Abstract
Background: The second stage of labour is regarded as the penultimate climax of the birth of the foetus. It has been perceived as the most critical time particularly with exposure to asphyxial insults and resultant subsequent residual damages for the foetus. To allay this anxiety and avoid untoward perinatal outcomes, it has been invoked to justify arbitrary time limits and high rates of interference to expedite the delivery as a preventative intervention.
Objective: The main objective of this study is to determine perinatal outcome in relation to the duration of second stage in the Ethiopian settings in Addis Ababa.
Methods: A facility-based prospective cohort study was conducted on 3776 women who delivered in the four selected teaching hospitals in Addis Ababa, Ethiopia. It focused on the outcome of the babies born to these mothers and the labour partograph data. Neonatal outcomes that were examined included the presence of meconium-stained amniotic fluid,1st minute Apgar score of <7, 5th minute Apgar score of <7, incidence of perinatal asphyxia, sepsis, foetal injury, rates of admission to the intensive care unit and perinatal mortality. Mean with standard deviation for quantitative, percentage and proportion for qualitative variables were analyzed. A confidence limit of 95% and P value of <0.05 was adopted for the expression of statistical significance. Stepwise multiple logistic regression analysis was done, and adjusted odds ratios used to explore the real association. Chi square and Fischer exact tests were also employed for categorical variables.
Inclusion Criteria: term pregnancies beyond 37 completed weeks of gestation, singleton, vertex presentation, having reached or were referred either with established or prolonged second stage of labour.
Exclusion Criteria: preterm deliveries before 37 completed weeks of gestation, unknown or undetermined gestational ages, intrauterine foetal death before 2nd stage of labour and neonates with known lethal congenital anomalies.
Result: The mean duration of labour was 14.4 + 8.3 hours’ and second stage of labour was 62 min±44 (4-330min). It was found out that perinatal complications increased with increasing duration of second stage of labour. With a duration of second stage of labour of more than 1hour, Apgar score <7, respiratory distress syndrome, meconium aspiration syndrome and admission to neonatal intensive care unit became more inevitable.
Conclusion: There is increased probability of perinatal morbidity and mortality with prolonged second stage. Hence, labour should be re-assessed in order to avoid poor neonatal outcomes especially if second stage of labour is protracted beyond an hour.
Recommendation: national guideline on management of labour and perinatal audit at a central higher level ought to be in place.
Keywords: Perinatal Outcome; Second Stage; Labour; Addis Ababa-Ethiopia
Introduction
The second stage of labour (SSOL) is defined as duration from fully dilated cervix until delivery of the baby [1-7]. A prolonged second stage is depicted, in nulliparous patients, as a lack of continuing progress for 3 hours with regional anaesthesia or 2 hours without regional anaesthesia whereas for multiparous patients a lack of furtherance for 2 hours with or 1 hour without regional anaesthesia [5,6,8]. Every year an estimated 4 million babies die in the first 4 weeks of life and a similar number are stillborn. Three-quarters of neonatal deaths happen in the first week with the highest risk of death being on the first day of life. Almost all (99%) neonatal deaths arise in low and middle-income countries, the highest rates are generally registered in sub-Saharan Africa. The countries in these regions, with some exceptions, have made little progress in reducing such deaths in the past 10–15 years. Globally, the main direct causes of neonatal death are estimated to be preterm birth (28%), severe infections (26%), and asphyxia (23%). Maternal complications in labour carry a high risk of neonatal death, and poverty is strongly associated with an increased risk [9].
The World Health Organization recommends that decisions about curtailing the SSOL should be based on surveillance of the maternal and foetal conditions, and on the progress of labour. WHO also suggests that if there are signs of foetal distress or if the presenting part fails to descend there is a good reason to terminate the labour. However, if the mother’s condition is satisfactory, the foetus is in good condition, and there is evidence of progress in the descent of the foetal head, there are no grounds for intervention. In case of a second stage of >2 hours in nulliparous women and >1 hour in multipara; the chance of spontaneous delivery within a reasonable time decreases, and termination should be contemplated [8]. Before the introduction of continuous electronic foetal heart rate monitoring, the usual practice in managing the SSOL was to avoid a prolonged second stage and to expedite delivery by operative means in order to reduce the risk of foetal asphyxia [4]. This approach sometimes led to augmentation with oxytocin, difficult instrumental operative vaginal deliveries or too difficult Caesarean sections which could contribute to neonatal and maternal morbidity [3].
