Abstract
Objective: To compare the severe complications of open surgical repair with successful endovascular grafting using the alternative resuscitative technique. This experience could give spine surgeons more information about these life-threatening complications and provide another method to deal with this acute situation in the future.
Summary of Background Data: Acute vascular injury in a lumbar disc operation is a rare and life-threatening complication. Early recognition, resuscitation, and treatment play an important role in the management of complicated vessel injury. This surgical intervention used both open approach and endovascular surgery. Over the past decade, there has been a trend toward endovascular surgery. However, a patient could only receive an angiography under effective resuscitative control.
Method: We retrospectively reviewed medical charts from January 1, 2006 to December 31, 2016 for spinal fusion surgery at our institute. In a ten-year review, only two cases, with an incidence of 0.03%, of complicated vessel injury were recorded from 6,640 spinal fusion surgeries.
Results: Major vessel injuries were located in L4-L5 and L5-S1 spaces. The first case was microdisectomy and the other case was interbody fusion. Both cases had intraoperative hypotension and abdominal distention. Estimated blood loss were 15400ml and 2500ml, respectively. All type of injury was laceration. Comparing to the first case, the second case demonstrated less blood transfusion and no devastating conditions.
Conclusion: Spinal surgeons should keep this technique in mind for hemorrhage control and realize the subsequent complications.
Keywords: Vessel Injury; Aortic Cross Clumping; Endovascular Grafting; Spine Surgery
Abbreviations: TLIF: Transforaminal Lumbar Interbody Fusion; CT: Computed Tomography; ECMO: Extracorporeal Membrane Oxygenation; MRI: Magnetic Resonance Imaging
Introduction
Acute great vessel injury can be a fatal complication during disc operations. This type of injury has different clinical presentations, such as vascular laceration, arteriovenous fistula, or pseudo aneurysm [1,2]. The incidence of vessel injury during lumbar disc surgery is rare, and most of these injuries are not obvious during the operation. Early recognition, resuscitation, and treatment play an important role in the management of complicated vessel injury. This situation could prove fatal if effective first aid is not executed immediately. However, a few high evidence articles concluded the management of vascular injury complications in lumbar disc surgery. In the past decade, open surgical repair remained the mainstay of surgical intervention for vascular injury. The type of injury impacts the choice of surgical intervention. The open approach for hemorrhage control was traditionally indicated for laceration in an acute setting [3], whereas the endovascular repair was indicated for an arteriovenous fistula or pseudo aneurysm. This technique has advanced for different types of injury, including laceration, over the past decade [4]. The previous study demonstrated that endovascular repair could reduce the morbidity and mortality rates in patients with unstable hemodynamic status [5]. Moreover, the angiography could confirm the lesion and provide the most minimally invasive form of treatment. However, the patient could receive angiography under effective resuscitative control. Few articles address the issues of the resuscitative strategy for acute hemorrhagic control.
A previous systemic review, published in 2002, demonstrated vascular injury during a lumbar surgery. The results showed that most of the cases were treated as conventional repairs. Recently, the endovascular technique has been hailed as an alternative treatment, because of its lowered risk of comorbidity and complications of open suture repair. Another recent review demonstrated the trend toward the importance of endovascular repair. The advantage of angiography could confirm the diagnosis and control the hemorrhage using endovascular grafting, while lowering related complications with open surgical repair [6]. Aortic cross clumping was traditionally used for hemorrhage control in trauma or cardiovascular surgery; however, few articles discuss how this technology was utilized as hemorrhage control in lumbar disc surgery. The objective of this report is to compare the severe complications of open surgical repair with successful endovascular grafting using the alternative resuscitative technique. This experience could give spine surgeons more information about these life-threatening complications and provide another method to deal with this acute situation in the future.
