Abstract
Objectives: To validate the effectiveness of the Undergraduate Orthopaedic Student Internship Programme (Ortho-SIP) in preparing final year students for the practice of medicine post-graduation.
Methods: A questionnaire based on a five-point Likert scale was given to the students upon completion of different components of the Ortho-SIP. Based on this scale, the number of variable reviews is collated, and individual summated Likert scale scores are calculated the overall improvement to students’ self-confidence, clinical efficiency, and clinical skills.
Results: Majority of responses from students who participated in the Ortho-SIP were favourable. 76 % of responses indicated a grade 4 and above (overall mean 3.9) for the quality of their experience in the internship programme. The mean summated Likert scale score for the students is 24.2/30. 83 % of responses indicated that they would recommend or strongly recommend the programme to their colleagues.
Conclusion: Students found the scenario case discussions and the practical skill stations relevant and enjoyable opportunities for them to practice clinical skills. We found that according to the students’ self-perception, they were more confident of their post-graduate medical practice and felt that their clinical efficiency and skills had benefited significantly from the programme. Integrating hands-on experiences into the final year of medical students’ education can enhance their learning and preparation for post-graduate practice.
Keywords: Medical education; Clinical competency; Orthopaedic student internship programme; Student readiness residency
Introduction
Medical students in their final year face the ever-real challenge of translating their knowledge into clinical skills and from the textbooks onto patients. With a change of role, students may be expected to feel a degree of anxiety and a lack of preparation [1,2]. Hospitals also recognize that new graduates are unprepared for their first clinical posts in terms of clinical skills and selfconfidence [3,4]. However, medical schools can facilitate this transition by implementing programmes that mitigate the concerns and uncertainties of the students and help them students achieve the self-confidence and competencies required of clinicians [4,5]. The curriculum designed for medical students needs to include or be supplemented with practical training in order to allow them to fully grasp their clinical skills and prepare them [6]. Additionally, there is only a short period of time before final year students take up the posts of house officers in hospitals with real patients. This puts the pressure on them to pick up these skills very quickly and proficiently.
A hands-on approach has been shown by many experiments to be the quickest way to learn and this is especially applicable to skillbased knowledge [7-9]. and hence is the recommended method to meet the need of students to pick up the skills quickly and proficiently. Recent literature indicates that clinicians whose skills are acquired through practice and by interacting with a simulation perform better than those whose skills are acquired through information alone [7-12]. In 2005, a revised final undergraduate year (Foundation Programme) was designed to focus on practical skills which included three eight-week rotations in medicine, surgery, and primary care. The students were graduates from King’s, Guy’s, and St. Thomas’ [13,14]. The majority of students involved in the study indicated marked increase in confidence and progression in perceived clinical skill competencies. The programme has since been introduced into 25 schools in the United Kingdom [10]. Multiple other studies have also noted that doctors in their first year of practice and students involved in bridging programmes most appreciate the opportunity to shadow seniors and gain their bearings in their new workplace environment before being expected to take on the responsibility [15,16]. Although not for as long a period as the Foundation Programme or the currently compulsory one-year Pre-Registration House Officer (PRHO) in the UK, our SIP shares the same aims to mentally prepare the students by instilling in them the same self-confidence and proficiency in clinical skills.
