Abstract
Background: In this era of ongoing identification and analysis of medical errors, fluid and electrolyte management has trailed behind the medical decisions that have immediate obvious adverse consequences. This predicament may reflect a lack of understanding of the importance of considering individual volume and electrolyte abnormalities as a separate variable that can significantly alter a patient course and outcome.
Objective: This study evaluated the utilization of parenteral preparations, fluids and electrolytes in two tertiary hospitals.
Method: The study was a cross sectional descriptive survey which utilized the folders/medical records of patients’ that visited the hospitals within January 2017 and December 2018. Data was collected using structured observational check list for parenteral utilization, patient care and health facility indicators. Data regarding parenteral utilization was obtained from sampled medical records retrospectively and filled in structured check list accordingly with careful observation. The data was checked and analyzed using the SPSS software (ver. 20.0 for Windows, Inc., Chicago, IL, USA). Descriptive statistics of frequency, percentage, mean and standard deviation was used to summarize the data.
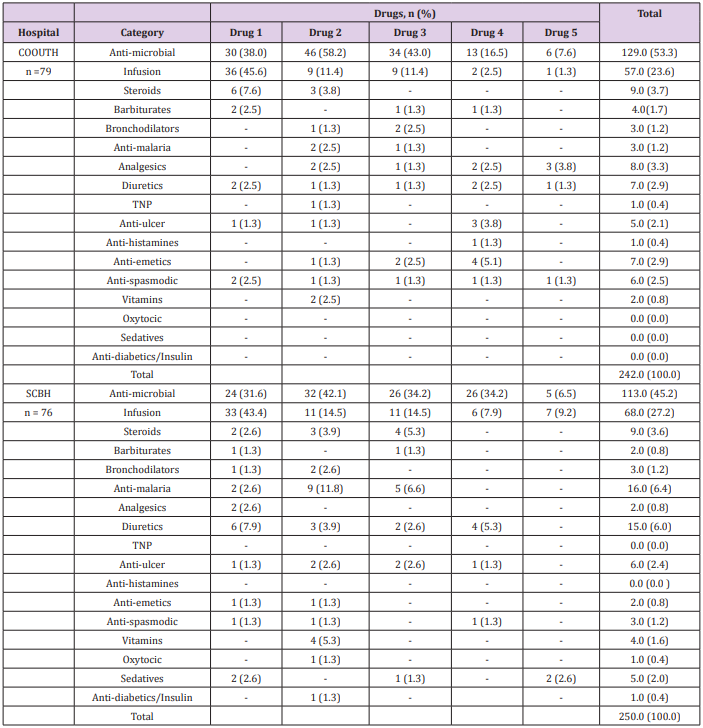
Result: The study revealed that 242 (100.0%) drugs were prescribed to various patients, including anti-microbial drugs 129(53.3%) and infusions 57 (23.6%) appearing as the most commonly prescribed medications which were found in the first two (2) drugs prescribed to patients in Chukwu Emeka Odimegwu Ojukwu University Teaching Hospital (COOUTH). Similarly, at Saint Charles Boromeo Hospital (SCBH), a total of 250 (100%) drugs were prescribed to various patients, including anti-microbial drugs 113( 45.2%), infusions 68 (27.2%) and antimalarial 16 (6.4%) appearing as the most commonly prescribed medications which were found majorly in the first three (3) drugs prescribed to patients. At COOUTH, more generic drugs 214(88.1%) were prescribed than the branded drugs 29(11.9%). Similar trend occurred at SCBH, where higher number of drugs prescribed were generic 171(70) compared to branded prescriptions 74 (30.2). Chi-square test revealed significant association (χ2 = 15.873, p = 0.001) between total dosage frequency of drugs prescribed in both hospitals. The relationship between total number of brands and generic prescription in both hospitals was significand (χ2 = 9.765, p = 0.002).
Conclusion: The generic prescription practices of parenteral drugs was prevalent in the two hospitals. Parenteral preparations were frequently used in the two hospitals.