Methods
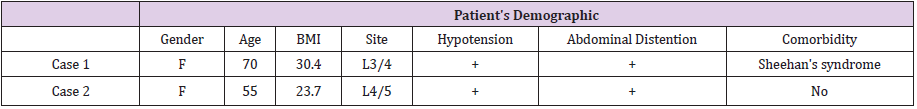
We retrospectively reviewed medical charts from January 1, 2006 to December 31, 2016 for lumbar spinal fusion surgery at our institute. In a ten-year review, only two cases of complicated vessel injury were recorded from 6,640 spinal fusion surgeries. The incidence of acute vessel injury in spinal fusion surgery at our institute was 0.03%. The patients’ demographics, surgical data, and case management were recorded. We analyzed the data about preoperative blood loss, total blood transfusion, symptoms, injured vessels, preoperative cardiac arrest, and abdominal compartment syndrome. The patient demographics and surgical data are illustrated in Tables 1 & 2.
Methods
Case 1
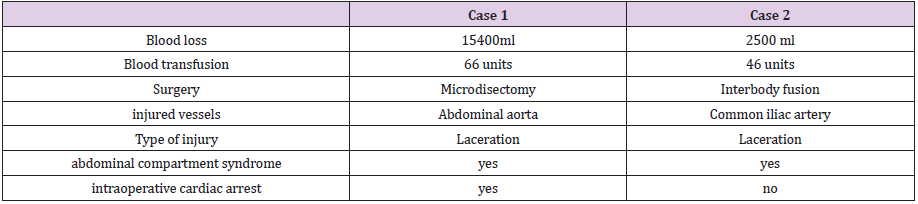
A 70-year-old woman with Sheehan’s syndrome was admitted for micro decompression and L3-L4 discectomy from the left side on February 1, 2012. The computed tomography (CT) of the lumbar spine demonstrated degenerative retrolisthesis, grade I, and disc bulging in the L3-L4 space (Figure 1). The operation time was about five hours, and the perioperative period was smooth. Consciousness change and the acute onset of hypotension happened in the postoperative room. Additionally, abdominal distention was found. Acute internal bleeding and abdominal compartment syndrome were highly suspected; therefore, an emergent midline laparotomy was performed, and the lesser sac was opened and entered. The abdomen aorta was cross clamped at the level of celiac axis. Perforation of abdominal aorta, about 50% of circumference with 0.5 cm defect over the posterior aspect, at the level just above common iliac bifurcation, was found. The massive retroperitoneum hematoma was about 15,400 ml. Cardiac arrest ensued and cardiopulmonary resuscitation was performed immediately. Extracorporeal Membrane Oxygenation (ECMO) was indwelled. The laceration was repaired with 4-0 prolene plus pledget suture, continuously. However, cardiac arrest still persisted, and the patient expired on the table.
Case 2
A previously healthy 55-year-old woman was admitted with symptoms and signs of low back pain radiating to the right leg for six months. These symptoms were accompanied with numbness below the knee and weakness of the right ankle. The plain film disclosed degenerative joint disease of the lumbar spine with marginal spurs formation and intervertebral disc space narrowing over the L4-L5 level. Magnetic resonance imaging (MRI) reportedly showed marked disc space narrowing and the herniation of the L4-5 nucleus pulpous and hypertrophy of facet joints to encroach the dural sac and bilateral intervertebral foramen (Figure 1). She was submitted for transforaminal lumbar interbody fusion (TLIF), L4-L5, on October 7, 2016. The patient was operated on under general anesthesia. Perioperative blood pressure was measured over 48/18 mmHg during discectomy under Loupes. No tachycardia was measured. Unstable hemodynamic status after resuscitation persisted during discectomy over the L4-L5 level through posterior approach.