Methodology
Description of the Orthopaedic Student Internship Programme (Ortho-SIP)
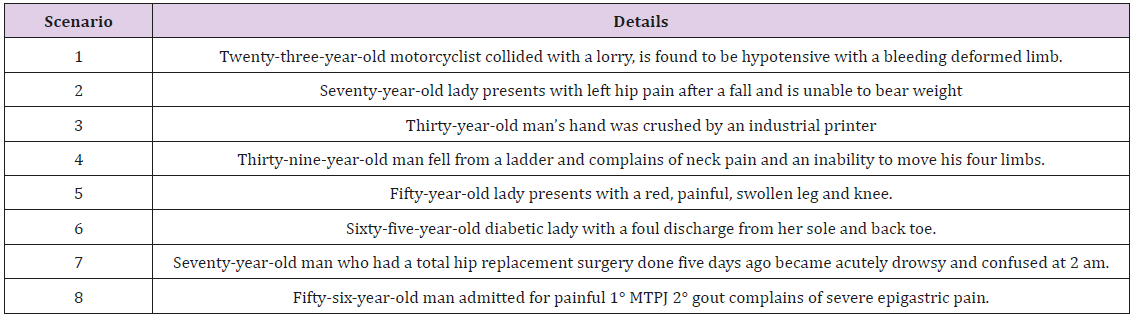
The Ortho-SIP was an education tool first introduced in 2008 to transfer medical knowledge into clinical skills for the final year medical student in the preparation for student readiness to practice medicine after graduation. 17 Every year since then, a third of the cohort is posted to the Ortho-SIP. The remaining two thirds of the cohort are posted to either General Surgery SIP or Obstetrics and Gynaecology SIP [17]. It consisted of a first day skill course consisting of case scenario discussions and practical skill stations emphasizing on clinical decision-making thought process and clinical skills enhancement. The case scenario discussions were situational in nature, each lasting fifteen minutes and led by professors (Table 1). The skills stations also lasted fifteen minutes each and practical skills imparted to the students included using plaster, traction, X-rays, dressing, drains, suturing, venepuncture, lines and blood culture, urinary catheterization in trauma patients, and log rolls. Based on the feedback from the 2008 and 2009 participants, they had already had sufficient prior experience with venepuncture. As a result, in the 2010 Ortho SIP 1 day skills course, the “Venepuncture, Lines and Blood Pressure” station was replaced with a knee aspiration station, to provide the students with as much exposure to clinical skills as possible. Simulation-based clinical skills training provided the students with a safe environment in which they had the confidence to take responsibility. It allowed them to make mistakes, reflect, obtain feedback, and repeat [15].
The 1day foundation skills course was followed by a 4-week student internship which comprised of job-shadowing the junior doctors under the supervision of registrars and consultants in the wards, as well as a didactic tutorial at the end of each week [17]. This was conducted over a structured work schedule including a studyguide, mid-posting programme director review, and end-posting assessment of the student by doctors and nurses. 17 This allowed them to gain hands-on training in the management of surgical patients and observe the practical procedures they had practiced during the skills course, such as taking blood and setting up traction. They could also observe the major operating theatre, day surgery operating theatre, and taking night calls [17]. The Ortho- SIP was established with the aim of educating the students not only through theory but also practice, by giving them more hands-on exposure. The hands-on experiences should allow students to pick up the skills with greater efficiency and proficiency, as well as build the confidence required of them when working with hospital staff and patients as house officers. The aim of this study is to validate the effectiveness of the Ortho-SIP programme by evaluating the students’ self-perceptions of «clinical readiness”.
Participants
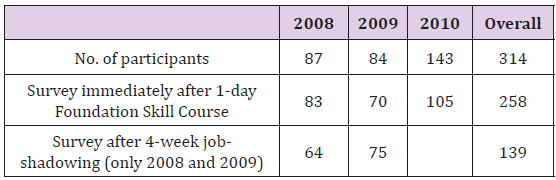
The participants of the programme as well as the survey were students in their final year of medical school. The overall response rate for the 1-day Ortho-SIP Skill course was 83/87 (95 %), while the response rates for the years 2008, 2009, 2010 were 83/87 (95 %), 70/84 (83 %), 105/143 (73 %) respectively. Overall Response rates for the survey conducted after the 4-week job-shadowing was 139/171 (81 %), while the response rates for the years 2008 and 2009 were 64/87 (74 %) and 75/84 (89 %) respectively (Table 2).
