Abstract
In recent years chemotherapy and hematopoietic stem cell transplantation are commonly used for the treatment of leukemia disease. In case of chemotherapy, anticancer drugs cause symptoms i.e., mucosal desorder, vomitus, diarrhea, alopecia, and skin disorder. Chemotherapy and hematopoietic stem cell transplant is effective for these treatment. However, for the patients it is a great burden physically and mentally. Therefore, a new therapy method is required; methods that can induce apoptosis only in leukemia cells and suppress the side effect. In this study, we focus on the characteristic of the ultraviolet light range UVA1 to investigate the possibility of cellular apoptosis induction in leukemia T cells. The UV-LED with the wavelength of 389nm was applied in human T cell leukemia (Jurkat T cell) to evaluate the apoptosis and necrosis percentage induction. The Jurkat T cells were irradiated with 0, 10, 20, 30J/cm2 irradiation dose, respectively. As the result, the percentage of apoptosis increased proportionally according to the irradiation dose value. 57 % of apoptosis was obtained at 30J/cm2 irradiation dose. Importantly, the percentage of necrosis was generated only 0.2%. This result indicate the possibility of cellular apoptosis induction without completely destroy a cell that could cause in side effect in the end. This treatment could lead us to a new treatment item such as a micro device by using UV-LED for implant in the bone marrow.
Introduction
In recent years, the mortality rate of leukemia patients has been increasing worldwide. According to the National Cancer Center in Japan, the actual measured number of deaths in 2016 was 4,900 male and 3,300 females [1]. Leukemia is a blood cancer. In the blood cells, there are erythrocytes, platelets and leukocytes. However, these blood cells become cancer during the process of formation in the bone marrow. The cancerous cells (leukemic cells) proliferate in the bone marrow and can be occupy. Therefore, the normal blood cells decrease and the following symptoms such as anemia, immune-compromised, bleeding tendency, and enlargement of the spleen appeared [2-4]. Leukemia is divided into myelocytic and lymphatic from the type of cancerous cells, moreover it is divided from the progressive pattern and symptoms into acute and chronic. In acute leukemia there are an acute myeloid leukemia (AML) and acute lymphoblastic leukemia (ALL) [5,6].
On the other hand, in chronic leukemia there are chronic myelogenous leukemia (CML) and chronic lymphocytic leukemia (CLL) [7,8]. For the treatment of leukemia, chemotherapy and hematopoietic stem cell transplantation are commonly used [9,10]. In case of chemotherapy, mucosal disorder, vomitus, diarrhea, alopecia, skin disorder and others side effect are caused by the anticancer drugs [11]. On the other hand, it is necessary to wait for a donor from relative or unrelated person to do hematopoietic stem cell transplantation. In hematopoietic stem cell transplantation, after the treatment of anticancer drugs or radiation, stem cells are administered into the body. However, similar side effects and complicating disorder are observed in chemotherapy. In contrast, many patients for the hematopoietic stem cell transplantation have specific complication such as Graft Versus Host Disease (GVHD), which not occurred in the chemotherapy [12]. Therefore, different methods of treatment to reduce a side effect in order to diminish the suffering of the patient are needed. In this study, we focus in the characteristic and potential of ultraviolet light. It is known that the ultraviolet light are able cutoff the DNA cell [13]. If by applying the ultraviolet light in micro-device to implant into the bone narrow, it might have the possibility for directly cure without using anticancer drug. For the development of an implant photonics micro-device, it is necessary examine the effective ultraviolet wavelength which could induce cellular apoptosis with lower necrosis to avoid internal infection.
