Abstract
The presence of ipsilateral aneurysm in the stenosis of the internal carotid artery is determined by CT angiography in 1.8-3.2% of cases. The literature describes the most varied options for treating this pathology: isolated or alternate, and now the method of simultaneous endovascular treatment - carotid stenting and endovascular embolization of aneurysm - is gaining popularity. The main difficulties associated with the choice of treatment tactics for such patients are associated with the stage, temporal parameters, the need to eliminate intracranial aneurysm, the evaluation of perioperative complications. In the clinical example, the hybrid approach is presented - simultaneous carotid endarterectomy and embolization of aneurysm. In certain cases (anatomical variants, the structure of atherosclerotic plaque, individual features), the application of this approach is more justified than the growing popularity of simultaneous endovascular treatment.
Keywords: Aneurysm of the brain; Atherosclerosis; Carotid Endarterectomy; Stenosis of the Internal Carotid Artery; Embolization
Short Communication
According to the literature in patients with hemodynamically significant lesions of precerebral arteries, angiography is detected in 5% of cases with intracranial aneurysm, and in 1.8-3.2% - ipsilateral aneurysm with stenosis of the internal carotid artery [1-3]. Currently, in the absence of randomized studies, there are no definite clinical recommendations on the tactics of treatment of this group of patients [4-6].
Materials and Methods
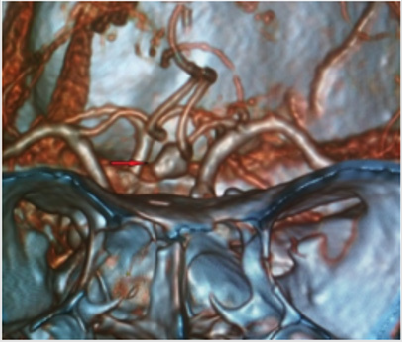
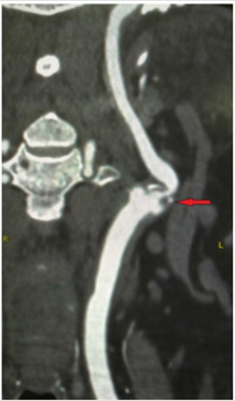
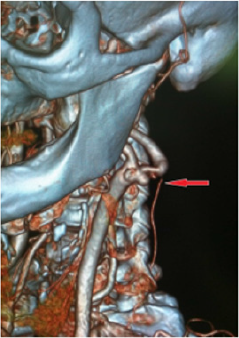
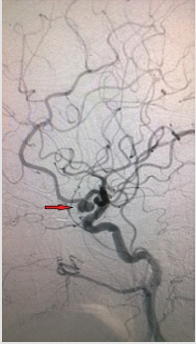
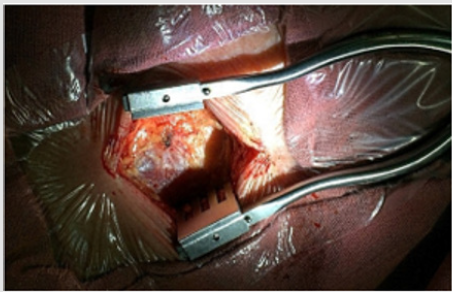
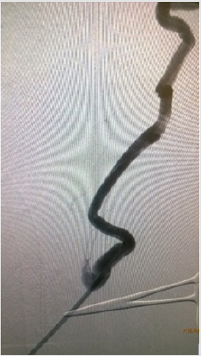
A clinical case of successful simultaneous hybrid surgical treatment of stenosis of the internal carotid artery and ipsilateral aneurysm of the anterior connective artery. An asymptomatic patient, 61 years old, entered the department of vascular surgery with complaints of headache, tinnitus, dizziness, unsteadiness of gait. According to ultrasound of brachiocephalic arteries, stenosis of the ICA on the left is 90%, atherosclerotic plaque is dense with ulcer, distal to the stenosis zone, C-shaped kinking, linear velocity of blood flow in the zone of deformation is 142 cm/s, in the stenosis zone is 340 cm/s. According to computed tomography, stenosis of the left ICA is 90%, saccular aneurysm of the left anterior communicating artery is 8.5x6 mm with a neck of 3 mm (Figures 1-3). According to cerebral angiography, stenosis of the left ICA is 85%, atherosclerotic plaque with ulcer, saccular aneurysm of the left anterior connective artery, irregularly shaped with a diverticulum, 7.5x5.3 mm in diameter with a neck 2.7 mm (Figures 4 & 5). Considering a dense atherosclerotic plaque with ulceration, a C-shaped kinking just behind the stenosis zone, as well as straightening of the artery during stent implantation to the optimal stenosis overlap position, which could lead to a pronounced hemodynamically significant septal kink, the decision was made to perform a simultaneous hybrid operation in volume CEA on the left and embolization of an aneurysm of the left anterior connective artery.
Figure 1: According to 3D computed tomography, saccular aneurysm of the anterior communicating artery.