Survey Development
In order to assess the students’ self-perception of “clinical readiness”, a prospective review of the Ortho-SIP effectiveness using customized student questionnaires on a five-point Likert scale was conducted. Self-perception of “Clinical readiness” is defined as a demonstration of confident, effectively performed clinical skill. The questionnaire was hence designed to determine the students’ perception of their confidence, clinical effectiveness, and level of proficiency of their practical skills. The “clinical readiness” is then quantified by the mean obtained from the summated individual Likert scale score measuring improvement of student confidence, clinical effectiveness, and clinical skill enhancement. These surveys were conducted immediately after the 1-day foundation skills course, as well as after the 4-week job-shadowing experience, and also into their post-graduate surgical practice. A score of 1 referred to no benefit gained, 2 to below average, 3 to average, 4 to a good experience, and 5 to a significantly beneficial experience. The survey also included questions for students to assess the usefulness of each individual component of the Ortho-SIP, for the administration to make improvements to the programme at the time. There are no major changes to the programme between the years that could affect the students’ learning through the Ortho-SIP.
Data Analysis
As each year’s gender and race ratios were uniform, we found
it acceptable to analyses the data according to years. To measure
the success of the programme as an education tool, only scores of
4 and above were considered significant and only responses that
indicated 4 and above were counted into the number of favourable
reviews [18]. The individual summated Likert scale score assessing
self-confidence, clinical efficiency calculated based on the six
questions regarding confidence, clinical effectiveness, and clinical
skills based on the 1-day foundation skills course and the 4-week
job-shadowing. The six questions are:
1) How did the foundation skills course increase your
confidence to begin your sudent internship attachment?
2) How did the foundation skills course help you to be more
effective in the ward?
3) How did the foundation skills course improve your clinical
skills for medical practice?
4) How did the internship programme increase your
confidence in becoming a house officer?
5) How did the internship programme help you to be more
effective in the ward?
6) How did the internship programme improve your clinical
skills for medical practice?
Results
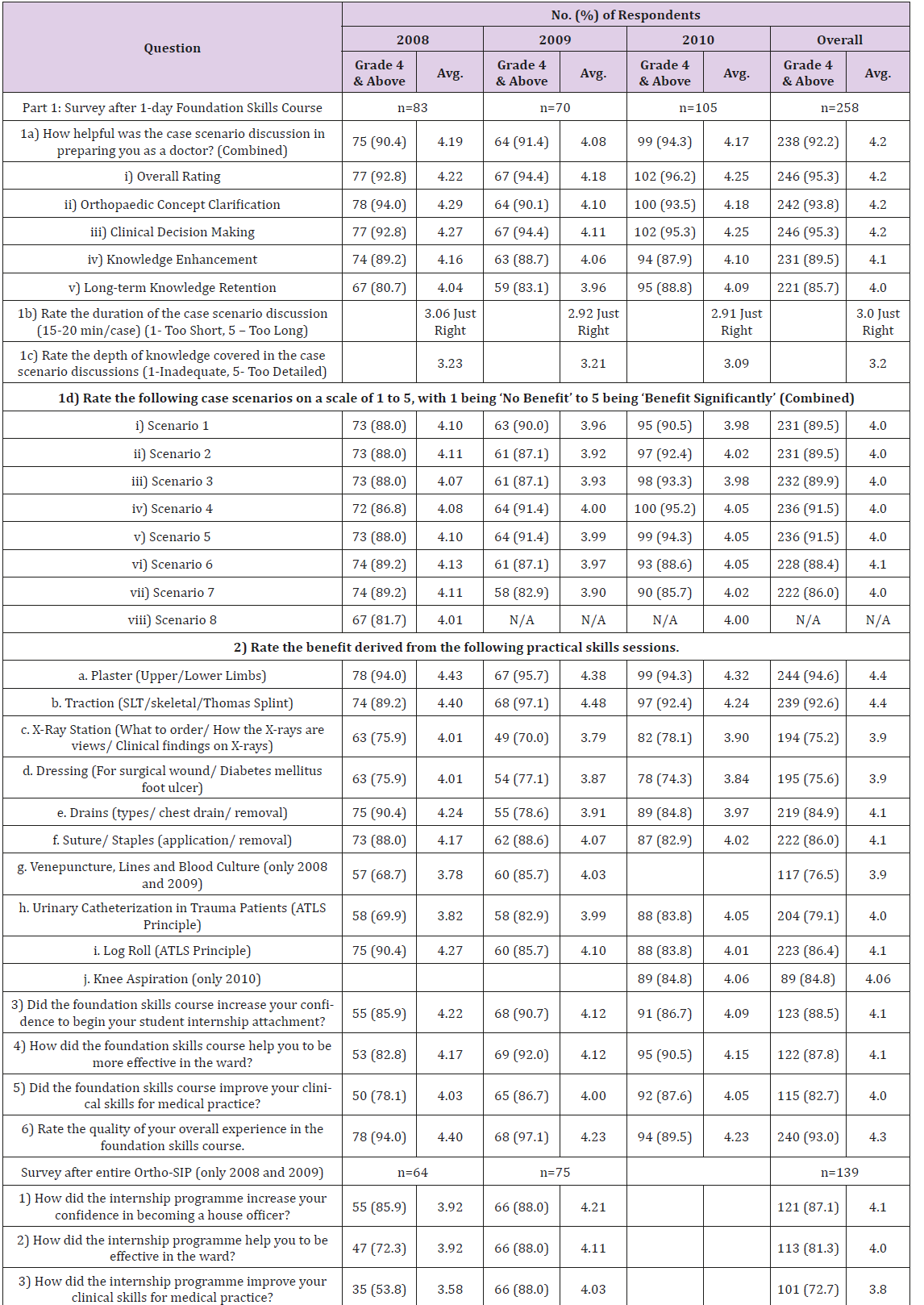
