Abstract
Vitamin D levels are significantly lower in obese children and adolescents compared to non-obese matching peers. While evaluating the number of obese and non-obese cases who improved upon vitamin D supplement, obesity was found to pose a risk for not receiving benefit from the vitamin D supplementation. Vitamin D given to these vulnerable groups results in a significantly attenuated increase in 25(OH)D levels with supplementation. However, the proper dose and duration cannot be deduced because several of the studies reported a portion of vitamin D deficient obese children and adolescents at the end of their supplementation period. Screening for vitamin D levels is thus recommended since obese children and adolescents are more prone to be deficient. Additionally, the dose and duration of vitamin D supplementation or treatment should follow the guidelines. Finally, it is prudent to hypothesize that if the published studies had performed simultaneous weight adjustment strategies more of the enrolled obese participants would have reached vitamin D sufficiency by the end of the supplementation trial coupled with the favorable changes in their BMI.
Keywords: Adolescents; Supplementation; Vitamin D; Obesity; Dose
Mini Review
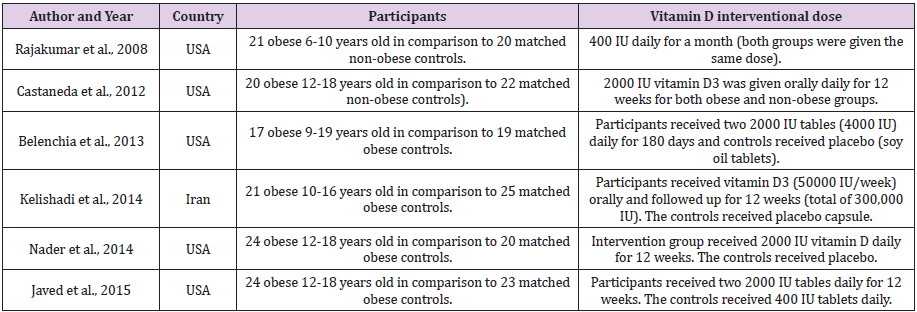
Many previous worldwide studies pointed out the decreased 25-hydroxy vitamin D [25(OH)D] levels that occur in obese adolescents compared to normal weight controls [1-3]. Lower concentrations of serum 25(OH)D levels in obese subjects may be explained by enhanced uptake by adipose tissue and increased metabolic clearance, and it is suggested that the sedentary lifestyle of obese subjects could be associated with less outdoor activity and less exposure to sunlight [4,5]. There was no consensus regarding the dosage given in the earlier interventional studies which supplemented deficient adolescents with vitamin D. From the literature, six randomized controlled trials (RCT) [6-11] which supplied obese children and adolescents with vitamin D were identified and are demonstrated in Tables 1 & 2. Two of these studies gave vitamin D supplementation dose according to the guidelines which is 1200-2000 IU daily for obese pediatric age patients [12]. One gave a daily dose of 400 IU which is even less than the updated RDA of vitamin D in this age group (600 IU) according to the global consensus recommendations by [13]. The last three gave higher doses of vitamin D; two of them provided 28000 IU weekly either for 180 days or 12 weeks, and in the third 50000 IU was given weekly for 12 weeks. Although all six studies were managing obese children and adolescents with deficient vitamin D status, only the latter three studies provided a treatment dose which is between 3000-6000 IU daily according to the global consensus recommendations by [13].
Table 2: Randomized controlled clinical trials which supplied obese children and adolescents with vitamin D.
The study of Belenchia, et al. [8], which performed the longest supplementation period among the previous six studies, reported that only 93% of those receiving vitamin D supplementation became sufficient after 6 months. A more alarming number was reported by Javed et al. [11] who found that 75% of their vitamin D supplemented children and adolescents did not reach vitamin D sufficiency by the end of the 12-week supplementation trial. Additionally, Harel, et al. [14] reported that although there was a significant increase in mean 25(OH)D after the initial course of treatment with vitamin D, 25(OH)D levels normalized in only 28% of their series of obese adolescents in a non-RCT supplementation study carried out in the USA. The latter authors further added that repeat courses with the same dosage in the other 72% did not significantly change their low vitamin D status given that the dose used was 50000 IU weekly for 6-8 weeks for deficient adolescents.
