeconomic demands, cultural habits and academic pressures
among the different population groups. In this study alcohol is
main the predictor of poor sleep quality among medical students
the study agree by research conducted by Van Reen et al and with
Kenney et al. which alcohol consumption was associated with later
bedtimes and rise times [29,30] this alterations result from acute
alcohol use include shorter sleep onset, a decrease in amount of
rapid eye movement sleep, more stage 4 sleep in the first half of
the night, an increase in wake during sleep, and an increase in delta
electroencephalography power.
Research indicates an association between irregular selfreported
sleep patterns and increased alcohol consumption.
Specifically, self-report of insomnia is associated with a twofold
increase in self-reported alcohol abuse. [31] Whereas this study
disagrees with the study done among large portion of college student
by revealed that tension and stress accounted poor sleep quality,
whereas alcohol and caffeine consumption, were not significant
predictors of sleep quality [32]. Current khat chewers’ participants
had increased risk of poor sleep quality than non-chewers. This
finding agrees with the study conducted in Jimma town and Yemen
[33,34] this could be the result of sympathomimetic effects of khat
(Catha edulis) which has amphetamine like effect Which causes
psycho-stimulation and euphorigenic effects by impairing the sleep
center [34,35]. This study also investigated the use of an electronic
device in relation to the quality of sleep among health science
students. Most of the participants in this study reported the use of
an electronic device.
In this study population, using an electronic device for >2 hours
increased the risk poor sleep quality. Use of electronic devise for
prolonged time showed relation with poor sleep quality, study
conducted among southern Taiwan and Iran students demonstrated
significant negative association between the degree of internet
addiction and sleep quality [36,37] The possible mechanism for the
negative effect of electronics use on sleep is that the light produced
by electronic devices may disturb circadian rhythms by inhibiting
melatonin hormone, resulting in the inability to start sleep at the
right time and the brightness of the light that is projected onto
the retina from computers or mobile screens send signals to
hypothalamus which is thought to be factors that trigger changes
in sleep patterns [38].
Even though we deployed a Multi-stage sampling technique
we didn’t use design effect. Second, use of a self-administered
survey that relied on subjective measures of sleep quality and other
covariates may have introduced some degree of error in reporting
behavioral covariates, and the period of the semester when the
survey was administered could have influenced the sleep quality.
However, we believe that by the use of the anonymous questionnaire
and validated instrument might overcome these issues.
This study provides strong evidence that poor sleep quality is
vastly prevalent among Jimma university health science students.
The findings in this study show that alcohol consumption,
khat chewing, duration of electronic device use and academic
performance are statistically significant predictors of poor sleep
quality which have a big impact on student’s wellbeing. As sleep
good quality may be a marker for health status and quality of life,
prospective studies are needed to be done.
The authors have not declared any conflict of interests.
We would like to express our appreciations to Jimma University
for financial support that helped us to undertake this research. We
also express our heartfelt gratitude to all study participants and
data collectors who were willing to participate in this study.
- Taylor DJ, Bramoweth AD (2010) Patterns and Consequences of Inadequate Sleep in College Students: Substance Use and Motor Vehicle Accidents. Journal of Adolescent Health46(6): 610-612.
- Curcio G, Ferrara M, De Gennaro L (2006) Sleep loss, learning capacity and academic performance. Sleep Medicine Reviews.
- Araújo MFM de, Lima ACS, Araújo TM de, Veras VS, Zanetti ML, et al. (2014) Association of sociodemografic factors and sleep quality in brazilian university students.Texto e Contexto Enfermagem, 23(1): 176-184.
- Boysan M (2016) Developmental Implications of Sleep. A J Clin Neurosci Psychopathol18(2):44-52.
- (2007) Prince R, Hospital A. Global perspectives on sleep and health issues. pp. 35-42.
- Afandi O (2013) Sleep Quality Among University Students: Evaluating the Impact of Smoking , Social Media Use , and Energy Drink Consumption on Sleep Quality and Anxiety. Student Pulse 5(06): 1-3.
- Kazim M, Abrar A (2011) Sleep patterns and academic performance in pa students of amedical college in p. KUST Med J3(2):60.
- Azad MC, Fraser K, Rumana N, Abdullah AF, Shahana N, et al. (2015) Sleep disturbances among medical students: a global perspective. J Clin Sleep Med11(1):69-74.
- Afandi O, Hawi H, Mohammed L, Salim F, Hameed AK, Rizwana B (2012) Sleep quality among University students in the UAE. GULF Med J1:193-199.
- (2004) Regional WHO. WHO technical meeting on sleep and health European Centre for Environment and Health: 22-24.
- Suen LK, Tam WW, Hon K (2010) Association of sleep hygiene-related factors and sleep quality among university students in Hong Kong. Hong Kong Med J16(3):180-185.
- Lund HG, Reider BD, Whiting AB, Prichard JR, et al. (2010) Sleep Patterns and Predictors of Disturbed Sleep in a Large Population of College Students. J Adolesc Heal[Internet]46(2):124-132.
- Lu J, Fang GE, Shen SJ, Wang Y, Sun Q (2011) A Questionnaire survey on sleeping in class phenomenon among Chinese medical undergraduates. Med Teach 33(6):508.