All 308 Ortho-SIP student-interns had completed and passed the programme over 6 4-week SIP postings in the years 2008, 2009, and 2010. Feedback from 258 (83 %) of the 308 student-interns were collected on the respective days of the skill course. 95 % (n=258) of students responded with a grade 4 and above (mean 4.3 range 3-5) of having beneficial experiences during the 1-day course. 92.2 % students reported a grade 4 and above (mean 4. range 3-5) case scenario discussions effectiveness in guiding clinical decision making, concept clarification, knowledge enhancement and aid in long term knowledge retention respectively. For the practical skills sessions, the survey showed that 84 % of students reported a grade 4 and above (mean 4.1 range 1-5) beneficial experiences. The mean overall grade for case discussions and skill stations were 4.1 and 4.1.
From responses collated after the 4-week student-internship, 83 % students had a grade 4 and above (mean 4.1 range 2-5) increased in confidence of becoming a “House Officer” upon medical graduation. 87 % students reported a grade 4 and above (mean 4.0 and 3.8, range 2-5) improvement in effectiveness during hospital ward duties and skill enhancement after student-internship. Responses indicate that an above average (grade 4 and above) increase in confidence, clinical effectiveness, and skill enhancement was experienced by 87 % of students due to the foundation skill course and 78 % of students due to the job-shadowing experience. The mean of the summated individual Likert scale scores measuring students’ confidence, clinical effectiveness, and clinical skill enhancement is a 24.2 upon 30. 83 % of students responded that they would recommend or strongly recommend the Ortho-SIP to their colleagues [19,20] (Table 3).
Discussion
All components were rated a grade 4 and above (beneficial to
significantly beneficial) by at least 75% of students, indicating that
the contents of the programme were able to engage and benefit
most of the students.
The case scenario discussions and practical skills station in
particular drew favourable comments in the open-ended section of
the survey. The duration of the case scenario discussion was just
right and the depth of the knowledge discussed matched that of
their lecture notes, being neither inadequate nor too detailed. This
gives credence to the effectiveness of problem-based approaches
as a tool in medical education, in reducing the anxiety faced by
students in decision-making [17,18]. Responses commended the
good organization and cited the enthusiasm of the coordinators as
one of the reasons that made the course so enjoyable. This result
coheres with the conclusions of previous studies, that information
as well as hands-on experiences through simulation makes the
best combination of learning [7-12]. Simulation complements the
experiential learning in wards and a combination of procedural
experience and skill programmes increases self-reported
confidence [14,15].
Feedback for improvement included giving more time for the
practical skills station or holding the foundation skills course over
two days instead of one, to prevent the programme from being too
rushed. Students appreciated having the professors there to lead
the workshop.