Keywords: Infusions; Parenteral Nutrition; Drug Utilization; Critical Care; Electrolyte Imbalance
Introduction
Background
Parenteral nutrition is the intravenous administration of a nutritionally balanced and physicochemical stable sterile emulsion or solution. It is indicated when the GIT is inaccessible, inadequate or inappropriate to meet the patients on going nutritional needs or gut rest is indicated. Parenteral nutrition (PN) is a complex therapy containing more than 40 components, including dextrose, amino acids, fat emulsions, water, electrolytes, trace elements, and vitamins. To order PN appropriately, clinicians need to have a good understanding of body composition, fluid balance, electrolyte assessment, and acid-base balance. Human cells consist of 65% to 90% water, water and solutes pass through cell membranes both actively and passively, specific fluid and electrolyte concentrations are necessary in order for cell metabolism to occur, and these balances are affected by different stresses including trauma, surgery, and critical illness [1-4]. While fluid loss both measurable and insensible, occurs with these stressors, replacement and maintenance fluids are commonly administered without consideration of specific patient needs. Protocols and order sets allow for one size fits all fluid management that, though the time efficient, may not optimize patient recovery and may be detrimental. A patient fluid and electrolyte status affects all organ systems. Improper dosing can exacerbate already injured systems. The human body in a state of wellness has a remarkable capacity to make small and large adjustments in fluid and electrolyte intake and mobilization for specific needs. In a state of illness these compensatory mechanisms are disrupted, and recovery is dependent on restoration of an appropriate balance [4- 6].
Introduction
The birth of a baby is a natural process and an important and joyful social event for the individual family and the wider community. However, the time of birth and the first month is a very risky period for the child (Compaoré). Every year 2 million newborns die within 24 hours of their life, 99% of these deaths occur in low-income countries. Approximately 4 million births are recorded as neonatal deaths each year worldwide, ¾ of them occurring in the first week of life with the risk in the first day. WHO (2013) observed that despite a global decline of nearly 50% of the mortality rate among children under five, which rose from 90 to 48 deaths per 1,000 live births between 1990 and 2012, the neonatal mortality rate only decreased by 36% from, during the same period, 33 to 21 deaths per 1000 live births. This resulted in children under five years, an increase in the proportion of deaths occurring during the neonatal period, from 37% in 1990 to 44% in 2012 when 2.9 million children died in the month after birth, mainly from preventable causes. The neonatal mortality rate is an indicator of the quality of obstetric and neonatal care. It depends on the level of socio-economic development of a country. For SANIFO Hope Foundation (2013), 82% of newborn deaths are the 58 developing countries classified as high risk, and each year 2 million newborns die within 24 hours of their existence.
Fluid, electrolyte, and nutrition management is important because most infants in a neonatal intensive care unit (NICU) require intravenous fluids (IVFs) and have shifts of fluids between intracellular, extracellular, and vascular compartments. Therefore, careful attention to fluid and electrolyte balance is essential. If inappropriate fluids are administered, serious morbidity may result from fluid and electrolyte imbalances. Inadequate attention to nutrition in the neonatal period leads to growth failure, osteopenia of prematurity and other complications. They are utilized to ensure an adequate delivery of calories and protein when patients are unable to take sufficient food by either the oral route or via feeding tube. PN is utilized in a variety of patient populations, including surgical patients, severely malnourished patients, and the critically ill ones at intensive care unit. Nutritional support is a recognized determinant of outcome in critically ill patients. Development of critical care services in Nigeria has not been accompanied by certain appropriate ancillary support services such as adequate nutritional support [7-9]. Parenteral preparations is mostly prescribed for surgery and patients in intensive care units. In this era of ongoing identification and analysis of medical errors, fluid and electrolyte management has trailed behind the medical decisions that have immediate obvious adverse consequences, perhaps because the effects of fluid mismanagement appear as multiple organ system failings that are attributed instead to progression of the underlying disease in the patient. This predicament may also reflect a lack of understanding of the importance of considering individual volume and electrolyte abnormalities as a separate variable that can significantly alter a patient course and outcome [8-9].