Development of UV-LED Irradiation System
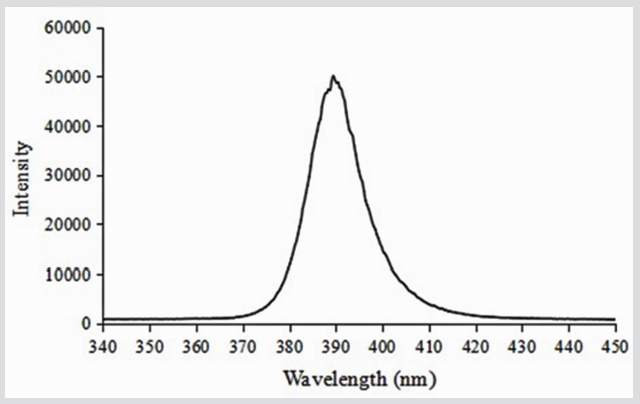
In this study, to evaluated the induction of cellular apoptosis and necrosis using ultraviolet light, we developed an irradiation system applying commercially ultraviolet light emitting diode (UVLED) with the peak wavelength 389nm and FWHM 13.4nm (LZ1- 10UA00-U4, LED Engin, Inc,) as shown in (Figure 1). This UV-LED is classified in UVA1 (340 - 400nm) field. The irradiation system is composed for 10 pieces without optical lens and reflective plate.
Methods
It is necessary to understand the characteristics of the UV-LED irradiation system in order to evaluate the effect of ultraviolet light to cancer cells. Therefore, irradiation intensity, irradiation uniformity and the temperature characteristics of medium used in this experiment were evaluated first.
Evaluation of Irradiation Intensity
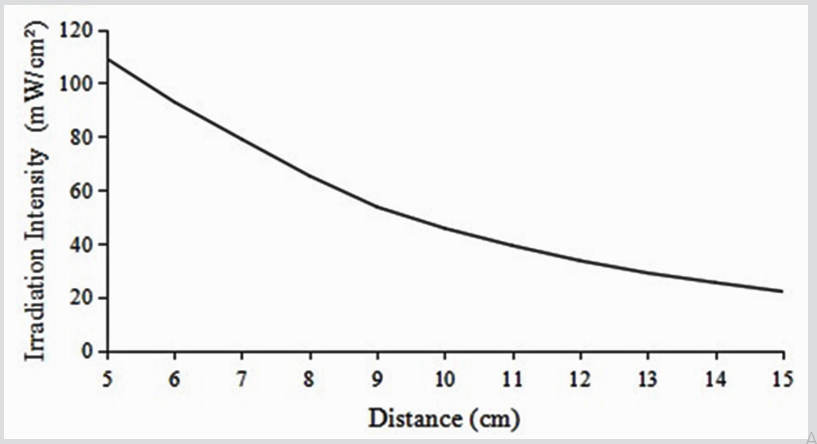
To evaluate the characteristic of the UV-LED irradiation system, the irradiation intensity of light source was measured. The light source was fixed above the center of power-meter (PM100USB, S310C, Thorlabs, Inc). The height of the light source was varied from 5cm to 15cm and the mean irradiation intensity was measured at 1cm intervals.
Evaluation of Irradiation Uniformity
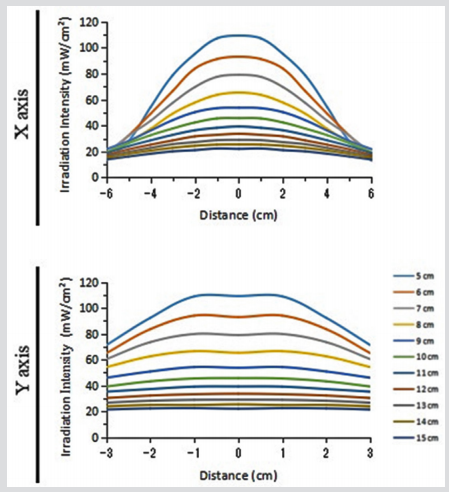
To evaluate the irradiation uniformity, the light source was fixed above the center of the power-meter, and the power-meter was moved at intervals of 1cm while in the X axis direction and the Y axis direction from the center of the light source, and the irradiation intensity was measured in each place. The height of the light source was varied from 5cm to 15cm at 1cm intervals.