“Ortho workshop and suture workshop were very good, highly
recommended for future students.”
“Suturing/Traction workshops will be useful.”
“Workshop is too packed. Should spread out over 2-3 days. Too
intensive.
Otherwise very comprehensive workshop. Increases my
confidence to start SIP.”
“Very good programme. Would have been better if increased
time for practical skills.”
In terms of confidence and applicability of the newly acquired
knowledge to clinical skills and future medical practice, both the
foundation skills course and the internship programme drew
positive reviews (mean grade of 4.1, 4.1, 4.0, 4.1, 4.0, and 3.8, range
1-5). This indicates that at least from the perception of the students,
the Ortho-SIP was successful in boosting their confidence and the
contents were applicable to their future functions as house officers.
Regarding the 4-week job-shadowing, most suggestions were
about shortening the time period to about 2-3 weeks. This would
allow them to have more time to study for their final MBBS exams.
Students also felt that two weeks would have been long enough to
be exposed to the different cases and the different approaches of
clinical management in Orthopaedics. Other suggestions include
shortening the Ortho-SIP and afterward doing a rotation with
General Surgery SIP to be exposed to a wider variety clinical
conditions and their management.
“Too long. Very time-consuming. Weekends used as well. Need
time to study for MBBS.”
“Following Medicine SIP 4/42, Ortho-SIP is too long. Preferably
shortened to 2-3/52 and deliver time to Paeds.”
“Rotation to each ward would be more beneficial so that we can
see a variety of cases.”
These results cohere with that of other studies in that, although
job-shadowing on the whole value-adds to the students’ learning,
there is a limit to the benefit derived from job-shadowing compared
to the time spent.16 At the same time, not all students appreciate
the opportunity to job-shadow [16].
Responses also showed that the job-shadowing was carried
out more efficiently when organized into teams, as they could learn
more by working with Registrars and Consultants. This coheres
with the results of previous studies that indicate that the jobshadowing
during the transition year is best facilitated in teams,
where students can interact with members of allied healthcare
[2,4,13,14,16].
“Team-based management seems preferable for patient care
and junior staff teaching.”
“Team-based system will be better for our learning.”
“The House Officers being ward-based, had difficulty rounding
with the consultant. Although it was different for the team-based
organization, it offered a different experience. I must say most of us
had difficulty adjusting to this system and felt that the team-based
organization was a more organized approach.”
The 82% of students who would recommend the Ortho-SIP
is a reflection of how the components of the programme are not
redundant, as they felt that future years of medical students should
also have the same beneficial experiences.
The overall positive feedback from this study gives support for
the importance and effectiveness of implementing a programme
that helps medical students transit from their final year to working
in hospitals as housemen [1,2,4-6,13,14]. It also gives credit to a
more hands-on approach when educating students – allowing them
to learn by having them carry out the procedures and immersing
them, with some guidance, in the environment that they will
eventually work in.
Limitations of the Study
While the Likert scale can reflect the level of effectiveness of each component of the programme, it may not be able to establish cause and effect, as it would not be able to reflect the actual factors that contributed to the success of the different components of the programme. As the different surveys were conducted at different times, not all the participants were available to give feedback, hence there may be unaccounted for discrepancies in the results of the surveys. However, the surveys represented at least 75% of the participants and hence can still be considered a reliable source. Though the overall response rates are high, there is a potential for a non-response bias. Students who chose not to respond to the surveys may have had less favorable experiences during the Ortho- SIP than those who did respond.
Conclusion
In conclusion, we found that our Ortho-SIP is beneficial for final year students. Not only did they enjoy being able to translate their medical knowledge into practical skills, they were able to do so proficiently and learn from their seniors how to do so in a hospital setting. This in turn led them to have more self-confidence and project “clinical readiness” for when they enter their post-graduate medical practice. This gives credence to the importance of having a transitional programme for students in their final year, as well as the incorporation of simulation and shadowing.
Acknowledgement
None.
Conflict of Interest
The authors declare they have no conflict of interest.