The evaluation of utilization of parenteral preparations in the aforementioned health facilities have not been carried out as no previous published literature were found. The study therefore, seeks to document a comprehensive parenteral utilization report of the health facilities and generate evidence-based information for intervention studies, and add to knowledge in promoting value based services, resource allocation, planning and better health care service delivery in our health facilities. This study evaluated the utilization of parenteral preparation for fluid electrolyte and nutrition, and document information for interventions and policy.
Methods
Study Location and Study Site
The study was carried out in two hospitals in Anambra State namely; St Charles Borromeo Hospital Onitsha, and Chukwuemeka Odumegwu Ojukwu University Teaching Hospital (COOUTH), Awka. St Charles Borromeo hospital is a mission hospital situated in the densely populated town called Onitsha with approximately 120 beds capacity. Onitsha is the commercial nerve center of the state predominantly inhabited by businessmen, artisans, civil servants and traders. It is demarcated from on the western side by the River Niger. COOUTH is situated at Awka, the capital city of Anambra State with 15 Departments and a bed capacity of about 400. Both towns are located in the tropical rain forest belt of eastern Nigeria.
Study Population
The study was carried out using eligible folders that met the inclusion criteria for in-patients who were admitted in the hospitals as inpatient within January 2017 and December 2018.
Sampling Method
All the eligible folders that met the inclusion criteria in the medical wards, surgical wards, and accident and emergency units were utilized to increase reliability.
Data Collection and Assessment of Collected Data
Data was collected using structured observational check list for parenteral utilization, patient care and health facility indicators. Data covering parenteral utilization was obtained from medical records retrospectively and filled in structured check list accordingly with careful observation.
Study Period
The study lasted from March 2018 to October 2018.
Statistical Analysis
The data was checked, cleansed and analyzed using the SPSS software program version. Descriptive statistics frequency, percentage, means and standard deviation was used to summarize the data.
Inclusion Criteria
a) All folders/patient records with parenteral preparation that felled between the stated periods but were ineligible
b) All the inpatients folders of patients that contained parenteral preparations.