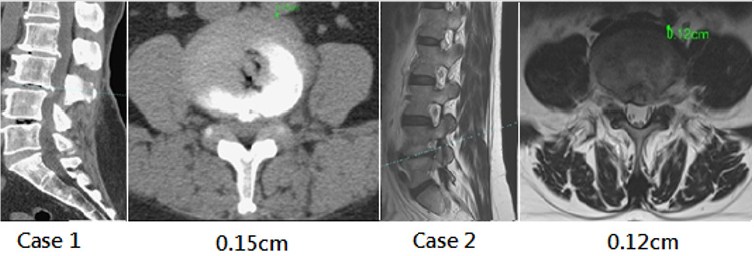
An operation was held, and the wound was closed with gauze packing. Then, the patient was turned to the supine position and the vascular surgeon was consulted. Emergent aortic cross clumping at the descending aorta via thoracotomy was performed, and the patient was sent to the angiographic room. Left common iliac artery active bleeding with massive retroperitoneal hematoma was found during the angiogram (Figure 2). A 0.035 Terumo wire was inserted into the left femoral artery under flouro. A pigtail was inserted, and the Terumo wire was changed to Amplus wire. A 7-mm x 5-cm Viabahn endoprosthesis was deployed smoothly (Figure 2). Then, the aortic cross clamping was taken off. The ischemia time was 50 minutes. After contrast injection, no further leak was noted. Abdominal compartment syndrome was suspected, and the peritoneum was opened, and decompression was completed. A massive retroperitoneal hematoma of about 500 ml was noted. A chest tube was inserted via thoracotomy.
Figure 2: The angiography demonstrated left common iliac artery perforation and acute bleeding control after stent replacement.
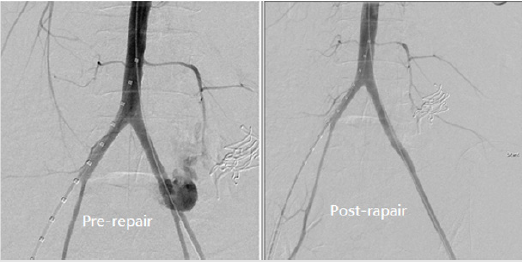
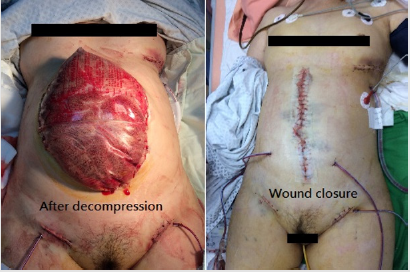
One pad was used to cover the intestines temporarily. Abdominal wound closure was done three days later, after emergent surgery (Figure 3). Postoperative lab data demonstrated normal renal function and coagulation file. Mild elevated liver function was found on postoperative day two and returned to the normal range on postoperative day five. Removal of the endotracheal tube was performed on postoperative day six. No paraplegia or pulmonary complications were found during the postoperative period. The patient was discharged 24 days after operation. Major vessel injuries were located in L4-L5 and L5-S1 spaces. The first case was microdiscectomy and the other case was interbody fusion. Both cases had intraoperative hypotension and abdominal distention. Estimated blood loss were 15400ml and 2500ml, respectively. All type of injury was laceration. Comparing to the first case, the second case demonstrated less blood transfusion and no devastating conditions (Table 2).
Figure 3: The angiography demonstrated left common iliac artery perforation and acute bleeding control after stent replacement.
Intervertebral discectomy and fusion during TLIF are performed posteriorly to the anterior annular complex. In regard to the intact anterior longitudinal ligament, vessel injury complications during discectomy are rare. Several previous studies demonstrated the incidence of vessel injury during lumbar discectomy was around 0.039-0.14% [6-9]. The previous study demonstrated a mortality rate of about 15% [3]. Some literature disclosed different presentation of postoperative vascular injury, such as Arteriovenous fistula or pseudo aneurysm [1,2]. The injuries during lumbar disc surgery can be acute onset or late presentation [3]. Intraoperative vascular injury can be a life-threatening complication [4]. The diagnosis of vascular complication depends on the CT scan or angiography [1,5,10]. However, the diagnosis during the intraoperative period depends on clinical suspicion, such as unstable hemodynamic status after intensive resuscitation. The surgical repair technique varies with different types and sites of injury [6]. Surgical exploration still remains the definitive treatment during the preoperative period.