Result
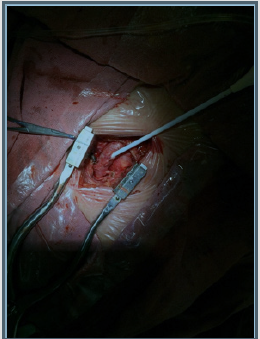
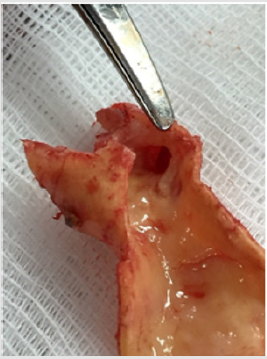
Anesthesiologic manual was performed in the volume of inhalation anesthesia by the sevoran. A 5.0 cm incision was made above the left CCA bifurcation site (Figure 6). CCA, ECA, ICA and the upper thyroid artery were injected. 5,000 units of heparin were injected intravenously. The arteries were bypassed and pinched by Geister atraumatic clamps. Longitudinal arteriotomy of the CCA with the transition to the internal carotid artery 15 mm, endarterectomy from the bifurcation and the mouth of the ICA. Atherosclerotic plaque is dense with an ulcer, the residual lumen is about 10%. Sewing of an arteriotomy with a thread of medpropilen 6/0 of Covidien. At the proximal end, the formation of the pouch with the femoral introducer Prelude 6F (Merit Medical), the parallel removal of the clamps (Figure 7). The ICA occlusion time was 12 min. Microcatheter Headway 17 Micro Vention (Terumo) is inserted into the aneurysm cavity by the 0,014 wire Micro Vention (Terumo). The aneurysm embolization was performed with Axium 3D (EV3) coil 8x20 mm, 7x30 mm, 2x6 mm. On control angiography, the aneurysm cavity is completely embolized, the blood flow through the anterior connective and anterior cerebral arteries of TICI III (Figure 8). Microcatheter removed. The duration of the endovascular stage was 40 min. On control angiography, an atherosclerotic plaque of the internal carotid artery is not present (Figures 9 & 10). The total operation time is 95 minutes. The patient is extubated after 30 minutes. Transferred from the intensive care unit after 4 hours. On control ultrasound after 3 days, the reconstruction zone is passable, the linear blood flow velocity at all sites does not exceed 100 cm/s.
Discussion
According to the literature, earlier the most frequently used treatment method for such a tandem pathology was CEA, followed by dynamic monitoring of the state of the aneurysm [1,4,7-9]. According to the only meta-analysis conducted in 2012, which included 141 observations, in 73.7% of cases the intervention was performed only on the internal carotid artery (in 91.3% of them CEA), in other cases, the methods alternated in different ways simultaneously or in stages [1]. The percentage of rupture of aneurysms in the early and remote postoperative periods after isolated CEA ranged from 0% to 5.3% [1,5]. However, in the vast majority of cases, the size of aneurysms in the observations did not exceed 7 mm [3,10]. Currently, the most popular is the method of simultaneous endovascular treatment - CAS and aneurysm embolization. In some clinics, two-stage treatment is preferred - CAS and after 3 weeks embolization of the aneurysm, with mandatory monitoring of blood pressure after the first stage [6]. Also, with not pronounced stenosis of the ICA and stable ASB, embolization of the aneurysm is possible, and the second stage in a month is CAS [11]. We have not encountered a hybrid treatment option for this pathology in the literature.
Conclusion
Due to the lack of evidence base in such patients, the decision on the tactics of treatment should be made by a consortium of physicians in the vascular surgeon, endovascular surgeon, neurosurgeon, anesthesiologist. Based on the analysis of the articles, the clinical approach to the treatment of such a group of patients was first applied.
Conflict of Interest
The authors declare no conflict of interest.
References
- Khan UA, Thapar A, Shalhoub J, Davies AH (2012) Risk of intracerebral aneurysm rupture during carotid revascularization. J Vasc Surg 56(6): 1739-1747.
- Bouri S, Thapar A, Shalhoub J, Jayasooriya G, Fernando A, et al. (2011) Hypertension and the post-carotid endarterectomy cerebral hyperperfusion syndrome. Eur J Vasc Endovasc Surg 41(2): 229-237.
- Emre Kaçar, Ömer Fatih Nas, Cüneyt Erdoğan, Bahattin Hakyemez (2015) Single-stage endovascular treatment in patients with severe extracranial large vessel stenosis and concomitant ipsilateral unruptured intracranial aneurysm. Diagn Interv Radiol 21(6): 476-482.
- Borkon MJ, Hoang H, Rockman C, Firas Mussa, Neal S Cayne, et al. (2014) Concomitant unruptured intracranial aneurysms and carotid artery stenosis: an institutional review of patients undergoing carotid revascularization. Ann Vasc Surg 28(1): 102-107.
- Siddiqui A, Vora N, Edgell RC, Callison RC, Kitchener J, et al. (2012) Rupture of a cerebral aneurysm following carotid endarterectomy. J Neurointerv Surg 4(5): 27.
- Wajima D, Nakagawa I, Wada T, Nakase H (2017) A trial for an evaluation of perianeurysmal arterial pressure change during carotid artery stenting in patients with concomitant severe extracranial carotid artery stenosis and ipsilateral intracranial aneurysm. Turk Neurosurg 29(5): 785-788.
- Ladowski JS, Webster MW, Yonas HO, Steed DL (1984) Carotid endarterectomy in patients with asymptomatic intracranial aneurysm. Ann Surg 200(1): 70-73.
- Ballotta E, Da Giau G, Manara R, Baracchini C (2006) Extracranial severe carotid stenosis and incidental intracranial aneurysms. Ann Vasc Surg 20: 5-8.
- Suh BY, Yun WS, Kwun WH (2011) Carotid artery revascularization in patients with concomitant carotid artery stenosis and asymptomatic unruptured intracranial artery aneurysm. Ann Vasc Surg 25(5): 651-655.
- Badruddin A, Teleb MS, Abraham MG, Taqi MA, Zaidat OO, et al. (2010) Safety and feasibility of simultaneous ipsilateral proximal carotid artery stenting and cerebral aneurysm coiling. Front Neurol 1: 120.
- Iwata T, Mori T, Tajiri H (2008) Successful staged endovascular treatment of a symptomatic cervical carotid bifurcation stenosis coupled with a coincidental unruptured cerebral aneurysm in the carotid distal segment. AJNR Am J Neuroradiol 29: 1948-1950.

 Short Communication
Short Communication