Opinion
In this paper we reflect on 15 years of experience of working on eHealth research and evaluation in the UK.
An integrated, interroperable eHealth programme has yet to materialise. The initial promise that eHealth interventions can facilitate the shaping of the 21st century healthcare systems Stead et al. [1], has not been empirically demonstrated in the past decade. Although isolated cases of successful initiatives exist, the potential of eHealth remains largely unrealised Muuraiskangas et al. [2-4]. Investment in large programmes which aim to develop an integrated and interoperable platform across settings and levels of care, such as the NPfIT in the UK, may not have provided good value for money. Worse still, patient’s safety may have also been compromised Han et al. [5]. Similarly, to eCommerce, eGovernment and eLearning, eHealth (Table 1) was the result of both a demand by consumers and an initiative by government. It was therefore initially considered a paradox that it failed to deliver the muchanticipated benefits. A closer study of the various implementation programmes reveals the reasons for the relative failure of the UK to have a homogeneous and interoperable eHealth platform. These are summarised below:
a) Delays and frustrations due to a number of top-down, centrally driven policies.
b) Lack of full appreciation of the “ecosystem” of healthcare, which consists of at least five highly interrelated and reactive to change factors: medical, technical, organisational, psychosocial and political.
c) Implementation of stand-alone, not fit-for-purpose systems.
d) An urgency with which eHealth initiatives have been commissioned, developed and deployed, typically at considerable expense.
e) Lack of eHealth-specific protocols for best practice, for example, lack of training for conducting remote consultations via telemedicine Pappas et al. [6-8].
Despite the widespread frustrations, there is currently a renewed interest to invest in new initiatives. As early as in 2012, the European Commission and the U.S. government signed a Memorandum of Understanding to promote a common approach for the interoperability of eHealth systems and education programmes for information technology and health professionals. This initiative remains unrealised too in terms of outcomes too. It is now clearer than ever that if eHealth was to succeed, a strategic, implementation, and evaluation framework would need to be established. Because eHealth introduces a number of interruptive processes and changes in already complex health care systems, the development of a comprehensive agenda for research, evaluation and sustainability is essential. In doing so, three individual but reasonably integrated steps are crucial: It is possible that eHealth sustainability requires synergic action between the private and the public sector. Such partnership models may enhance planning beyond the technology level and facilitate systems and problemsolving thinking for the sustainable and integrated use of eHealth.
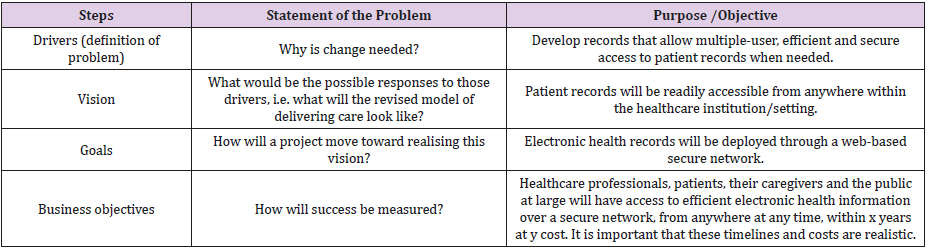
A comprehensive model of this kind, originally proposed by Beauchamp [9] as a generic business plan, was adapted by Catwell et al. (2009) for the purposes of examining how eHealth could be made more sustainable, focusing on the problems of patients, families and clinicians rather than on the technical problems alone. The model proposes a way to facilitate change management and sustainable use for future eHealth initiatives. The central element of the plan is the statement of a problem (e.g. why is change from paper-based to electronic medical records needed?) that needs a solution, and subsequent facilitation steps that form a ‘chain of reasoning’ that lead to how eHealth can provide the solution Catwell et al. (2009). In Table 2, we have mapped out the seven steps using the example of shifting from paper-based records to records available to all parties electronically. This example illustrates the potential of eHealth to benefit patients, clinicians and health services, but also the risks associated with privacy and confidentiality and the challenge of installing new systems that cross institutional borders.
The above model should consider needs at practice level and be adjusted so as to facilitate not only effective implementation of sustainable eHealth solutions, such as electronic health records, but also the realisation of targeted health outcomes (such as diabetes management in an endocrinology clinic and cholesterol management in a cardiology clinic). A targeted health outcome is integral in defining the problem, purpose and objective at all stages of the seven-step sustainability plan. Finally, long-term sustainability of eHealth will only materialise, if applications provide substantial maximisation of benefits and minimisation of clinical risk to patients. There is no reason why eHealth is not subjected to the same rigorous evaluation of effectiveness and safety as other clinical and pharmacologic interventions are. Nevertheless, the creation of a solid evidence-base that is intervention-specific is a major challenge, which requires time, effort and resources.
References
- Stead WW, Lin HS (2009) Computational technology for effective health care: immediate steps and strategic directions. National Academy of Sciences.
- Muuraiskangas S, Harjumaa M, Kaipainen K, Ermes M (2016) Process and effects evaluation of a digital mental health intervention targeted at improving occupational well-being: lessons from an intervention study with failed adoption. JMIR Ment Health 3(2): 13.
- Alvarez RC (2002) The promise of e-Health – a Canadian perspective. EHealth International 1(4): 1-6.
- Commission of the European Communities (2004) e-Health - making healthcare better for European citizens: an action plan for a European e-Health area.
- Han YY, Carcillo JA, Ventkataraman ST, Clark RSB, Watson SR, et al. (2005) Unexpected increased mortality after implementation of a commercially sold computerized physician order entry system. Pediatrics 116(6): 1506-1512.
- Pappas Y, Seale C (2009) The opening phase of telemedicine consultations: an analysis of interaction. Social Science and Medicine 68(7): 1229-1237.
- Pappas Y, Vseteckova J, Mastellos N, Greenfield G, Randhawa G (2018) Diagnosis and Decision-Making in Telemedicine. Journal of Patient Experience.
- Pappas Y, Seale C (2010) The physical examination in telecardiology and televascular consultations: a study using conversation analysis. Journal of Patient Education and Counselling 81(1): 113-118.
- Beauchamp G (2007) Business Analysis-Delivering the Right Solution to the Right Problem.

 Opinion
Opinion