Abstract
Type 2 thyroplasty (TP2) has been performed as a surgical treatment for adductor spasmodic dysphonia (AdSD) using a titanium bridge (TB), because of its strength and excellent stability. We report a case that did not show voice deterioration after removal of the TB due to mucosal perforation originating from the lower TB during long-term follow-up after TP2. This is the first report of a complication of TB use during long-term follow-up after TP2. A 23-year-old female patient presented with a speech disorder in 201X and was diagnosed as having AdSD. At first, thyro-arytenoid myectomy (TAM) was performed, followed subsequently by botulinum toxin injection therapy (BT therapy). However, despite these treatments, the patient’s voice failed to improve. Finally, TP2 was performed in 201X+1. The postoperative voice was satisfactory, but her voice deteriorated again in 201X+4. Formation of granulation tissue was detected in the subglottic space, as a result of a mucosal break caused by the lower TB. Despite conservative therapy with medications, the granulation tissue developed and disappeared repeatedly. Therefore, operation for removal of the TB was performed under local anesthesia in 201X+5. The intra-operative voice was not spasmodic, and the postoperative voice also remained unchanged. The granulation tissue disappeared. Currently, the postoperative voice profile is 0/21 mora, and G0. After the removal of the TB, the upper TB maintained the expansion of the thyroid cartilage and the voice remained unchanged after its removal. Complications arising from TBs must be borne in mind. After TP2, if granulation tissue appears in the subglottic space, removal of the TB should be considered.
Keywords: Adductor Spasmodic Dysphonia; Type 2 Thyroplasty; Titanium Bridge; Complications
Abbreviations: AdSD: Adductor Spasmodic Dysphonia; TB: Titanium Bridge; TAM: Thyro-Arytenoid Myectomy,
Introduction
Adductor spasmodic dysphonia (AdSD) is caused by local dystonia of the thyroarytenoid muscle. Isshiki reported the usefulness of type 2 thyroplasty (TP2) as a surgical treatment for this condition [1-4]. TP2 involves the use of a titanium bridge (TB) to open the thyroid cartilage and move the bilateral vocal cords outward. At our department also, we use TBs for TP2. We report a case in which the voice showed no deterioration after the removal of a TB owing to mucosal perforation caused by the lower TB during long-term follow-up after TP2. This is the first report of a complication caused by TB use during long-term follow-up after TP2.
Case
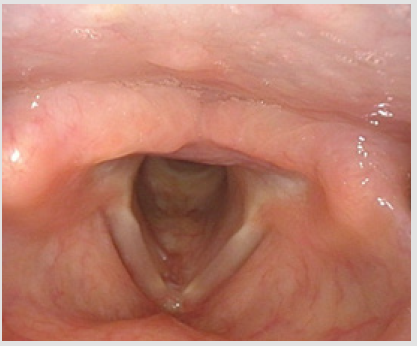
A 23-year-old female patient presented to us with a speech disorder in 201X and was diagnosed as having AdSD. At first, thyro-arytenoid myectomy by Muta method (TAM) was performed, followed subsequently by botulinum toxin thyroarytenoid injection therapy (BT therapy). However, despite these treatments, her voice failed to improve. Finally, TP2 was performed in 201X+1. The postoperative voice was satisfactory, but her voice turned deteriorated again in 201X+4. Examination revealed formation of granulation tissue in the subglottic space (Figure 1), which was a result of a mucosal break caused by the lower TB. Despite conservative therapy with medications like tranilast, the granulation tissue formed and disappeared repeatedly (Figure 2). Therefore, operation for removal of the TB was performed under local anesthesia in 201X+5.
Figure 1: Endoscopic findings 4 years after TP2. Formation of granulation tissue is noted in the subglottic space (arrow). G3R3B3 MPT10s 0/21 Mora Jitter 24.88% Shimmer 5.87%.
Figure 2: Endoscopic findings after conservative therapy with medications such as tranilast Granulation tissue under the glottis showed a tendency to shrink, however the lower TB was exposed (arrow). G1R1B1 MPT12s 2/21 Mora Jitter0.52% Shimmer1.81%.
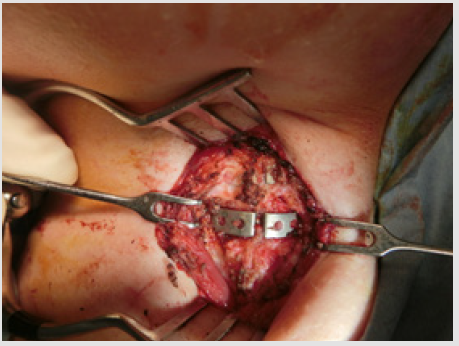
Intraoperative findings: A horizontal skin incision was made on the neck. The strap muscles were split at the central line, to expose the thyroid cartilage. Both upper and lower TBs were then fixed on the thyroid cartilage (Figure 3). The lower TB was removed under voice monitoring. No change of voice was noted immediately after removal of the TB, the recorded voice profile remaining Mora 0/21 and G0. No fistula was found in the lower TB extraction area, and no salivation was noted upon coughing. The removed part in the midline was covered with a strap muscle flap (Figure 4). The postoperative course was uneventful, and the granulation tissue and mucosal perforation disappeared (Figure 5). Currently, 3 months since the removal operation, the voice profile is maintained as follows: Mora method 0/21, GRBAS scale G0.After the removal of the lower TB, the upper TB maintained the expansion of the thyroid cartilage, and the voice did not change after the removal.
