Abstract
The aim of this study was to assess the clinical outcomes and survivorships of cementless Corail small stems to mid-size stems at a mid-term follow-up. A retrospective case-control study included 420 primary hip arthroplasties performed between 2006 and 2010. A case group of small size stems (8 to 10, n=173) were compared to a control group (mid-size stem 11 to 13, n=247). Complications and revisions were recorded. Kaplan- Meier survivorships were measured. Mean follow-up was 6 ± 1.1 years (range, 4-9). The mean PMA score and complication rate at last follow-up were not significantly different between cases and controls. No significative difference was noted between the groups for survivorship free of stem aseptic loosening (p=0.2), free of stem removal for any reason (p=0.09), and free of stem or cup revision for any reason (p=0.3). Small Corail stems were not associated with higher complication or revision rates compared to mid-size stems.
Introduction
Initially developed to be implanted in young patients [1], cementless THA (Total Hip Arthroplasty) are now commonly used, with a proportion that recently surpassed cemented THA in England (39.1% in 2016 [2]) and Australia (63.3% in 2015 [3]). Several series reported excellent long-term survival [4-8], up to 96% at a 23 years follow up with the CorailTM stem (DePuy Synthes, Saint Priest, France) [8]. However, few studies reported the influence of the stem size on the clinical outcomes after THA [9-12]. The British National Joint Register suggested that the revision rate of the Corail stem was higher with small femoral stems (8 to 10) compared to mid-size stems (11 to 13) [12]. The purposes of our study were to assess the clinical outcomes and survivorships of standard small stems (exposed group) to standard mid-size stems (control group) at a mid-term follow-up. We hypothetized that the use of small stems was not associated with a higher risk of revision compared to mid-size stems.
Patients and Methods
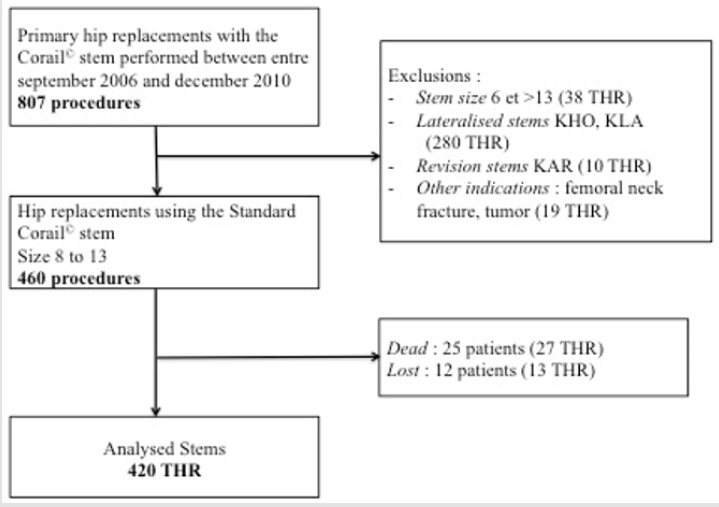
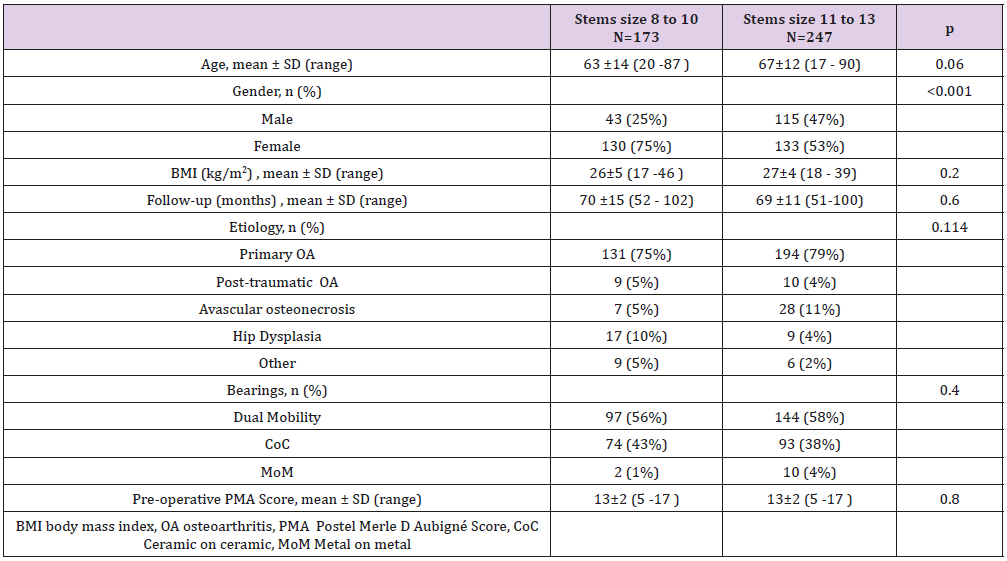