Earlier in 2013, Vimaleswaran, et al. [15] concluded via a bidirectional genetic approach that a higher BMI leads to lower 25(OH)D, while any effects of lower 25(OH)D increasing BMI are likely to be small. The latter authors predicted that population level interventions to reduce BMI are expected to decrease the prevalence of vitamin D deficiency. Nevertheless, almost all published clinical trials for vitamin D supplementation in obese children and adolescents didn`t plan a simultaneous weight control program to ensure better response to the assigned dosage.In conclusion, obese children and adolescents should be screened for vitamin D levels since they are more prone to be deficient. Additionally, vitamin D supplementation and treatment for obese children and adolescents should follow the guidelines regarding the dose given with close follow up for compliance and effects. Finally, it is prudent to hypothesize that if the interventional studies for vitamin D supplementation had performed simultaneous weight adjustment strategies whether by diet and/or exercise, more of their enrolled children and adolescents would have reached vitamin D sufficiency. Future supplementation studies should thus be designed to include weight management program for such vulnerable ages to help achieve better vitamin D levels coupled by the expected BMI favourable changes.
Funding
None.
Acknowledgement
None.
Conflict of Interest
No conflict of interest.
References
- Alyahya KO (2017) Vitamin D levels in schoolchildren: a cross-sectional study in Kuwait. BMC Pediatr 17(1): 213.
- Kumaratne M, Early G, Cisneros J (2017) Vitamin D Deficiency and association with body mass index and lipid levels in Hispanic American adolescents. Glob Pediatr Health 4: 2333794X17744141.
- Kitsos A, Dounousi E, Kalaitzidis R, Anna Challa, Kostas C Siamopoulos, et al. (2018) Serum vitamin D in obese and overweight subjects according to estimated glomerular filtration rate. Hormones (Athens) 17(2): 237-246.
- Wortsman J, Matsuoka LY, Chen TC, Lu Z, Holick MF (2000) Decreased bioavailability of vitamin D in obesity. Am J Clin Nutr 72: 690-693.
- Bolland MJ, Grey AB, Ames RW, Mason BH, Horne AM, et al. (2007) The effects of seasonal variation of 25-hydroxyvitamin D and fat mass on a diagnosis of vitamin D sufficiency. Am J Clin Nutr 86: 959-964.
- Rajakumar K, Fernstrom JD, Holick MF, Janine E Janosky, Susan L Greenspan (2008) Vitamin D status and response to vitamin D 3 in obese vs non-obese African American children. Obesity 16: 90-95.
- Castaneda RA, Nader N, Weaver A, Ravinder Singh, Seema Kumar (2012) Response to vitamin D3 supplementation in obese and non-obese Caucasian adolescents. Horm Res Paediatr 78(4): 226-231.
- Belenchia AM, Tosh AK, Hillman LS, Peterson CA (2013) Correcting vitamin D insufficiency improves insulin sensitivity in obese adolescents: a randomized controlled trial. Am J Clin Nutr 97: 774-781.
- Kelishadia R, Saleka S, Saleka M, Mahin Hashemipour, Mahsa Movahedian (2014) Effects of vitamin D supplementation on insulin resistance and cardiometabolic risk factors in children with metabolic syndrome: a triple-masked controlled trial. J Pediatr (Rio J) 90(1): 28-34.
- Nader NS, Castaneda RA, Wallace J, Deepak Khandelwal, Avneet Kaur Oberoi, et al. (2014) Effect of vitamin D 3 supplementation on Serum 25(OH)D, lipids and markers of insulin resistance in obese adolescents: A prospective, randomized, placebo-controlled pilot trial. Horm Res Paediatr 82: 107-112.
- Javed A, Vella A, Balagopal PB, Philip R Fischer, Amy L Weaver, et al. (2015) Cholecalciferol supplementation does not influence b-cell function and insulin action in obese adolescents: A Prospective double-blind randomized trial. J Nutr 145: 284-290.
- Cediel G, Pacheco Acosta J, Casti UoDurdn C (2018) Vitamin D deficiency in pediatric clinical practice. Arch Argent Pediatr 116(1): e75-e81.
- Munns CF, Shaw N, Kiely M, Thacher TD, Ozono K, et al. (2016) Global Consensus Recommendations on Prevention and Management of Nutritional Rickets. J Clin Endocrinol Metab 101(2): 394-415.
- Harel Z, Flanagan P, Forcier M, Harel D (2011) Low vitamin D status among obese adolescents: prevalence and response to treatment. J Adolesc Health 48(5): 448-452.
- Vimaleswaran KS, Berry DJ, Lu C, Tikkanen E, Pilz S, et al. (2013) Causal relationship between obesity and vitamin D status: bi-directional Mendelian randomization analysis of multiple cohorts. PLoS Med 10(2): e1001383.

 Mini Review
Mini Review