Exclusion Criteria
a) All folders/patient records that contains parenteral within the period which
b) All folders containing other health devices and aids apart from parenteral.
c) All patients that are not inpatients.
d) Illegible Folders
Ethical Consideration
Ethical approval was obtained from the Research and Ethics Committee of Chukwuemeka Odumegwu Ojukwu University Teaching Hospital Nnewi before commencement of the study. Every form of patient’s identification was concealed in line with global best practices.
Results
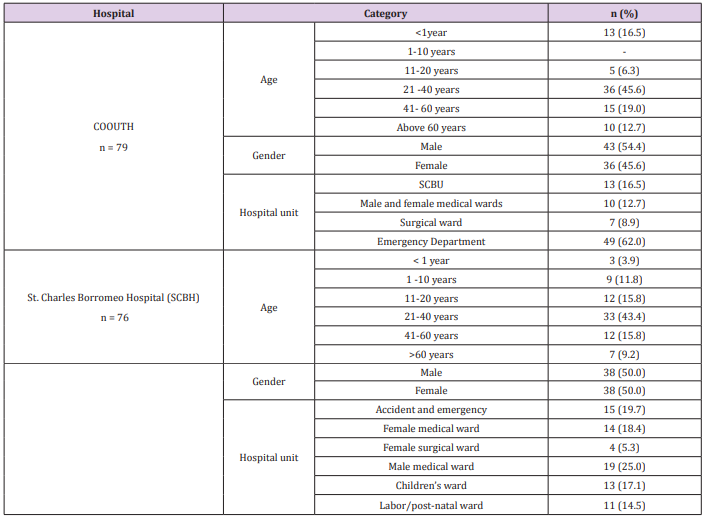
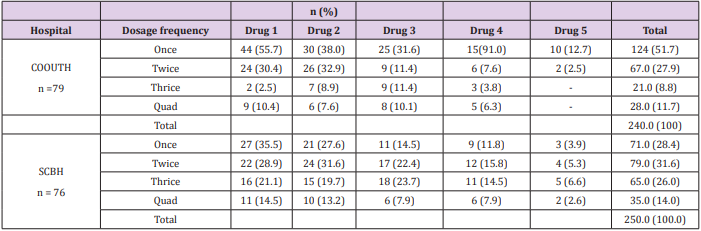
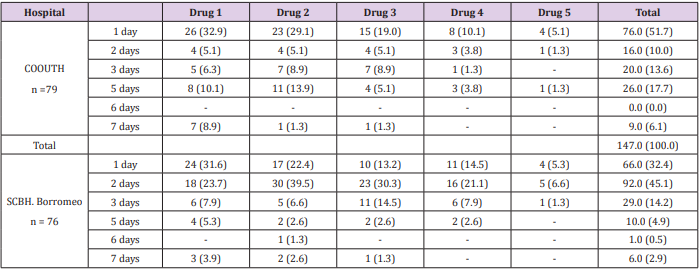
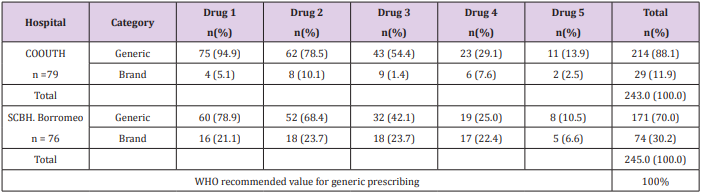
Demographic characteristics of patients in Chukwuemeka Odumegwu Ojukwu University (COOUTH) and Saint Borromeo hospitals (SCBH) showed that 79 patients from COOUTH and 76 patients from SCBH that received various parenteral preparations for various ailments were selected for the study. At COOUTH, majority of patients (36, 45.6%) were between 21 -40 years with average age of 29.0 ± 5.8 years while 15 (19.0%) with average age of 48.7 ± 5.1 years were between 41 – 60 years as shown in Table 1. Table 2 showed the classes of parenteral drugs prescribed for various ailments at COOUTH and SCBH. Antihistamines was the only un-prescribed class of medication at SCBH. There was no significant association in the distribution of various classes of medications in both hospitals, as revealed by Chi-square test (χ2 = 11.063, p =0.806). Dosage frequency of drugs prescribed at COOUTH and SCBH. Chi-square test as shown in Table 3, revealed a statistically significant association (χ2 = 15.873, p = 0.001) between total dosage frequency of drugs prescribed in COOUTH and SCBH as shown in Table 3. Table 4 indicated dosage duration of medications prescribed at COOUTH and SCBH. Dosage durations of total medications prescribed in both hospitals differed significantly as revealed by Chi-square (χ2 = 34.748, p = 0.005) between total dosage frequency of drugs prescribed in COOUTH and SCBH as shown in Table 4. Table 5 showed the categories of drugs prescribed at COOUTH and SCBH. In COOUTH, more generic drugs (214, 88.1%) were prescribed than the branded drugs (29, 11.9%). Similar trend occurred at SCBH, where higher number of drugs prescribed were generic (171, 70.0%) compared to branded prescriptions (74, 30.2%).
Table 1: Demographic characteristics of patients in Chukwuemeka Odumegwu Ojukwu University (COOUTH) and Saint Borromeo hospitals (SCBH) that were selected for the study.