We retrospectively recorded 807 patients who underwent primary THA in our institution between September 2006 and December 2010. During this period, 460 Corail standard stems were implanted in 417 patients. Flow chart of the study is presented in (Figure 1). Exclusions criteria were: revision THAs, lateralised stems and THA for tumor or fracture. Patients were classified based on whether a small (size 8 to 10) or a medium (size 11 to 13) Corail stem was implanted. A total of 420 primary THAs in 380 patients (40 bilateral) were available at a mean follow-up of 6 ± 1.1 years (range, 4-9), including 173 small stems (cases) vs. 247 mid-size stems (controls). Demographics data are summarized in (Table 1) (Figure 1). The stem used was a straight implant made of forged titanium alloy (TiAl6V4), entirely coated with hydroxyapatite (155±35μm). The standard Corail stem was declined from size 8 to 20. From size 8 to 13, stem length varied from 115 to 155mm, width from 7 to 10mm, and offset from 38 to 41.5mm. Neck length, height and shaft angle were similar for all stems (respectively 38.5mm, 36mm and 135°). The stem was used in a collared version.
Different cementless cups were used: 241 dual-mobility cups (57%) (SunfitTM, Serf, Decines, France), 167 ceramic-on-ceramic bearings (39%) (PinnacleTM, DePuy Synthes, Saint Priest, France), and 12 metal-on-metal cups (ASRTM, DePuy Synthes, Saint Priest, France). Complications and revisions were recorded each year since surgery. Patients were evaluated clinically using PMA score [13].
Surgical Technique
Procedures were all performed through a posterolateral approach by the same senior surgeon. Femoral preparation technique aimed for optimal filling of the trial broaches with good vertical and rotational stability keeping a bed of cancellous bone. A standard rehabilitation protocol was initiated after surgery with full-weight bearing allowed immediately.
Statistical Analysis
SSPS v.19 (IBM) was used for statistical analysis. Qualitative variables were compared with a Mann Whitney or Student t-test. Comparisons between categorical variables were performed using Chi-2 or Fisher’s exact test. Survival curves were calculated according to Kaplan-Meier (KM) method and compared using the log rank test. Statistical significance was set at p≤0.05.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The CPP Sud Est ethical comitee of Hospice Civils de Lyon (HCL) approved this study that complies to the MR004 methodology, registered in CNIL under number 18-130. For this type of study formal consent is not required (retrospective and anonymous study). All data were fully anonymized before their access. The ethics committee did not require an informed consent.