In Swedish study, overall rates of umbilical artery acidosis, birth asphyxia-related complications and admission to Neonatal Intensive Care Unit were 1.08, 0.63 and 6.42%, respectively. Rate of birth asphyxia- related complications gradually increased with duration of second stage: from 0.42% at <1 h to 1.29% at ≥ 4 h (adjusted RR 2.46 (95% CI 1.66 to 3.66)). For admission to NICU, corresponding rates were 4.97 and 9.45%, and adjusted RR (95% CI) was 1.80 (95% CI 1.58 to 2.04). Compared with duration of pushing <15 min, a duration of pushing ⩾ 60 min increased rates of acidosis from 0.57 to 1.69% (adjusted RR 2.55 (95% CI 1.51 to 4.30) from this it was concluded that prolonged durations of SSOL and pushing are associated with increased RRs of adverse neonatal outcomes [10]. However, no associations between prolonged second stage and adverse neonatal outcomes were reported by Molly et al. [11] and the duration of the second stage was not significantly associated with the risk of a low Apgar score or admission to NICU after adjustment for other factors as corroborated by Saunders et al. [12]. The balancing of optimal neonatal outcome while minimizing maternal morbidity and unnecessary interventions becomes an intricate challenge for obstetricians, residents, midwives, interns or others attending the parturient. The subject has not been addressed in the past and this study will hopefully establish a baseline on the effect of prolonged duration of the second stage and adverse perinatal outcomes.
Materials and Methods
The study was conducted from January 1 to July 30, 2018. It was carried out in Addis Ababa, the major urban centre and the capital city of Ethiopia. Regarding medical service, currently the city has more than 41 hospitals, 28 health centres, 35 health posts and more than 500 clinics. There are more than 12 public and more than 25 private hospitals in the city. Of the total 12 public hospitals, 3 of them, in addition to Tikur Anbesa Specialized Hospital, were selected by convenience and included in the study. All of the selected hospitals are capable of doing emergency caesarean section around the clock and provide intra partum foetal monitoring with foetal electrocardiography and Pinnard’s fetoscope auscultation mainly by residents, interns and midwives. The minimum sample size was calculated using Epi-info stat-calc of cohorts in reference to the study done in Taiwan [13]. We used the composite neonatal morbidity as an outcome measure with the exposed group being those who were delivered after duration of SSOL is >2hr, for whom the composite neonatal morbidity was put at 3.6% and the nonexposed group as those who were delivered before SSOL reached 2hr, for whom the composite neonatal morbidity was set at 5.8%.
We used the confidence interval of 95% and power of 80%. Based on the above, the sample size was 1550 for exposed and nonexposed each making the total sample size of 3100. Adding a 10% non-response rate of 310, the total sample size was set at 3410, but since it was convenient for us to collect additional data, we ended up with a total of 3776 women and their neonates constituting the study cohort. A structured, data collection tool format was prepared in English and pretested. Duration of the second stage was calculated as the number of minutes from the first cervical examination that revealed full dilation until delivery. Neonatal morbidities were defined on the basis of clinical diagnoses. Serious neonatal morbidities include 1st minute Apgar score <7, 5th minute Apgar score< 7, resuscitation need after delivery, meconium aspiration syndrome (MAS), respiratory distress syndrome (RDS), seizures, perinatal asphyxia (PNA), stillbirth, neonatal death, or admission to a Neonatal Intensive Care Unit (NICU). Following the data collection, each questionnaire was checked for completeness based on the code given during the collection.
Data was entered into SPSS version 20 statistical package and then checked, cleaned and analyzed using the software. Descriptive statistics like frequency tables, graphs and summaries were used to describe the independent variables. If outliers and missed values are found during exploration, causes were determined and if not, variables with missing value(s) and outliers were dropped out from the analysis. Cox regression was used to see the association between dependent and independent variables. Mean with standard deviation for quantitative variable, percentage and proportion for qualitative variable was analyzed. A confidence limit of 95% and p- value less than 0.05 was used as cut of point to see presence of statistical significance. To control the effect of confounding variables stepwise multiple logistic regression analysis was done and adjusted odds ratios (AORs) used to explore the real association. Chi- square and Fisher exact test also used for categorical variables. Ethical clearance obtained from the Department and the hospital directors.