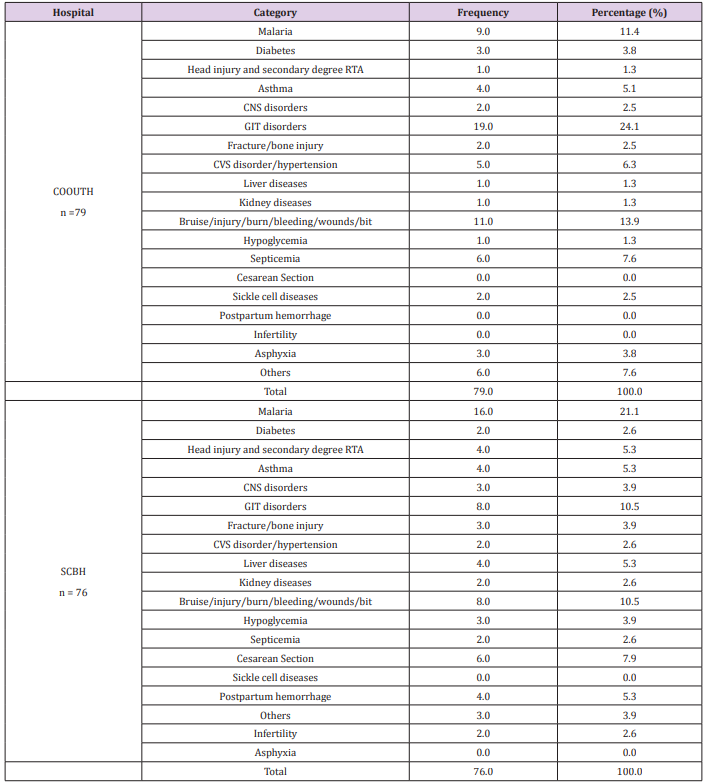
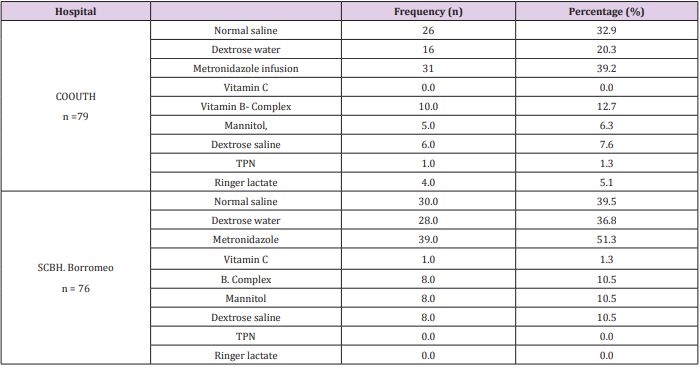
Chi-square test shown in Table 5, revealed a statistically significant association (χ2 = 9.765, p = 0.002) between total number of brands and generic prescription in COOUTH and SCBH. Ailments diagnosed at COOUTH and SCBH. Table 6 depicts frequency of various ailments diagnosed in COOUTH and SCBH. Prevalence of diagnosed ailments in COOUTH include; GIT disorders (19.0, 24.1%), Test of association using Chi-square reveled that there was a statistically significant different (χ2 = 44.384, P = 0.001) between the distribution of various diseases in both hospital, as they did not follow the same trend in prevalence. In Table 7, combination of medications prescribed with infusion in COOUTH and SCBH showed that normal saline, dextrose water and metronidazole were the most commonly combined infusions with other medications in both hospitals. The trend in both hospitals were almost similar as test of association using Chi-square did not reveal significant difference (χ2 = 11.880, p = 0.157).
Table 6: List of ailments diagnosed at COOUTH and SCBH. CVS: cardiovascular system, CNS: central nervous system, GIT: gastrointestinal tract, TRA: road traffic accident
Discussion
The Use of Parenteral Preparation in The Hospitals
In view of the clinical relevance of using parenteral forms, evidenced in different studies, it is essential that they be administered adequately. A tool that contributes to this goal is the adoption of good intravenous therapy practices in healthcare services [10,11]. Infusions form an essential part of inpatients prescription especially in tertiary hospitals with critically ill patients. Good understanding of their utilization pattern will aid procurement and eliminate the out of stock syndrome especially in emergency situations [12,13]. Delays in rational use of infusions and parenteral preparations is usually associated with life threatening emergencies and fatalities [14,15]. The study suggested that infusions were predominantly prescribed in the two hospitals and was present in the first two drugs prescribed to patients. This was an indication that most of the hospitalized patients have either undergone surgery or were affected by varying cases of electrolyte imbalance. Among the infusions, antibiotic preparations were very common. Hence, the rationale for the frequent antibiotics’ infusion prescription. This calls for antibiotic resistance stewardship. Most severely ill patients are placed on non-per-oral (NPO). Some other patients are emergency situation that required instant response that can by-pass the first pass metabolism especially in critical care. Emerging clinical studies suggest that patients in critical conditions benefit more from longer exposure of higher antibiotics especially at levels above the minimum inhibitory concentration (MIC) than results from in vivo and in vitro studies [16,17]. TPN is recommended for extended period in complications like pulmonary embolism [18].
