Abstract
Synopsis
Bladder training and biofeedback are equivalent for patients with stress urinary incontinence, considering general quality-of-life, sexual function, symptoms, and measures of muscle strength.
Keywords: Female Urinary Incontinence; Stress Urinary Incontinence; Pelvic Floor Muscle Training; Biofeedback; Quality of Life; Sexual Function
Abbreviations: UI: Urinary Incontinence; PFMT: Pelvic Floor Muscle Training; SUI: Stress Urinary Incontinence; MUI: Mixed Urinary Incontinence; BD: Bladder Diary; BIO: Biofeedback; HCPA: Hospital De Clinicals De Porto Alegre; BT: Bladder Training
Short Communication
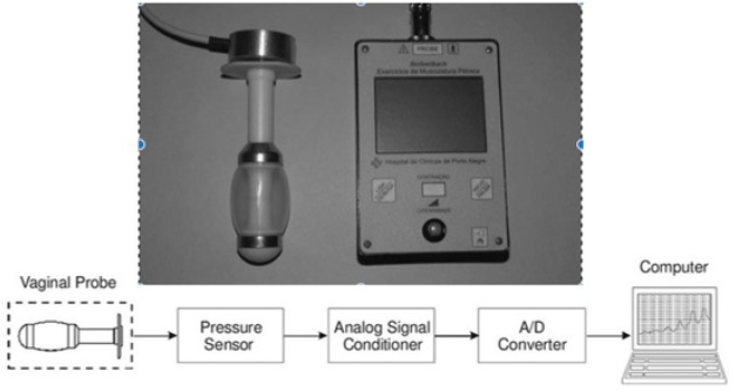
Urinary incontinence (UI) is defined as involuntary leakage of urine, with a wide spectrum of severity and a prevalence reaching 30% [1,2]. Initial management can be conservative with pelvic floor muscle training (PFMT). Supplementary physiotherapy techniques such as biofeedback can benefit patients who have difficulty with pelvic floor awareness, low motivation, or low adherence. Sanchez et al. [3] have described a home-use perineometer device (pressure biofeedback) intended to achieve better results for patients with stress or mixed urinary incontinence (SUI or MUI). Biofeedback group exhibited better performance than PMFT-only group (81/51% - P=0.025) [4]. The present study was designed to expand investigation of this biofeedback (BIO) technique. The design is a controlled, non-blinded, parallel, randomized clinical trial, conducted at a Urogynecology Clinic from January 2013 to September 2016. Sampling was consecutive and the women recruited were over the age of 18 and had SUI or MUI with a predominance of stress symptoms. Manual pelvic floor assessment and pressure perineometer was performed.
Bladder diary (BD), questionnaires on urogenital symptoms, quality of life and sexual function were administered. Patients in Group 1 (bladder training - BT) were given a form containing instructions on behavioral measures and lifestyle changes. The patients in Group 2 (Biofeedback - BIO) followed the same initial routine, with the addition of training on how to use the device. The final assessment was conducted after 12 weeks for both groups. Patients in Group 2 (BIO) performed a standardized series of mixed exercises for rapid and slow response fibers. Fourteen patients in each group were analyzed at the end of the study. Both groups exhibited improved results for number of daily leakages (P<0.001; β=21,4%) and nighttime micturition’s (P<0.002; β=14,5%). For sexual function, there were no individual or intragroup differences. As for quality of life measures, the improvements in sleep and in energy observed may be associated with the reduction in number of nighttime micturition’s observed in the BD analysis (P=0.002). Impact of incontinence exhibited a tendency towards significance in the BIO Group (P=0.053) in relation to the BT Group (P=0.006) (β=37,1%). Improvements in perineal contraction were not correlated with increased muscle strength (Rs=0.428 P=0.144). No adverse effects were observed during the study. Development of supplementary technologies is an unexplored area, with many improvements yet to be implemented. This study was approved by the local Research Ethics Committee (certificate no. 03356212.2.0000.5329), and informed consent was obtained from all the participants (Figure 1).
Acknowledgment
We acknowledge the financial support of FAPERGS, FIPE/ HCPA, CNPq. Financial disclosure: The authors have no financial relationships relevant to this article to disclose. Adriana Schmidt: design, planning, execution, data analysis, preparation of manuscript; Tatiane Araújo: execution, analysis, preparation of manuscript; Paulo Sanches and Danton Júnior: servicing and preparation of devices, importing data, software programming, data analysis, José Geraldo Ramos: design, planning, data analysis; methodological review; preparation of manuscript.
Financial Disclosure
The authors have no financial relationships relevant to this article to disclose.
Conflict of Interest
The authors have no conflicts of interest to disclose.
References
- Kammerer Doak D, Rizk DE, Sorinola O, Agur W, Ismail S, et al. (2014) Mixed urinary incontinence: international urogynecology association research and development committee opinion. Int Urogynecology J 25(10): 1303-1312.
- Dumoulin C, Hay Smith J (2014) Pelvic floor muscle training versus no treatment, or inactive control treatments, for urinary incontinence in women. Cochrane Database Syst Rev 5: CD005654.
- Sanches PR, Silva DP, Muller AF, Schmidt AP, Ramos JG, et al. (2009) Vaginal probe transducer: Characterization and measurement of pelvic floor strength. J Biomech 42(15): 2466-2471.
- Schmidt AP, Sanches PR, Silva DP, Ramos JG, Nohama , et al. (2009) A new pelvic muscle trainer for the treatment of urinary incontinence. Int J Gynaecol Obstet 105(3): 218-222.

 Short Communication
Short Communication