Results
The median duration of labour was 12.3 hours while the mean was 14.4±8.3 with a range of 2-72 hours. The mean duration of SSOL was 62 min±44 (4-330min). The mean duration of SSOL in nullipara was 69.4±47.4 (5-330) min, in multipara 55.7±39.5 (4-288) and in grand multipara 52±32 (10-130) min. The mean duration of variability of SSOL in minutes of ZMH was significantly higher than BLH (83.8 versus 54.2 P< 0.001), GMH (83.8 versus 66.6 P<0.001) and Y12H (83.8 versus 59.4 P<0.001). Of the neonates, 1973(52.3%) were males and 1803(47.7%) females. A total of 3758(99.5%) of the mothers had live birth and 18(0.5%) were stillborn. Of the live births, 3496(92.6%) had a first minute Apgar score ≥7 while 280(7.4%) had Apgar score of <7. Regarding the fifth minute Apgar score, 3706(98.1%) had ≥ 7 Apgar score and 70(1.9%) <7 Apgar score. A total of 328(8.7%) neonates were admitted to NICU; 135(3.6%) had respiratory distress syndrome (RDS); 60(1.6%) meconium aspiration syndrome (MAS); 2 (0.1%) birth injury; 10(0.3%) early onset neonatal sepsis (EONS); 5(0.1%) perinatal asphyxia (PNA) ; 9(0.2%) failure to suck and moreover 601(15.9%) of the neonates had one or more perinatal complications.
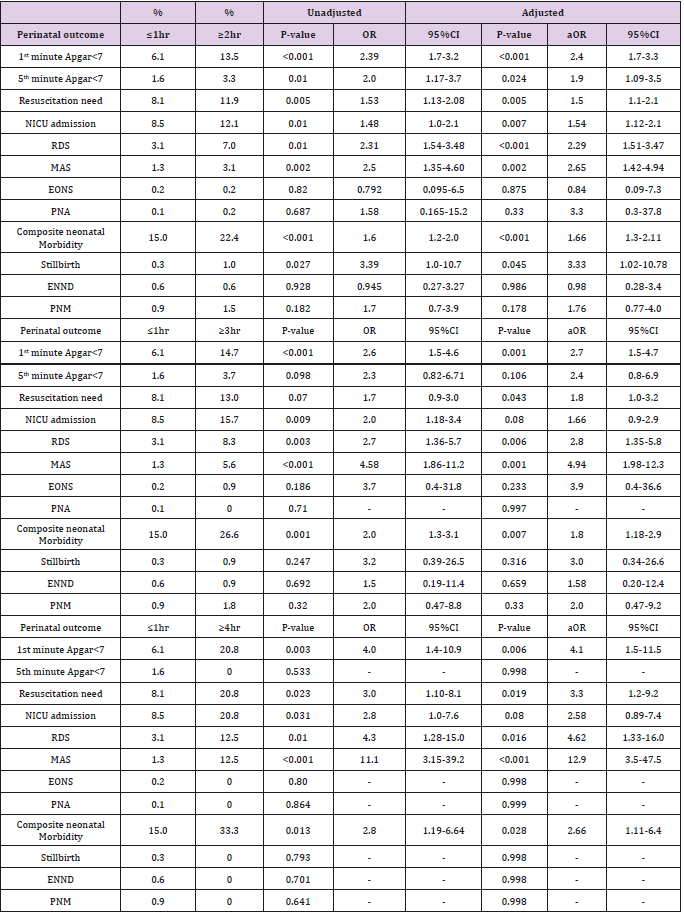
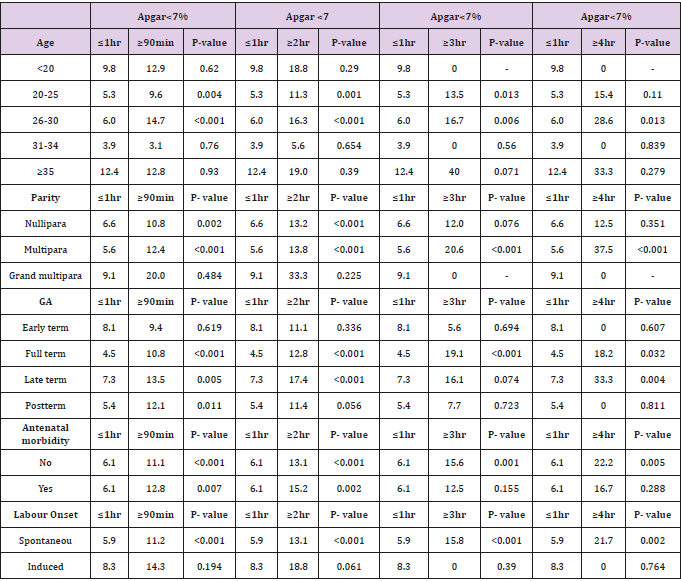
Duration of SSOL and weight of the baby has a statistically significant positive correlation (P=0.021). As duration of SSOL increases both 1st minute and 5th minute Apgar scores significantly decrease (P<0.001 for both). As presented in Table 1, this drop in Apgar score gets significant as duration of SSOL exceeds 1hr; first minute Apgar score <7 is significantly more in those mothers whose SSOL is ≥90min compared to ≤1hr (11.4% vs. 6.1%, P<0.001, aOR=2.02 and 95%CI is 1.5-2.6)), first minute Apgar score <7 is significantly more in those mothers with SSOL is ≥2hr compared to≤1hr (13.5% vs 6.1%, P<0.001, aOR=2.39 and 95%CI is 1.7), first minute Apgar score < 7 is more in mothers whose SSOL is ≥3hr compared to ≤1hr (14.7% vs. 6.1%, P<0.001), aOR=2.7 and 95%CI is 1.5-4.7). Even after controlling for the modifiers, 1st minute Apgar score being <7 is significantly associated with duration of SSOL (P=0.009, aOR=1.004 and 95% CI is 1.001 -1.006). Fifth minute Apgar score <7 is significantly more in those mothers whose SSOL is ≥90min compared to ≤1hr (3.3% vs. 1.6%, P<0.001, aOR=2.0 and 95%CI is 1.5-2.6), fifth minute Apgar score <7 is significantly more in those mothers with SSOL is ≥2hr compared to ≤1hr (3.3% vs. 1.6%, P<0.024, aOR=1.9 and 95%CI is 1.09-3.5).