Results
Complications and Revisions
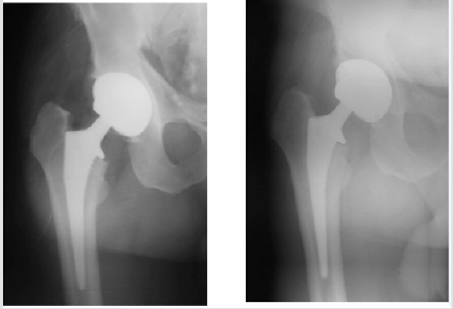
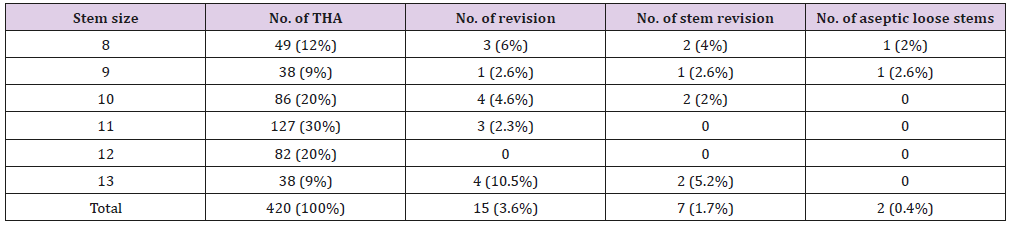
Seven dislocations were identified (six in the patients with a single mobility cup, and one in a dual mobility cup), among which 4 cases needed cup revision. One patient had a fracture of a ceramic liner and one early revision was performed two days after surgery for leg length discrepancy. Seven femoral stems were revised: one case for periprosthetic fracture, 4 cases for infection and 2 cases for aseptic loosening (both in small stems). A 69-year old patient had a stem revision 1.5 year after surgery in a context of femoral Paget’s disease (stem size 8). A malposition and an under sizing of the stem could explain this early failure. After revision with a bigger stem (size 11), the PMA score was 15 points at 6 years. A 56-year old man had a stem revision 5 years after surgery (size 9) (Figure 2A & 2B). During revision, the surgeon reported a mobility of the stem, but no evidence of infection was recorded. The revision rates depending on stem size are detailed in (Table 2).
Figure 2: Radiographs of a 56 years old man who had a stem revision for aseptic loosening. Immediate (Fig 2A) and three years post-operative (Fig 2B) X-rays with development of femoral lines in Gruen’s zones 1, 2, 3 and 6.
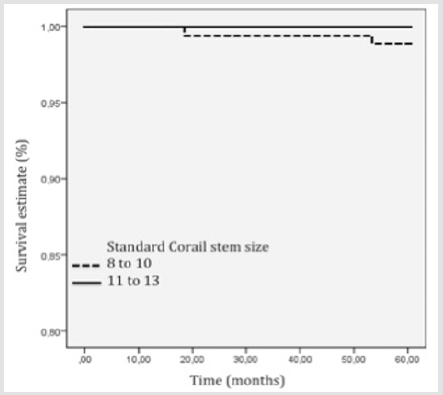
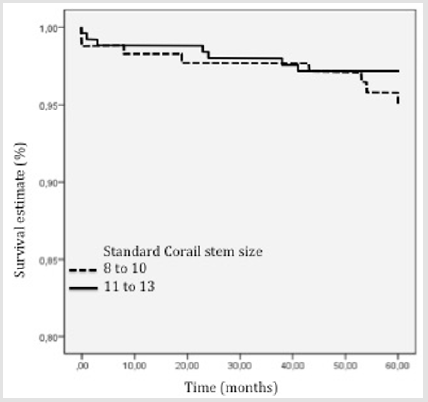
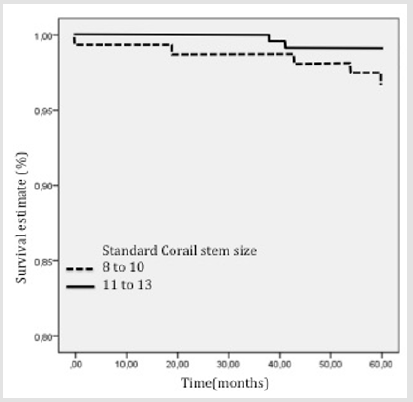
Survivorships
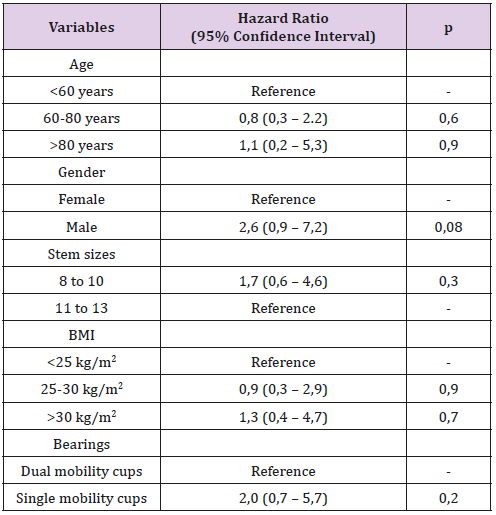
The KM survivorship free of stem aseptic loosening was respectively 99% (95% CI [96.8-100%]) in the small stem group, and 100% in the medium size stem group (p=0.2) (Figure 3). The KM survivorship free of stem revision or stem removal for any reason was 98% (95% CI [96.9-99.5%]) at five years (97% (95% CI [94-99.6%]) in the small size group, and 99% (95% CI [98-100%]) in the mid-size group, p=0.09) (Figure 4). The KM survivorship free of cup or stem revision for any reason was 96% (95% CI [94.2-97.8%]) in the overall cohort at five years (95% (95% CI [91.7-98.4%]) in cases vs. 98% (95% CI [95.1-99.2%]) in controls, p=0.3) (Figure 5). In a univariate analysis, none of the following factors were risk factors for revision: age, gender, stem size, BMI and bearing (Table 3).
