Abstract
Patients with CHF and COPD were examined during physical activity with dynamic monitoring of CO2. Parameters of dyspnea are compared with CO2 values before, during and after 6MWT. When performing physical activity revealed signs of periodic breathing, which has a prognostic value.
Introduction
Dyspnea is the most important symptom of patients with Chronic Heart Failure (CHF) and patients with Chronic Obstructive Pulmonary Disease (COPD). The nature of this dyspnea, despite tremendous advances in the fields of cardiology and pulmonology, is not well known [1,2]. Difficulties arise probably when trying to objectify the patient’s subjective feelings. This is partly due to the lack of a unified interpretation of the concept of dyspnea. Necessary measures in the diagnosis are methods of instrumental objectivization [3,4]. Along with the generally accepted methods of examination, various functional diagnostic methods are used to determine functional impairment, in which the parameters of gas exchange are often examined [5]. The value of end-tidal CO2 (PETCO2) is a constant that indicates the activity of the respiratory system [6]. Dyspnea is combined with changes in pulmonary ventilation and CO2 gas exchange [7,8]. Dyspnea is one of the most frequent reasons why patients stopped during the 6-Minute Walk Test (6MWT). Exercise tests are used to determine exercise tolerance in patients with CHF and COPD [9].
Purpose
To explore the features of changes PETCO2 during execution 6MWT in patients with CHF and COPD.
Methods
We studied 52 patients with CHF in New York Heart Association (NYHA), age 58±3,24 years (25 patients (48,1%) in NYHA class II, 22 patients (4,3%) in NYHA class III, 5 patients (9,6%) in NYHA class IV). Also, we studied 42 patients with COPD II-III, age 60 ± 3,48 years (1st group - 22 patients (52,4%) with COPD II, 2nd group-20 patients (47,6%) with COPD III). Control group 30 patients, age 48±3,42 years. Standard 6MWT was performed. Dyspnea was evaluated on a scale of Borg, MRS and VAS. We recorded nanogram before, during, after the 6MWT and in the recovery period using a capnograph Life Sense.
Results
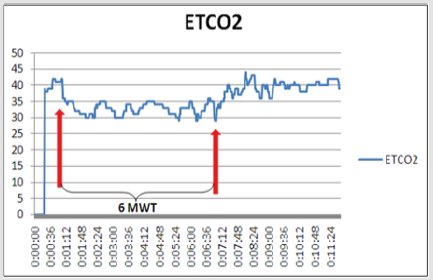
Significance of PETCO2 in patients with CHF in NYHA class II was 38,2±2,13mm Hg, in patients in NYHA class III was 34,4±2,22mm Hg, in patients in NYHA class IV was 32,4±1,14mm Hg. Significance of PETCO2 in 1st group patients with COPD was 36,2±2,43mm Hg, in 2nd group patients was 34,1±1,22mm Hg. All patients performed 6MWT. The 6MWT distance in patients with CHF in NYHA class II was 384±10,56m, in NYHA class III was 290±17,24m, in NYHA class IV was 142±3,51m. The 6MWT distance in 1st group patients with COPD was 440±15,48m, in 2nd group was 384±15,42m. There is reduction PETCO2 in all patients with CHF during the 6MWT. PETCO2 in patients with CHF in NYHA class II was 33,34±2,51mm Hg, in NYHA class III was 31,75±2,89mm Hg, in NYHA class IV was 28,8±1,32mm Hg. 69,2% patients reported dyspnea as the main reason for a stop during the 6MWT. There is increase PETCO2 in all patients with COPD during the 6MWT. After the 6MWT the significance of PETCO2 in 1st group was 43,21±2,81mm Hg, in 2nd group was 45,05±3,26 mm Hg. All patients reported dyspnea as the main reason for a stop during the execution 6MWT. When we analyzed the trend of PETCO2 we found that these patients showed signs of periodic breathing (Figure 1) than control group.
Conclusion
Thus, capnography increases the diagnostic value of the 6MWT, helps to make interpretation of dyspnea in patients with CHF and COPD.
References
- Garcia Aymerich J, Serra I, Gómez FP, Farrero E, Balcells E, et al. (2009) Physical activity and clinical and functional status in COPD. Chest 136(1): 62-70.
- Garcia Rio F, Lores V, Mediano O, Rojo B, Hernanz A, et al. (2009) Daily physical activity in patients with chronic obstructive pulmonary disease is mainly associated with dynamic hyperinflation. Am J Respir Crit Care Med 180(6): 506-512.
- Pitta F, Takaki MY, Oliveira NH, Santanna TJ, Fontana AD, et al. (2008) Relationship between pulmonary function and physical activity in daily life in patients with COPD. Respir Med 102(8): 1203-1207.
- Eliason G, Zakrisson AB, Piehl Aulin K, Hurtig Wennlöf A (2011) Physical activity patterns in patients in different stages of chronic obstructive pulmonary disease. COPD 8(5): 369-374.
- Francis DP, Shamim W, Davies LC, Piepoli MF, Ponikowski P, et al. (2000) Cardiopulmonary exercise testing for prognosis in chronic heart failure: Continuous and independent prognostic value from VE/VCO(2) slope and peak VO(2). Eur Heart J 21(2): 154-161.
- LL SHika, NN Kanaeva (1980) General issues of research methods and criteria for assessing respiratory rates. Medicine 21-36.
- Csorba Z, Petak F, Nevery K, Tolnai J, Balogh AL, Rarosi F, et al. (2016) Capnographic parameters in ventilated patients: Correspondence with airway and lung tissue mechanics. Anesthesia and Analgesia 122(5): 1412-1420.
- P Messner Pellenc, C Brasileiro, S Ahmaidi, J Mercier, C Ximenes, et al. (1995) Exercise intolerance in patients with chronic heart failure: Role of pulmonary diffusing limitation. Eur Heart J 16(2): 201-209.
- Belza B, Steele BG, Hunziker J, Lakshminaryan S, Holt L, et al. (2001) Correlates of physical activity in chronic obstructive pulmonary disease. Nurs Res 50(4): 195-202.

 Short Communication
Short Communication