However, it is sometimes difficult to detect the bleeding site during surgical exploration, which can cause s devastating condition. From our first case, a massive hematoma accumulated in the retro peritoneum, and sudden collapse occurred while the tamponade was released. It was hard to find the active bleeding site and repair the vascular lesion. The development of endovascular surgery in treating acute vessel injury was discussed in numerous pieces of literature [11-13], and several successful case reports were published in recent years [14-16]. The key to the success of emergent endovascular surgery was how to stabilize hemodynamic status before transfer to the angiographic room. In regard to our second case, emergent aortic cross clumping at the descending aorta via thoracotomy seemed to be an alternative technique for treating an unstable hemodynamic status during the preoperative period. Aortic cross clumping could be used to address uncontrolled non-compressible torso hemorrhage in trauma control. In early resuscitation, aortic cross clumping plays an important role in damage control. Aortic cross clumping could increase the clumpinduced afterload, which could raise mean arterial pressure. It could also shift volume to increase myocardial demand.
However, it may cause several complications, such as pulmonary complications, visceral ischemia, spinal cord ischemia, and systemic coagulopathy [17]. Postoperative organ failure may cause temporary or irreversible adverse events. Few articles applied this traditional technique for damage control of acute vessel injury in lumbar discectomy during the intraoperative period. Early diagnosis and rapid control of the hemorrhage should be part of treatment paradigm. This requires packing off the posterior wound and getting rapid access to the retroperitoneal vessels. However, it could also impair the retroperitoneal tamponade and accelerate blood loss, causing the patient to enter a very unstable hemodynamic status. In our case, we successfully combined aortic cross clumping and endovascular surgery for acute resuscitation and treatment. After treatment, even though we opened the retro peritoneum, there was no trepidation about loss of retroperitoneal tamponade. The patient did not have subsequent sequelae after the operation. A higher incidence of major vessel injury was located in L4-L5 and L5-S1 during disc operation [3,18]. At the L4-L5 space, common iliac arteries were within 5 mm of the anterior aspect of disc space. There were little changes in measurement between the supine and prone positions. Therefore, the distance at L4-L5 space between great vessels and the anterior edge of the disc space was closer than the other disc space [19].
In our two cases, great vessels were much closer to the anterior aspect of disc space. The two cases were 0.15 cm and 0.12 cm. On the other hand, another author explained why not all breaches of discs result in vessel injury. Preidiscal fibrosis may be one of the predictors [20]. However, further study will be needed to identify the predictors to determine who will be susceptible to intraoperative vessel injury during disc operation. Several pieces of literature discussed great vessel injury following lumbar micro discectomy [21]. Few articles investigated the association between minimally invasive surgery and complicated vessel injury. On the other hand, the previous review article mentioned that the microscopic technique in lumbar spine surgery seemed to be promising in avoiding vessel injury during lumbar spine surgery [3]. From a 10-year retrospective review at our institute, all acute and life-threatening cases were under microscope or Loupes. This may be related to the fact that the surgeons were not familiar with the depth of field under microscope or Loupes during the learning curve, which is not associated with minimally invasive surgery.
Conclusion
From now on, there is no consensus for management of emergent resuscitation and management during disc operation. Endovascular intervention is one of the first alternative techniques in decades, but only patients with relatively stable hemodynamic status were candidates for transfer to the angiographic room. Traditional aortic cross clumping could be used as the rescue technique; however, it may result in several temporary or irreversible complications. Therefore, spinal surgeons should keep this technique in mind for hemorrhage control and realize the subsequent complications.
References
- Shreiber MH, Wolma FJ, Morretin LB (1967) Angiographic findings in arteriovenous fistulas following lumbar disc surgery. Amer J Roentgenol 101(4): 957-960.
- Davies JM (1969) Ilio-iliac arteriovenous fistula following laminectomy. Clin Radiol 20(1): 103-104.