- Huen LL, Chan TW, Yu WM, Wing YK (2007) Do medical students in Hong Kong have enough sleep? Sleep Biol Rhythms 5(3):226-230.
- Zailinawati AH, Teng CL, Chung YC, Teow TL, Lee PN, et al. (2009) Daytime sleepiness and sleep quality among Malaysian medical students. Med J Malaysia 64(2):108-110.
- Ghoreishi A(2008) Sleep quality in Zanjan university medical students. Tehran Univ Med J66(1):66-71.
- Aesha Farheen Siddiqui, Hasan Al Musa, Hasan Al Amri, Abdulkareem Al Qahtani, Mushabab Al Shahrani, et al. (2016) Sleep Patterns and Predictors of Poor Sleep Quality among Medical Students in King Khalid University, Saudi ArabiaMalays J Med Sci 23(6): 94-102.
- Ibrahim NK, Badawi FA, Mansouri YM, Ainousa AM, (2017) Sleep Quality among Medical Students at King Abdulaziz University: A Cross-sectional Study. J Community Med Health Educ 7: 561.
- Seblewngel Lemma, Bizu Gelaye, Yemane Berhane, Alemayehu Worku, Michelle A Williams (2012) Sleep quality and its psychological correlates among university students in Ethiopia: a cross-sectional study Lemma et al. BMC Psychiatry 12:237.
- Haile YG, Alemu SM, Habtewold TD (2017) Insomnia and Its Temporal Association with Academic Performance among University Students : A Cross-Sectional Study 4: 1-7.
- Lemma S, Sheila V, Yared A, Mahlet G, Yemane B, et al. (2012) The epidemiology of sleep quality, sleep patterns, consumption of caffeinated beverages, and khat use among Ethiopian college students. Sleep Disorders: 593510.
- Doi Y, Minowa M (2003) Gender differences in excessive daytime sleepiness among Japanese workers. SocSci Med56(4):883-894.
- Afandi O, Hawi H, Mohammed L, Salim F, Hameed AK, Rizwana B (2012) Sleep quality among University students in the UAE. Gulf Med J1:193-199.
- Tadeg J, Andualem M, Hiwot B Yigizie Y (2019) Poor sleep quality and its predictors among type 2 diabetes mellitus patients attending Jimma University Medical Center, Jimma, Ethiopia. BMC Res Notes 12:488.
- Fossum IN, Nordnes LT, Straume S, Bjorvatn B, Pallesen S (2015) The Association Between Use of Electronic Media in Bed Before Going to Sleep and Insomnia Symptoms, Daytime Sleepiness, Morningness, and Chronotype. Behav Sleep Med 12(5):343-357.
- Gilbert SP, Weaver CC (2010) Sleep quality and academic performance in university students: a wake-up call for college psychologists. J Coll Student Psychother: 295-306.
- Perkinson Gloor N, Lemola S, Grob A (2013) Sleep duration positive attitude toward life, and academic achievement: The role of daytime tiredness, behavioral persistence , and school start times. J Adolesc 36(2): 1-8.
- Maheshwari G, Shaukat F (2019) Impact of Poor Sleep Quality on the Academic Performance of Medical Students. Cureus 11(4): e4357.
- Almojali, Almalki SA, Alothman AS, Masuadi EM, Alaqeel MK (2017)The prevalence and association of stress with sleep quality amongmedical student. Journal of Epidemiology and Global Health 7(3): 169-174.
- Van Reen E, Roane BM, Barker DH, McGeary JE, Borsari B, et al. (2016) Current alcohol use is associated with sleep patterns in first-year college students. SLEEP 39(6):1321-1326.
- Brower KJ (2003) Insomnia, alcoholism and relapse. Sleep Med Rev 7(6): 523-539.
- Hannah G Brian D (2010) Sleep Patterns and Predictors of Disturbed Sleep in a Large Population of College Students. Journal of Adolescent Health 46(2): 124-132
- Berhanu H, Mossie A, Tadesse S, Geleta D (2018) Prevalence and associated fac-tors of sleep quality among adults in Jimma Town, Southwest Ethiopia: a community-based cross-sectional study. Sleep Disord4:342328.
- AD Ali (2015) A pilot community-based study on association ofKhat (Catha edulis) chewing practice with psychosis inYemen. American Journal of Health Research3(2): 91-96.
- Abebe M, Adane K (2015) Adverse health efects of khat: a review. Family Med Sci Res4(1):154.
- Lin PH, Lee YC, Chen KL, Hsieh PL, Yang SY, et al. (2019) The Relationship Between Sleep Quality and Internet Addiction Among Female College Students. Front Neurosci 13:599.
- Purreza A, Mostafa E, Saeed R, Moslem J, (2016) Studying the Relationship between Quality of Sleep and Addiction to Internet among Students. Nova Journal of Medical and Biological Sciences 5(3): 1-7.
- Cheung LM, Wong WS (2011) The effects of insomnia and internet addiction on depression in Hong Kong Chinese adolescents: an exploratory cross-sectional analysis. Journal of Sleep Research 20(2): 311-317.

 Research Article
Research Article