Significantly more babies needed resuscitation in those mothers whose duration of SSOL is ≥2hr compared to ≤1hr (11.9% vs. 8.1%, P=0.005, aOR=1.5 and 95%CI is 1.1- 2.1), ≥3hr compared to ≤1hr (13.0% vs. 8.1%, P=0.043, aOR=1.8 and 95%CI is 1.0-3.2)(Table 1).There was no significant association between duration of SSOL with either duration of NICU stay or NICU outcome after admission. Overall, for every minute increment in duration of SSOL the neonates are 1.003 times more likely to have bad perinatal outcome (P=0.001, aOR=1.003 and 95%CI is 1.001- 1.005). NICU admission rate is significantly more common in those whose duration of SSOL is ≥2hr compared to ≤1hr (12.1% vs. 8.5%, P=0.007, aOR=1.54 and 95%CI is 1.1-2.1). After controlling for confounders NICU admission rate has significant positive association with duration of SSOL (P=0.038, aOR=1.003 and 95% CI is 1.000-1.005) (Table 1). MAS is more common in neonates whose duration of SSOL is ≥90min compared to ≤1hr (2.6% vs. 1.3%, P=0.007, aOR=2.1 and 95%CI is 1.2-3.8) and ≥3hr compared to ≤1hr(5.6% vs. 1.3%, P=0.001, aOR=4.94 and 95% CI is 1.98-12.3).
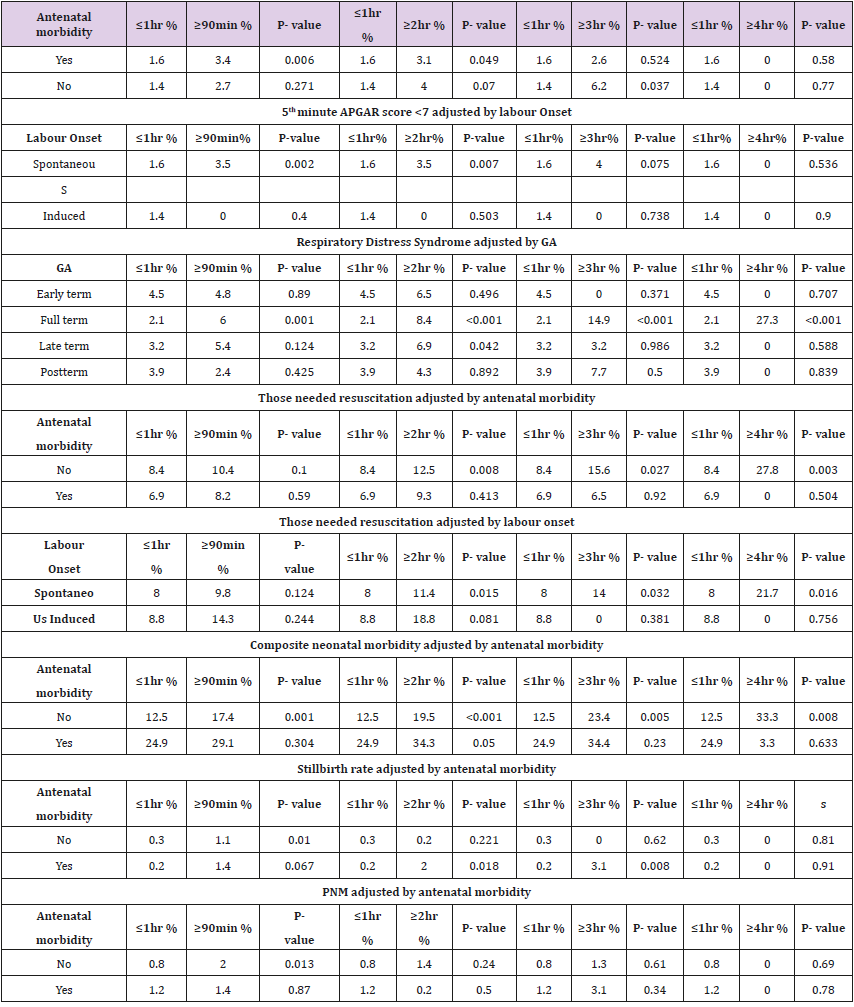
After adjusting for confounders MAS has a significant positive association with duration of SSOL (P=0.001, aOR=1.008 and 95% CI is 1.003-1.013) RDS is more common among neonates whose duration of SSOL is ≥90min compared to ≤1hr (5.1% vs. 3.1%, P=0.013, aOR=1.6 and 95%CI is 1.1-2.4), ≥2hr compared to ≤1hr(7.0% vs. 3.1%, P<0.001,aOR=2.29 and 95%CI is 1.51-3.47) and ≥3hr compared to ≤1hr (8.3% vs. 3.1%, P=0.006, aOR=2.8 and 95%CI is 1.35-5.8). Even after controlling for confounders RDS rate has increases with increasing duration of SSOL (P=0.004, aOR=1.005 and 95%CI is 1.002-1.009). Birth injury, EONS and PNA did not reveal significant association with duration of SSOL (P=0.156, P=0.693 and P=0.613 respectively). There was statistically significant association between antenatal morbidity and GA at delivery (P<0.001). Duration of labour and GA had a statistically significant positive association (P<0.001). However, duration of SSOL had no statistically significant difference with GA (P=0.740). There was statistically significant inverse relationship in perinatal morbidity with GA (P=0.014). Bad perinatal outcome had significant negative correlation with GA (p=0.018) as documented in (Table 2).