Evaluation of Temperature Characteristics of Mediums
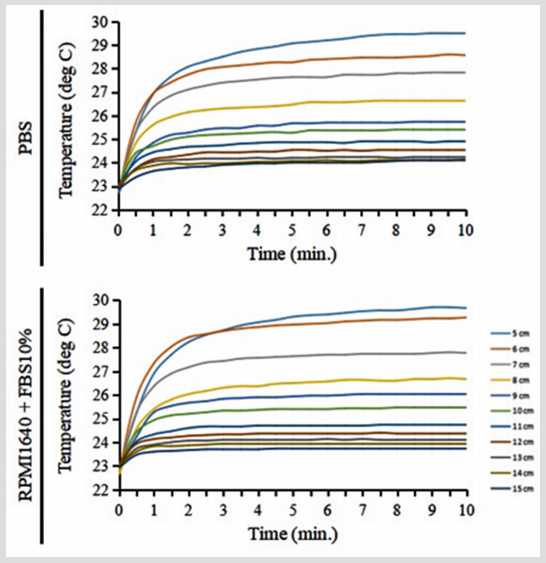
Two types of mediums: RPMI1640 (phenol red) Medium With L-glutamine and sodium bircarbonate (R8758-599ML, SIGMAALDRICH Co.,)/ Fetal Bovine Serum (FBS) 10% (S1820-500, Biowest SAS) and Phosphate Buffered Saline (PBS) medium (Wako Pure Chemical Industries, Ltd.) was irradiate with the 389nm peak wavelength to analyze the temperature characteristics of the mediums. 3mL of each medium were placed into φ6cm petri dish and a thermoelectric couple (TT-533, TANITA Corp.) was fixed in the center of petri dish. The light source was fixed above the center of the petri dish and the height was varied from 5cm to 15cm at 1cm intervals. On each height, at 10 minutes for 30 second interval the temperature was measured.
Irradiation Experiment
To evaluate the effect of peak wavelength 389 nm on the leukemia cell, the Jurkat T cells (human T cell leukemia, RCB 3052, RIKEN National Bio-Resource Center, Japan.) were cultured with RPMI1640 (phenol red)/ FBS 10% medium in 5% CO2 at 37 deg C, 48 hours. More than 85% live cells was used in the irradiation experiment. The Jurkat T cells were diluted to 0.5 × 106 cells/mL with PBS medium. In each nine dish, the irradiation dose of 0 J/cm2 (control), 10J/cm2 , 20 J/cm2 , and 30J/cm2 were applied. The light source was set at a height of 12cm and the irradiation intensity was 50 mW/cm2 . After the irradiation, the cells was cultured for 24 hours in 5% CO2 at 37 deg C using RPMI1640 (phenol red)/ FBS 10% medium. The cells were collected to examine cellular apoptosis and necrosis using a flow cytometer (BD FACS Aria II Cell Sorter, Becton Dickinson Co., Ltd.,), stained with annexin-V fluorescein isothiocyanate and propidium iodide (Medical & Biological Laboratories Co., Ltd.,).
Results
Evaluation of UV-LED Irradiation System
Irradiation intensity, irradiation uniformity and medium temperature characteristic using light source were evaluated in order to understand the characteristic of UV-LED irradiation system. Figure 2 shows the result of the irradiation intensity. The irradiation intensity is proportional to the irradiation distance. At 5cm more than 100mW/cm2 were obtain, however at 15cm irradiation distance, the irradiation intensity decreased to 25 mW/ cm2 . This is for, that in the light source there not use optical lens or reflective plate. On the other hand, (Figure 3) described the result of the irradiation uniformity measurement; from the irradiation distance of 5cm to 11 cm, the uniformity of X and Y axis direction are obtained concentrate irradiation intensity in the center, and from the irradiation distance 12cm to 15cm, uniform irradiation intensity was also obtained. (Figure 4) described the result of mediums temperature measurement. In comparison of the both mediums, RPMI1640 (phenol red)/ FBS10% medium was showing approximately 0.5 deg C higher in each condition than that of PBS medium. It seems that the medium temperature is increased by the light absorption occurred in phenol red. According to these results, PBS medium was chooses to be used in the irradiation experiment to examine the effect of ultraviolet light in the leukemia T cell. The irradiation distance was chosen at 12cm because the temperature is almost similar with the room temperature and the irradiation intensity is uniform.