References
- Tweed MJ, Badd W, Child S, Wilkinson TJ, Weller JM (2010) How the trainee intern (TI) can ease the transition from undergraduate education to postgraduate practice. NZMJ 123(1318): 81-91.
- Brennan N, Corrigan O, Allard J, Archer J, Barnes R, et al. (2010) The transition from medical student to junior doctor: today’s experiences of tomorrow’s doctors. Medical Education 44(5): 449-458.
- Matheson C, Matheson D (2009) How well prepared are medical students for their first year as doctors? The views of consultants and specialist registrars in two teaching hospitals. Postgraduate Medical Journal 85(1009): 582-589.
- Berridge E, Freeth D, Sharpe J, Roberts CM (2007) Bridging the gap: supporting the transition from medical student to practicing doctor-a two-week preparation programme after graduation. Medical Teacher 29(2-3): 119-127.
- Whitehouse CR, O Neill P, Dornan T (2002) Building confidence for work as house officers: student experience in the final year of a new problem-based curriculum. BMC Medical Education 36(8): 718-727.
- Moercke AM, Eika B (2002) What are the clinical skills levels of newly graduated physicians? Self-assessment study of an intended curriculum identified by a Delphi process. Medical Education 36(5): 472-478.
- Hansen E, Marmor M, Matityahu A (2012) Impact of a three-dimensional “hands-on” anatomic teaching module on acetabular fracture pattern recognition by orthopaedic residents. J Bone Joint Surg Am 94(23): e1771-e1777.
- Buerkle B, Pueth J, Hefler LA, Tempfer Bentz E, Tempfer CB (2012) Objective structured assessment of technical skills evaluation of theoretical compared with hands-on training of shoulder dystocia management: a randomized controlled trial. Obstetrics & Gynecology 120(4): 810-814.
- El Khoury LH, Saab B, Musharrafieh U, Antoun J (2012) Impact of a 3-day OSCE workshop on Iraqi physicians. Family Medicine 9: 627-632.
- Fann JI, Caffarelli AD, Georgette G, Howard SK, Gaba DM, et al. (2008) Improvement in coronary anastomosis with cardiac surgery simulation. The Journal of Thoracic and Cardiovascular Surgery 136(6): 1486-1491.
- Leong JJ, Leff DR, Aggarwal R, Reilly P, Atkinson HDE, et al. (2008) Validation of orthopaedic bench models for trauma surgery. J Bone Joint Surg Br 90(7): 958-965.
- Datta V, Bann S, Beard J, Mandalia M, Darzi A (2004) Comparison of bench test evaluations of surgical skill with live operating performance assessments. J Am Coll Surg 199(4): 603-606.
- Lempp H, Seabrook M, Cochrane M, Rees J (2005) The transition from medical student to doctor: perceptions of final year students and preregistration house officers related to expected learning outcomes. Int J Clin Pract 59(3): 324-329.
- Matheson CB, Matheson DJ, Saunders JH, Howarth C (2010) The views of doctors in their first year of medical practice on the lasting impact of a preparation for house officer course they undertook as final year medical students. BMC Medical Education 10(48).
- Stolarek I (2007) Procedural and examination skills of first-year house surgeons: a comparison of a simulation workshop versus 6 months of clinical ward experience alone. NZMJ 120(1253): U2516.
- Jones A, Willis SC, Mcardle PJ, O Neill P (2006) Learning the house officer role: reflections on the value of shadowing a PRHO. Medical Teacher 28(3): 291-293.
- http://medicine.nus.edu.sg/os/undergraduate/year5/html
- Jamieson S (2004) Likert scales: how to (ab)use them. Medical Education 38(12): 1217-1218.
- Evans DE, Roberts CM (2006) Preparation for practice: how can medical schools better prepare PRHOs? Medical Teacher 28(6): 549-552.
- Kneebone RL, Kidd J, Nestel D, Barnet A, Lo B, et al. (2005) Blurring the boundaries: scenario-based simulation in a clinical setting. Med Educ 39(6): 580-587.

 Research Article
Research Article