Figure 3: Both the lower and upper TBs were fixed to thyroid cartilage (arrow). The lower TB was removed under voice monitoring, but no obvious fistula formation was found.
Figure 5: Endoscopic findings 3 months after removal of the lower TB shows that the granulation under the glottis has disappeared. No perforation of the mucosa is seen either. Note: G0 MPT15s 0/21 Mora Jitter 1.60% Shimmer 1.44%
Discussion
In the original Isshiki method of TP2 [5], a silicon block (SB)
was used as the insert to maintain the expansion of the thyroid
cartilage. However, many problems, such as deviation of the SB, were
noted during the postoperative follow-up. In addition, the inward
migration material used in type 1 thyroplasty was also changed
from SB to Gore-Tex due to potential carcinogenicity problems, and
efforts were made to design and develop a TP2 spacer to replace
SB. Considering that titanium is a preferred material in terms of the
strength and biocompatibility, TP2 using TBs was first reported in
2002. TBs have strength and excellent stability, and Sanuki et al. 4)
reported the usefulness of TB in cases with failure of SB, titanium
mesh and titanium mini plate. According to that report, use of one
TB is insufficient for maintaining thyroid cartilage expansion. Since
the publication of this report, the Isshiki group has used two TBs
in all cases. There are no reports of any problems or complications
associated with the use of TBs, and this is the first case report of a
complication associated with TB use detected during postoperative
long-term observation after TP2.
Generally, as a treatment for formation of granulation tissue
if the infection is complicated, an antimicrobial agent is given,
and if it is not, tranilast or a steroid is given. However, in this case,
the granulation repeated developed and disappeared, and was
speculated as being a result of mucous membrane damage caused
by the TB. In this case, regeneration of the mucous membrane and
disappearance of the granulation could not be expected unless the
TB was removed. However, there was the strong fear that the TB
removal may cause voice deterioration. The patient was extremely
worried about a possible return of her spasmodic voice and said
that she would like to avoid worsening of the Mora score. This TB
removal operation was performed in the background of the abovementioned
conflict. The TB was removed under local anesthesia
with voice monitoring. We did not notice any voice deterioration.
It was speculated that the anchoring force of the expansion and
contraction over the several years after surgery and the opening
and maintenance force of the lower TB were superior to the force
of return to the original position after thyroid lateralization. The
force of return to the original position after lateralization of the
thyroid cartilage is supported by muscles attached to the thyroid
cartilage, such as the sternothyroid muscle, thyrohyoid muscle,
pharyngeal constrictor muscle, cricothyroid muscle, as well as
adductors of internal laryngeal muscles. It is thought that the
main causes of return of the cartilage to its previous position are
the restorative force and external forces exerted by muscles such
as the sternocleidomastoid muscle [6]. Fistula formation after
removal of the TB could be avoided. This was presumably since
the mucosal area covering the fistula was extremely small and that
covering the cervical muscles was firm. As the cause of the mucosal
perforation, it is possible that the airway mucous membrane at the
attachment site of the TB had become thinner with time. We think
that TB-derived mucosal perforation and granulation are difficult
to control by conservative treatment, and that TB removal should
be considered.
Conclusion
We encountered a complication associated with the use of TBs during TP2. We diagnosed the granulation tissue detected in the subglottic space as being the result of mucosal perforation caused by the lower TB and removed the TB. After the removal of the TB, the upper TB maintained the expansion of thyroid cartilage and the voice showed no deterioration after removal. TB-derived mucosal perforation is a complication that must be borne in mind by the attending physician. TB removal should be considered if the formation of granulation due to mucosal perforation caused by the TB cannot be conservatively treated.
Conflict of Interest
We have no disclosure to make that qualifies as a conflict of interest.
References
- Isshiki N, Tsuji DH, Yamamoto Y, Iizuka Y (2000) Midline lateralization thyroplasty for adductor spasmodic dysphonia, Ann Otol Rhinol Laryngol 109: 187-193.
- Isshiki N, Haji T, Yamamoto Y, Mahieu HF (2001) Thyroplasty for adductor spasmodic dysphonia: further experiences. Laryngoscope 111: 615-621.
- Sanuki T, Isshiki N (2007) Overall evaluation of effectiveness of typeⅡ thyroplasty for adductor spasmodic dysphonia. Laryngoscope 117(12): 2255-2259.
- Sanuki T, Isshiki N (2009) Outcomes of typeⅡ thyroplasty for adductor spasmodic dysphonia: analysis of revision and unsatisfactory cases. Acta Oto-Laryngologica 129(11): 1287-1293.
- Isshiki N, Yamamoto Y, Maeda HA (1999) New Surgical Treatment for Spasmodic Dysphonia.Practica Oto-Rhino-Laryngologica 92: 81-87.
- Kanazawa H, Isshiki N (2008) Complications in Type Ⅱ Thyroplasty Due to Inadequate Fixation. J Jpn Bronchoesophagol Soc 59: 497-505.

 Case Report
Case Report