Similarly, at SCBH, anti-microbial drugs, infusions and antimalarial appeared as the most commonly prescribed medications found in majority and occurring within the first three drugs prescribed to patients. This suggests that malnutrition is a common problem in most hospitalized patients. Surgical patients with malnutrition have around three times more post-operative complications and four times greater risk of death than well-nourished patients with similar operations [19]. The outcome of the class of drugs frequently prescribed in the two hospitals indicated that parenteral antibiotics were the leading infusions in the two hospitals. This supports a study in Nigeria by Enwere et al. which reported high prescription of parenteral antibiotics [20].
Infusion Use and Prescription Practices in The Hospitals
Most of the infusions were predominantly administered either once or twice daily in the two hospitals. This is associated with the level of patients need and clinician’s judgement and practices. Most hospitalized patients are either critically ill or have undergone surgeries and needs calories, proteins and other total parenteral nutritional substituents and electrolyte replacement. The study observed that the first, second and third medicine prescribes had higher prescription rates than the fourth and fifth drugs in both hospitals. This suggests indications for the predominant cases in commonly prevalent at the locations and suitability of frequently occurring medications [21]. However, a study suggested that clinicians usually prefer newer effective preparations with better profile to other existing options [22,23]. Prior drug utilization studies suggested that the tolerability of a drug may have more impact on the long term retention when compared to efficacy while changes in outcomes of therapy decides the retention of complement agents [24-26].The outcome showed that the dosage frequency in the two hospital varied significantly. Once a day dosing occurred more in the two hospitals assessed. It could be attributed to the nature and availability of preparations which usually applied most times in emergency situation before switching over to oral ones. Most of the infusions administered lasted for one to five days. Prolonged infusion of antibiotic in resistant infections has been demonstrated to have positive impacts on pharmacotherapy [27,28].
Categories and Types of Medications Available
More generic drugs prescriptions were common to both hospitals compared to branded prescriptions. However, the percentage generic prescription still felled below standards for the two hospitals. Previous study suggested that generic prescribing reduces patient’s confusion and medication errors [29]. Another study saw it as, “an indication of good practice” and a way of viable low-cost medications [30-32]. Generic prescribing in the hospitals was in conformity with the WHO recommendations and international best practices [33]. The idea of prescribing generic drugs will leave the patients with some many options on the costeffective drugs to purchase, hence encouraging compliance. The generic prescription pattern from this study was better than the outcome in another work done in a teaching hospital in western Nigeria where the percentage of generic prescription from the study were much lower than that obtained in this study [34].
Other studies in the western and northern parts of Nigeria indicated values below 50% generic prescribing [35-37]. A study on the knowledge perception and, attitude of physicians on generic medicine prescribing suggested that therapeutic failure was a major concern that discourages generic prescribing [38]. However, another study in western Nigeria indicated that decline in generic prescribing was associated with the activities of pharmaceutical marketers who press for the prescription of their brands [37]. The list of ailments and individual parenteral medications prescribed indicated critically ill and emergency conditions which validated the use of parenteral preparations and infusions [38-42].
Conclusion
The use of parenteral preparations in the hospitals was achieved and the trend of prescription and utilization was determined. The categories and types of parenteral nutrition available were assessed and the disease pattern associated with their utilization were ascertained which mostly indicated electrolyte imbalance. The generic prescription and substitution practices of parenteral drugs in the two hospitals were assessed and were concluded to be more of generic than branded drug prescription. Thus, it can be concluded from the research that parenteral preparation can be inferred to be frequently used in the two hospitals assessed in South-eastern part of Nigeria.