Table 3: Univariate analysis of risk factors for stem revision.
(HR : hazard ratio ; CI : confidence interval)
Clinical Outcomes
The mean PMA score at last follow-up was not significantly different between small stems (17±1.6) (range, 7 to 18) and midsize stems (17±1.6)(range, 5 to 18), (p=0.38).
Discussion
Since 1986, Corail stem has been implanted and evaluated many times with excellent results [4-6,8,12,14-17]. This original stem design may be considered as the gold-standard of cementless stems. At 5 and 10 years, survivorships were about 98% in most of the series [4-6,12], and at 23 years up to 96% for Vidalain [8]. Our results are consistent with these previous series, with an overall stem survival of 98% (95% CI [96.9-99.5]) at a five-year follow-up, considering stem removal for any reason. Jameson et al. [12] demonstrated that complication rates were higher for small femoral stems than for mid-size stems (HR=1,8 [99% CI [1.4-2.37]; p<0.001). In this current study, the size of femoral stems did not influence complication rates (HR=1.7 (95% CI [0.6-4.6]; p=0.33) and clinical outcomes and survivorships were similar between both groups. Clinical evaluation using PMA score, mostly based on pain and walking, did not show significant differences between small and mid-size stems (p=0.4). PMA scores were good or excellent in >90% of the patients in both groups. These results are consistent with the study by Engh et al. [11] who did not find any relation between stem size and satisfaction (p=0.24), pain (0.17), or function (p=0.4). Only standard Corail stems were included as lateralised stems previously demonstrated a higher risk of loosening [18,19].
Demey et al. [20] showed that the use of a collared Corail stem increased the horizontal and vertical stability. In our series, we only implanted collared stems, while most of stems were collarless for Jameson et al [12]. Two cases of stem aseptic loosening were recorded in our study (13% of the causes for revision). This was consistent with the results of Jameson et al [12] with a revision rate of 16.5% for stem aseptic loosening. At 15-year, Engh et al. [11] calculated the overall survivorship of the stem was 98%. Survivorship was not significantly different among the different stem sizes (p=0.4). Vresilovic et al. [9] reported the survivorship of 296 femoral stems at 2-year follow-up and did not find any significant difference according to stem size. Our study had several limitations. First, we did not perform radiological analysis, as it was not the purpose of this study but to focus on survivorship. Second, the study was retrospectively performed. The strengths were its homogeneity, as the same senior surgeon performed all procedures and the mid-term follow-up.
The influence of stem size on revision rate is controversial. In the current study, small size stems (8 to 10) were not associated with higher revision rates compared to mid-size stems (11 to 13). Further studies including a larger sample size, at a longer followup, with radiological analysis must be performed in the future.
References
- Charnley J, Cupic Z (1973) The nine and ten year results of the low-friction arthroplasty of the hip. Clin Orthop Relat Res (95): 9-25.
- (2016) NAL. National Joint Registry for England and Wales: 13th annual report.
- (2016) Australian Ortopaedic Association National Joint Replacement Registry. Annual Report.