The median duration of NICU stay was 24hours while the mean was 52±55 (0.30-168) hrs. Two hundred sixty five (82.8%) of the neonates admitted to NICU discharged improved while 12(3.8%) of the neonates admitted died. Furthermore, 3(0.9%) were referred to other institution for better care and 40(12.5%) of them, nevertheless stayed in the NICU for 7 or more days. It was also found out that 70% of the neonatal deaths occurred within 24hours; 20 % occurred within 1-3 days and 10% occurred within 3 to 7days. 12 of the neonates died before they reached to NICU and 11 died at NICU making the total early neonatal death (ENND) 23(0.6%). The total PNM is 41(1.1%) as referred to in Table 3. Composite neonatal morbidity was significantly more common among neonates whose duration of SSOL is ≥90min compared to ≤1hr (19.4% vs. 15.0%, P=0.001, aOR=1.4 and 95%CI is 1.1-1.7), ≥2hr compared to ≤1hr (22.4% vs. 15.0%, P<0.001, aOR=1.66 and 95%CI is 1.3-2.11) and ≥3hr compared to ≤1hr(26.6% vs. 15.0%, P<0.007, aOR=1.8 and 95%CI is 1.18-2.9). Even after adjusting for confounding factors, there was a strong association of duration of SSOL with composite neonatal morbidity (P=0.001, aOR=1.003 and 95% CI is 1.001-1.005).
It was also observed that for those foetuses who died in SSOL, the time of foetal death is significantly associated with duration of SSOL (P=0.002) as presented in Table 3. The mean duration of SSOL is significantly longer in stillbirth compared to non-stillbirth (91.9min vs. 62.8min, P=0.005). After controlling for confounders, stillbirth rate has a significant positive association with duration of SSOL (P=0.009, aOR=1.010 and 95% CI is 1.003-1.018) but ENND did not have a significant association after controlling for confounders. PNM was significantly more prevalent in those whose duration of SSOL is ≥90min compared to ≤1hr (1.9% vs. 0.9%, P=0.024, aOR=2.1 and 95% CI is 1.1-4.1)
Table 3: Duration of SSOL and perinatal outcome adjusted by different factors.