- Franzini M, Altana P, AnnessiV, Lodini V (1987) Iatrogenic vascular injuries following lumbar disc surgery. Case report and review of the literature. J Cardiovascular Surg (Torino) 28(6): 727-730.
- Kwon TW, Sung KB, Cho YP, Kim DK, Ko GY, et al. (2003) Large vessel injury following operation for a herniated lumbar disc. Ann Vasc Surg 17(4): 438-444.
- Nam TK, Park SW, Shim HJ, Hwang SN (2009) Endovascular treatment for common iliac artery injury complicating lumbar disc surgery: limited usefulness of temporary balloon occlusion. J Korean Neurosurg Soc 46(3): 261-264.
- Papadoulas S, Konstantinou D, Kourea HP, Kritikos N, Haftouras N, et al. (2002) Vascular Injury Complicating Lumbar Disc Surgery. A Systematic Review. Eur J Vasc Endovasc Surg 24(3): 189-195.
- van Zitteren M, Fan B, Lohle PN, de Nie JC, de Waal Malefijt J, et al. (2013) A shift toward endovascular repair for vascular complications in lumbar disc surgery during the last decade. Ann Vasc Surg 27(6): 810-819.
- Bingol H, Cingoz F, Yilmaz AT, Yasar M, Tatar H (2004) Vascular complications related to lumbar disc surgery. J Neurosurg Spine 100(3 Suppl spine): 249-253.
- Goodkin R, Laska LL (1998) Vascular and visceral injuries associated with lumbar disc surgery: medicolegal implications. Surg Neurol 49(4): 358-370.
- Szolar DH, Preidler KW, Steiner H, Riepl T, Flaschka G, et al. (1996) Vascular complications in lumbar disc surgery: report of four cases. Neuroradiology 38(6): 521-525.
- Bierdrager E, Van Rooij WJ, Sluzewski M (2004) Emergency stenting to control massive bleeding of injured iliac artery following lumbar disk surgery. Neuroradiology 46(5): 404-406.
- Lange M, Fink U, Philipp A, Oeckler R (2002) Emergency diagnosis with spiral CT angiography in case of suspected ventral perforation following lumbar disc surgery. Surg Neurol 57(1): 15-19.
- Loh SA, Maldonado TS, Rockman CB, Lamparello PJ, Adelman MA, et al. (2012) Endovascular solutions to arterial injury due to posterior spine surgery. J Vasc Surg 55(5): 1477-1481.
- Kokotsakis J, Misthos P, Sakellaridis T, Farsaris D, Anagnostakou V, et al. (2010) Emergent endovascular repair as damage control step of aortic injury after posterior spinal instrumentation. Ann Thorac Surg 89(4): 1304.
- Bautista Hernández V, Moya J, Martinell J, Polo ML, Fraile J (2002) Successful stent-grafting for perforation of the thoracic aorta by an intraaortic balloon pump. Ann Thorac Surg 73(3): 956-958.
- Zhou W, Bush RL, Terramani TT, Lin PH, Lumsden AB (2004) Treatment options of iatrogenic pelvic vein injuries: conventional operative versus endovascular approachdcase reports. Vasc Endovascular Surg 38(6): 569-573.
- Leslie M (2011) Thoraco-Abdominal Aorta. Milano: Springer-Verlag.
- Inamasu J, Guiot BH (2006) Vascular injury and complication in neurosurgical spine surgery. Acta Neurochir (Wien) 148(4): 375-387.
- Ganesan C, Petrus L, Ross IB (2012) Regarding the possibility of anterior vascular injury from the posterior approach to the lumbar disc space: an anatomical study. Spine 37(22): E1371-1375.
- Bolesta MJ (1995) Vascular injury during lumbar discectomy associated with peridiscal fibrosis. J Spinal Disord 8(3): 224-227.
- Huttman D, Cyriac M, Yu W, O'Brien JR (2016) The unusual presentation of a vascular injury after lumbar microdiscectomy: case report. J Neurosurg Spine 24(3): 381-384.

 Research Article
Research Article