- Vidalain JP (1997) HA coating. Ten-year experience with the CORAIL system in primary THA. The Artro Group. Acta Orthop Belg 63(1): 93-95.
- Froimson MI, Garino J, Machenaud A, Vidalain JP (2007) Minimum 10-year results of a tapered, titanium, hydroxyapatite-coated hip stem: an independent review. J Arthroplasty 22(1): 1-7.
- Hallan G, Lie SA, Furnes O, Engesaeter LB, Vollset SE, et al. (2007) Medium- and long-term performance of 11,516 uncemented primary femoral stems from the Norwegian arthroplasty register. J Bone Joint Surg Br 89(12): 1574-1580.
- Drobniewski M, Borowski A, Synder M, Sibiński M (2013) Results of total cementless hip joint arthroplasty with Corail stem. Ortop Traumatol Rehabil 15(1): 61-68.
- Vidalain JP (2011) Twenty-year results of the cementless Corail stem. Int Orthop 35(2): 189-194.
- Vresilovic EJ, Hozack WJ, Rothman RH (1996) Incidence of thigh pain after uncemented total hip arthroplasty as a function of femoral stem size. J Arthroplasty 11(3): 304-311.
- Sköldenberg OG, Bodén HSG, Salemyr MOF, Ahl TE, Adolphson PY (2009) Periprosthetic proximal bone loss after uncemented hip arthroplasty is related to stem size: DXA measurements in 138 patients followed for 2–7 years. Acta Orthop 77(3): 386-392.
- Engh CA, Mohan V, Nagowski JP, Sychterz Terefenko CJ, Engh CA (2009) Influence of stem size on clinical outcome of primary total hip arthroplasty with cementless extensively porous-coated femoral components. J Arthroplasty 24(4): 554-559.
- Jameson SS, Baker PN, Mason J, Rymaszewska M, Gregg PJ, et al. (2013) Independent predictors of failure up to 7.5 years after 35 386 single-brand cementless total hip replacements: a retrospective cohort study using National Joint Registry data. J Bone Joint Surg Br 95(6): 747-757.
- Merle D Aubigné R (1990) Numerical classification of the function of the hip. 1970. Rev Chir Orthop 76(6): 371-374.
- Røkkum M, Brandt M, Bye K, Hetland KR, Waage S, et al. (1999) Polyethylene wear, osteolysis and acetabular loosening with an HA-coated hip prosthesis. A follow-up of 94 consecutive arthroplasties. J Bone Joint Surg Br 81(4): 582-589.
- Chatelet JC, Setiey L (2004) Comportement osseux à long terme après implantation dun pivot fémoral totalement revêtu d hydroxyapatite: Une série continue de 120 arthroplasties totales primaires à 12 ans de recul. Rev Chir Orthop 90(7): 628-635.
- Boldt JG, Cartillier JC, Machenaud A, Vidalain JP (2015) Long-term Bone Remodeling in HA-coated Stems: A Radiographic Review of 208 Total Hip Arthroplasties (THAs) with 15 to 20 Years Follow-up. Surg Technol Int 27: 279-286.
- Merini A, Viste A, Desmarchelier R, Fessy MH (2016) Cementless Corail™ femoral stems with laser neck etching: Long-term survival, rupture rate and risk factors in 295 stems. Orthop Traumatol Surg Res 102(1): 71-76.
- Cantin O, Viste A, Desmarchelier R, Besse JL, Fessy MH (2015) Compared fixation and survival of 280 lateralised vs 527 standard cementless stems after two years (1-7). Orthop Traumatol Surg Res 101(7): 775-780.
- Courtin C, Viste A, Subtil F, Cantin O, Desmarchelier R, et al. (2017) Cementless lateralized stems in primary THA: Mid-term survival and risk factors for failure in 172 stems. Orthop Traumatol Surg Res 103(1): 15-19.
- Demey G, Fary C, Lustig S, Neyret P, Si Selmi TA (2011) Does a collar improve the immediate stability of uncemented femoral hip stems in total hip arthroplasty? A bilateral comparative cadaver study. J Arthroplasty 26(8): 1549-1555.

 Research Article
Research Article