5th minute APGAR score <7 adjusted by antenatal morbidity.
Discussion
There exist individual variations among women of spectral age groups with regard to duration of labour in general and second stage in particular. It is also highly variable with perinatal outcomes especially when second stage of labour is prolonged. In as much as there are studies that demonstrated no association between prolonged second stage of labour and neonatal morbidity risks [14- 20], others have established increased adverse neonatal outcomes and difficult mode of delivery [21-27]. This study is in line with the proponents of the latter. As duration of SSOL increased, both 1st minute and 5th minute Apgar scores significantly decreased. This significant drop in Apgar score starts as duration of SSOL exceeds 1 hour. This result is similar to the study by Ronald Mayanja and his colleagues which showed that the strength of association between duration of second stage and good perinatal outcome was inversely proportional to time, with best results registered when delivery occurred within 30minutes{ OR, 4.9, 95% CI (1.8-13.1)}, weakening towards duration of ≥60 minutes [28,29].
Nevertheless, the result is much higher than the study done in Taiwan which stated that 1st minute Apgar score <7 is 2.1% in those whose duration of SSOL <2hr compared to 1.8% whose duration of SSOL is > 2hr [13]. When adjusted for antenatal morbidity, the association between SSOL and drop in 1st minute Apgar score was significant only in those without antenatal morbidity at 1hr and for those whose duration of SSOL was ≥2hr compared to ≤1hr (9.0% vs 6.1%, P=0.03), implying that the low Apgar score in the group before 1hr was probably mainly due to the antenatal morbidity. But after 90 minutes, the association is significant regardless of antenatal morbidity demonstrating the effect of the duration of SSOL on the low first minute Apgar score which by itself is significant. When adjusted for gestational age, the duration of SSOL is significant only in those who are at full term which shows that the low Apgar score in the population for those who are early term, late term and postterm could be the resultant of either immaturity or dysmaturity. When adjusted for maternal age, the low first minute Apgar score is significant only in those whose age groups fall between 20 to 30 years.
This significant association in low Apgar score is seen in this age group probably because the low Apgar score in the two extremities of reproductive age is corollary to the high risks associated with the teenage pregnancy or advanced maternal age. However, the sequel could also be because of the small number of mothers in this population which might fail to show the significance. NICU admission rate significantly increased with duration of SSOL form 8.5 to 12.2% when duration of SSOL is ≤1hr compared to ≥2hr and further increased to 20.8% when duration of SSOL became ≥4hr; and these effects persisted even after we controlled for confounders. Our result is much higher when compared to the study done by Laughon et al. [26], which stated that NICU admission for those whose duration of SSOL is < 2hr is 4.1% and for those more than 2 hr is 6.2% [14]. Our study has also a much higher figure than the study done by Sandström [10] which stated that NICU admission for those whose duration of SSOL < 1hr is 4.97% , for those <2hr is 6.02% and for those ≥4hr 9.45% [30]. Such variations could be partly explained by the population studied and the study designs.
Overall composite neonatal morbidity significantly increased with increasing duration of SSOL from 15.0% when duration ≤1hr to 26.6% when duration ≥3hr and to 33.3% when the duration was ≥4hr. This figure is much higher than study done by Rouse et al. which stated that the rate of composite neonatal morbidity is 1.7% for those whose duration was <1hr, 2.9% for those whose duration is <2hr and 4.1% for whose duration is ≥4hr [25]. RDS and MAS also increase with duration of SSOL and the effect persists even after controlling for confounders for both. The SSOL on RDS increases from 3.1% on those whose duration is ≤1hr to 12.5% on whose duration is ≥4hr and on MAS it increases from 1.3% on those whose duration is ≤1hr to 12.5% on those whose duration of SSOL is ≥ 4hr. As these do have serious neonatal consequences, individualized timely and masterly management options should be exercised long before irreversible neonatal damages occurred. It was also observed that for those foetuses who died in SSOL, the time of foetal death was significantly associated with duration of SSOL (P=0.002).