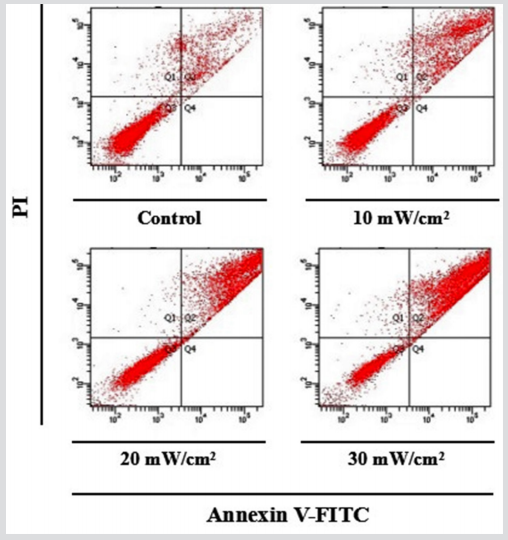
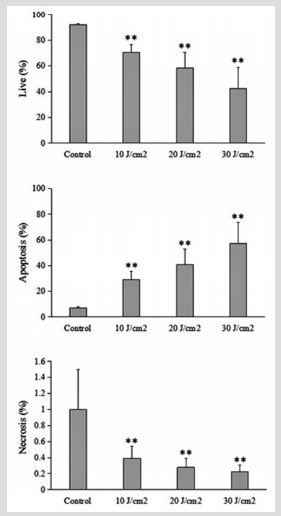
Effects of Irradiation to the Cell
Figures 5a & b shows the result of the irradiation experiment using peak wavelength 389 nm on the Jurkat T cells. Figure 5a is the flow cytometry dot plots, with each dot described the condition of cell. The area Q1 define necrosis, Q2 define apoptosis and Q3 define live cells. It is understandable that in comparison of control with 10, 20 and 30 J/cm2 , the live cells were changed to apoptosis. Figure 5b is the graph made with the values acquired by flow cytometry dot plots. The apoptosis induction was increased significantly when the irradiation dose increased. The is a significant difference observed between the test plots and all the treatment; 29% of apoptosis was acquired at 10J/cm2 irradiation dose, 41% at 20J/cm2 , and at 30J/ cm2 irradiation dose, 57% apoptosis was acquired. On the other hand, no great difference on each irradiation dose in the induction of cellular necrosis was observed; in average it was 0.3% acquired. However compare to control, the rate of necrosis was observed decreased according to doses of the treatment. Moreover, the higher the doses of the treatment, the less necrosis rate was observed. These results indicated that the peak wavelength 389nm is effective to induce specifically cellular apoptosis without inducing cellular necrosis, that might causes infection into the body.
Discussion
In this study, we develop an irradiation system using peak wavelength 389nm UV-LED to examine the cellular apoptosis induction on human T cell leukemia (Jurkat T cells). The irradiation experiment was done in condition of uniform irradiation at the room temperature without causing the medium temperature increased for examination the effect of ultraviolet light only in the cells. Irradiation dose of 10, 20 and 30J/cm2 was applied and in comparison, with control i.e, non-irradiated dose: the apoptosis induction was increased in accordance to the irradiation dose. On 30J/cm2 irradiation dose, 57% of apoptosis induction was acquired. Interestingly, the proportion of necrosis was only 0.3%. This result indicated the possibility of safety treatment in leukemia cells as the target. The induction of T cell apoptosis is mediated through activation of the FAS/FAS-ligand system in irradiated cells as a consequence of singlet oxygen generation. The generation of singlet oxygen is considered to have a central role in inducing apoptosis and is an underlying mechanism of UVA1 phototherapy [14]. The findings of the present study demonstrated that the peak wavelength 389nm of UV-LED is effective to treat leukemia disease and show the possibility to develop an implant device.