The effect persisted even after controlling for confounders. The mean duration of SSOL was significantly longer in stillbirth compared to not stillbirth (91.9min vs. 62.8min, P=0.005) When adjusted for antenatal morbidity stillbirth rate was significantly associated with duration of SSOL only for those without antenatal morbidity at ≥90min when compared to ≤1hr. We could not find significant association after this time probably due to the small number of cases identified. This is in accordance with other studies [29]. ENND does not have significant association with duration of SSOL. However, PNM rate has rather unusual association when adjusted by antenatal morbidity which shows for those who have antenatal morbidity. PNM is significantly higher even in those whose duration of SSOL is <30min compared to ≥30min (3.1% vs 0.8%, P=0.031). So, we cannot justify for this mortality the duration of SSOL other than for the already present antenatal morbidity and its effect on the unborn foetus. It is worth acknowledging the fact that there exists a wide range of methodological variations among the different cited studies that dealt with prospectively collected data and retrospectively analysed material.
Nevertheless, they are convergent when univariate analysis is performed emphasizing the hazardous perinatal outcomes in relation to unduly prolonged second stage of labour. Hence, increasing duration of SSOL has a significant effect on low 1st and 5th minute Apgar, RDS, MAS, need for neonatal resuscitation and admission to NICU, stillbirth rate starting from 1hr and PNM starting from 90 minutes. In the presence of a high index of anticipation of poor outcomes, careful assessment of patients with antenatal morbidity need to be coupled with strict and continuous foetal monitoring either by CTG or FECG or on-to-one follow up should be in place at SSOL as even shorter durations can ENND up with a high PNM. In a nutshell, it is obvious that time is of the essence and the tipping point for decision and intervention based on the foetal condition, the management should thus be highly individualized [30]. We recommend that a national guideline for the management of labour in general and prolonged second stage of labour in particular, should be in place; and outmoded protocols be replaced in keeping with contemporary recommendations of the international community [30,31-34]. A regular perinatal audit and reporting should be introduced at municipality or ministerial level.
Acknowledgement
We are deeply indebted to the Department of Ob-Gyn, College of Health Sciences, School of Medicine of the Addis Ababa University for the ethical clearance, approval and support of the study. Our collegial appreciation goes to the medical directors of the hospitals involved in the study. We highly value the immense input of the data collectors, supervisors, reviewers and the secretarial support staff. We declare that there are no personal conflicts of interest and institutional or individual financing other than what has been covered by the authors.
References
- (2012) FIGO Safe Motherhood and Newborn Health (SMNH) Committee Management of the second stage of labor. Int J Gynecol Obstet 119: 111-116.
- Savas M Menticoglou M, Frank Manning M, Christopher Harman M, Ian Morrison M (1995) Perinatal outcome in relation to second-stage duration. Am J Obstet Gynecol 173(3): 906-912.
- Hunt M, Menticoglou M (2015) Perinatal Outcome in 1515 Cases of Prolonged SSOL in Nulliparous Women. J Obstet Gynaecol Can 37(6): 508-516.
- Jos B Delee M (1920) The prophylactic forceps operation. Am J obstet Gynecol 1: 34-44.
- (2014) NICE Intrapartum care for healthy women and babies pp. 190.
- Friedman EA (1954) The graphic analysis of labor. Am J Obstet Gynecol 68: 691-703.
- Friedman EA (1955) Primigravid labor: A graphicostatistical analysis. Obstet Gynecol 6: 567-589.
- (1996) WHO Care in normal birth: a practical guide. World Health Organization. Department of Reproductive Health and Research 96(24): 1-58.
- Joy E, Lawn SC, Jelka Zupan (2005) 4 million neonatal deaths: When? Where? Why? Lancet 365: 891-900.
- Sandström A, Altman M, Cnattingius S, Johansson S, Ahlberg MM, Stephansson O, et al. (2017) Durations of second stage of labour and pushing, and adverse neonatal outcomes: A population-based cohort study. J. Perinatol 37: 236-242.
- Altman MR, Lydon Rochelle MT (2006) Prolonged second stage of labour and risk of adverse maternal and perinatal outcomes: A systematic review. Birth 33: 315-322.
- Saunders NS, Paterson CM, Wadsworth J (1992) Neonatal and maternal morbidity in relation to the length of the second stage of labour. Br J Obstet Gynaecol 99(5): 381-385.
- Yueh Chang Kuo C PC, Kuo Gon Wang (1996) Factors Influencing the Prolonged Second Stage and the Effects on Perinatal and Maternal Outcomes. J Obstet Gynaecol 22(3): 253-257.
- Abalos E, Oladapo OT, Chamillard M, Díaz V, Pasquale J, et al. (2018) Duration of spontaneous labour in ‘low-risk’ women with ‘normal’ perinatal outcomes: A systematic review. European Journal of Obstetrics & Gynecology and Reproductive Biology 223: 123-132.
- Le Ray CC, Audibert FF, Goffinet FF, Fraser W (2009) When to stop pushing: Effects of duration of second-stage expulsion efforts on maternal and neonatal outcomes in nulliparous women with epidural analgesia. Am J Obstet Gynecol pp. 201.
- Myles TD, Santolaya J (2003) Maternal and neonatal outcomes in patients with a prolonged second stage of labour. Obstet Gynecol 102(1): 52-58.
- Thomas T, Joaquin S (2003) Maternal and neonatal outcomes in patients with a prolonged second stage of labor. Obstetics & Gynecol 102(1): 52-58.
- Naime Alix AF, Fourquet, Sigue D, Potin J, Descriaud C, et al. (2008) [How long can we wait at full dilatation. A study of maternal and neonatal morbidity related to the duration of the second stage of labour in nulliparous women]. J. Gynecol. Obstet. Biol. Reprod 37: 268-275.
- Nuria Infant Torres, Milagros Molina Alarcón, Juan Gómez Salgado, Julián RodríguezAlmagro, Ana Rubio Álvarez, et al. (2019) Relationship between the duration of the second stage of labour and neonatyal morbidity. J Clin Med 8(3): 376.
- Bleich ATT, Alexander JMM, McIntire DDD, Leveno KJ (2012) An analysis of second-stage labour beyond 3 h in nulliparous women. Am J Perinatol 29: 717-722.
- Gimovsky AC, Berghella V (2016) Randomized controlled trial of prolonged second stage: Extending the time limit vs usual guidelines. Am J Obstet Gynecol 214(3).
- Cheng YW, Hopkins LM, Laros RK, Caughey AB, (2007) Duration of the second stage of labour in multiparous women: Maternal and neonatal outcomes. Am J Obstet Gynecol 196(6): 585.e1-585.e6.
- Cheng YW, Shaffer BL, Nicholson JM, Caughey AB (2014) Second stage of labour and epidural use: A larger effect than previously suggested. Obstet Gynecol 123(3): 527-535.
- Allen VM, Baskett TF, O Connell CM, McKeen D, Allen AC, et al. (2009) Maternal and perinatal outcomes with increasing duration of the second stage of labour. Obstet Gynecol 113(6): 1248-1258.
- Rouse DJ, Weiner SJ, Bloom SL, Varner MW, Spong CY, et al. (2009) Second stage labour duration in nulliparous women: Relationship to maternal and perinatal outcomes. Am J Obstet Gynecol 201(4): 357. e1-357.e7.
- Laughon SK, Berghella V, Reddy UM, Sundaram R, Lu Z, et al. (2014) Neonatal and maternaloutcomes with prolonged second stage of labour. Obstet. Gynecol 124(1): 57-67.
- Grobman WA, Bailit J Lai Y, Reddy UM, Wapner RJ, Varner MW, et al. (2016) Association of the duration of active pushing with obstetric outcomes. Obstet Gynecol Dept 127(4): 667-673.
- Mayanja R, AC, MM, SM, Nkonwae I (2016) Association between Duration of SSOL and Perinatal Outcomes among Mothers admitted in Labour at Mbarara Regional Referral Hospital, Uganda. American Scientific Research Journal for Engineering, Technology, and Sciences (ASRJETS) 25(1): 112-30.
- Wei hong Li, Hong yu Zhang, Yi Ling, Song Jin (2011) Effect of prolonged second stage of labour on maternal and neonatal outcones. Asian Pacific Journal of Tropical Medicine 4(5): 409-411.
- Cheng YW, Hopkins LM, Caughey AB (2004) How long is too long: Does a prolonged second stage of labor in nulliparous women affect maternal and neonatal outcomes? Am J Obstet Gynecol 191(3): 933-938.
- Singh S, Aiyer KU, Vardhan S (2018) Management of prolonged second stage of labor. Int J Reprod Contracept Obstet Gynecol 7(7): 2527-2531.
- (2017) Perinatal Practice Guideline, Clincal Guideline, Delays in the Second Stage of Labour. South Australian Maternal, Neonatal & Gynaecology Community of Practice.
- Grantz KL, Sundaram R, Ma L, Hinkle S, Berghella V, et al. (2018) Reassessing the duration of the second stage of labour in relation to maternal and neonatal morbidity.Obstet Gynecol 131(2): 345.
- Lawn JE, Blencowe H, Waiswa P, Amouzou A, Mathers C, et al. (2016) Stillbirths: rates, risk factors, and acceleration towards 2030. Lancet 387(10018): 587-603.

 Research Article
Research Article