Conclusion
In this study, we examined the cellular apoptosis in the human T cell leukemia (Jurkat T cells) using UV-LED with the peak wavelength of 389nm. 57% of apoptosis was acquired with 30J/cm2 of irradiation dose. It was found that induction of apoptosis depends on irradiation dose, and the proportion of necrosis induction is practically naught. These results clarified several factors required for the development of implant devices for leukemia diseases treatment.
Acknowledgement
This work was done in part at Gene Research Center, Hirosaki University.
References
- (2016) Cancer Statistics in Japan, Center for Cancer Control and Information Services. National Cancer Center,
- JL Steegmann, M Baccarani, M Breccia, LF Casado, V García Gutiérrez, et al. (2016) European LeukemiaNet recommendations for the management and avoidance of adverse events of treatment in chronic myeloid leukaemia. Leukemia 30: 1648-1671.
- K Kojima, J Ishizawa, M Andreeff (2016) Pharmacological activation of wild-type p53 in the therapy of leukemia. Exp Hematol 44(9): 791-798.
- G Tamamyan, T Kadia, F Ravandi, G Borthakur, J Cortes, et al. (2017) Frontline treatment of acute myeloid leukemia in adults. Crit Rev Oncol Hematol 110: 20-34.
- SK Tasian, SP Hunger (2017) Genomic Characterization of Paediatric Acute LymphoblasticLeukaemia: An Opportunity for Precision Medicine Therapeutics. Br J Haematol 176(6): 867-882.
- EJ Jabbour, JE Cortes, HM Kantarjian (2013) Resistance to Tyrosine Kinase Inhibition Therapy for Chronic Myelogenous Leukemia: A Clinical Perspective and Emerging Treatment Options. Clin Lymphoma Myeloma Leuk 13(5): 515-529.
- TJ Kipps, FK Stevenson, CJ Wu, CM Croce, G Packham, et al. (2017) Chronic lymphocytic leukaemia. Nat Rev Dis Primers 3: 16096.
- B Chen, JB Lee, H Kang, MD Minden, L Zhang, et al. (2018) Targeting chemotherapy-resistant leukemia by combining DNT cellular therapy with conventional chemotherapy. J of Experimental & Clinical Cancer Research 37: 88.
- AM Dickinson, J Norden, S Li, I Hromadnikova, C Schmid, et al. (2017) Graft-versus-Leukemia effect Following Hematopoietic Stem Cell Transplantation for Leukemia. Front Immunol 8: 496.
- J Sun, Q Wei, Y Zhou, J Wang, Q Liu, et al. (2017) A systematic analysis of FDA-approved anticancer drugs. BMC Syst Biol 11: 87.
- MK Juric, M Shevtsov, P Mozes, J Ogonek, RE Crossland, et al. (2017) B-Cell-Based and Soluble Biomarkers in Body Liquids for Predicting Acute/Chronic Graft-versus-Host Disease after Allogeneic Hematopoietic Stem Cell Transplantation. Front Immunol 7: 660.
- Ahmad Besaratinia, J Yoon, C Schroeder, SE Bradforth, M Cockburn, et al. (2011) Wavelength dependence of ultraviolet radiation-induced DNA damage as determined by laser irradiation suggests that cyclobutane pyrimidine dimers are the principal DNA lesions produced by terrestrial sunlight. FASEB J 25(9): 3079-3091.
- Kato Y, Sasagawa I, Kaneko M, Osawa M, Fujita N, et al. (2004) Aggrus: a diagnostic marker that distinguishes seminoma from embryonal carcinoma in testicular germ cell tumors. Oncogene 23(52): 8552-8556.
- Morita A, Werfel T, Stege H, Ahrens C, Karmann K, et al. (1997) Evidence that singlet oxygeninduced human T helper cell apoptosis is the basic mechanism of ultraviolet-A radiation phototherapy. J Exp Med 186: 1763-1768.

 Research Article
Research Article