Acknowledgement
We would like to acknowledge Nnamdi Azikiwe University for providing a conducive environment for research work.
References
- Agren J, Zelenin S, Hakansson M, Eklöf AC, Aperia A, (2003) Transepidermal water loss in developing rats: role of aquaporins in the immature skin. Pediatr Res 53(4): 558-565.
- Auron A, Mhanna MJ (2006) Serum creatinine in very low birth weight infants during their first days of life. J Perinatol 26: 755-760.
- Chiou YB, Blume-Peytavi U (2004) Stratum corneum maturation. A review of neonatal skin function. Skin Pharmacol Physiol 17(2): 57-66.
- Deshpande KS (2003) Total parenteral nutrition and infections associated with use of central venous catheters. American Journal of Critical Care 12(4): 326-327: 380.
- Greta L Piper, Lewis J Kaplan (2012) Fluid and electrolyte management for surgical patients 92(2): 189-205.
- Hartnoll G, Betremieux P, Modi N (2000) Body water content of extremely preterm infants at birth. Arch Dis Child Fetal Neonatal 83 (1): F56-59.
- Omar SA, DeCristofaro JD, Agarwal BI, La Gamma EF (2000) Effect of prenatal steroids on potassium balance in extremely low birth weight neonates. Pediatrics 106(3): 561-567.
- Peters O, Ryan S, Matthew L (1997) Randomized controlled trial of acetate in preterm neonates receiving parenteral nutrition. Arch Dis Child Fetal Neonatal Ed 77(1): F12-155.
- Rollins CJ, Elsberry VA, Pollack KA, Pollack PF, Udall JN, et al. (1990) Three-in-one parenteral nutrition: a safe and economical method of nutritional support for infants. JPEN J Parenter Enteral Nutr 14 (3): 290- 294.
- (2008) The Brazilian Health Surveilance Agency Regulations and Legislations 2008. Assessen online on 23 May 201.
- Manjiani D, Paul DB, Kunnumpurath S, Kaye AD, Vadivelu N, et al. (2014) Availability and utilization of opioids for pain management: global issues. Ochsner J 14(2): 208-215.
- Meissner W, Coluzzi F, Fletcher D, Huygen F, Morlion B, et al. (2015) Improving the management of post-operative acute pain: priorities for change. Curr Med Res Opin 31(11): 2131-2143.
- Greta L Piper, Lewis J Kaplan (2012) Fluid and electrolyte management for surgical patients 92(2): 189-205
- Dellinger RP, Levy MM, Carlet JM, Bion J, Parker MM, et al. (2008) Surviving sepsis Campaign: international guideline for management of sepsis and septic shock 2008. Intensive Care Med 34(1): 17-60.
- Kumar A, Robberts D, Wood KF, Light B, Parrillo JE, et al. (2006) Duration of hypotension before initiation of effective antimicrobial therapy is the critical determinant of survival in human septic shock. Crit Care Med 34: 1589-1596.
- Lodise TP, Lomaestero B, Drusano GL (2007) Piperacillin –tazobactam for pseudomonas aeruginosa infection: clinical implications of an extended infusion dosing strategy. Clin Infect Dis 44: 357-363.
- Sinnolareddy MG, Robberts MS, Lipman J, Robberts JA. Beta-lactam, et al. (2012) Pharmacokinetics/Pharmacodynamics in critically ill patients and strategies for dose-optimization – a structured review. Clin Exp Pharmacol Physiol 39(6): 489-496.
- Mailloux RJ, DeLegge MH, Kirby DF (1993) Pulmonary embolism as a complication of long-term total parenteral nutrition. JPEN. J Parenter and Enteral Nutr 17(6): 578-582.
- Samaneh B, Sepideh E, Hossein K, Saeed R (2012) Evaluation of Parenteral Nutritional Support in the Surgical and Medical Wards of a Referral Teaching Hospital 20(1) :60.
- Enwere OO, Falade CO, Salako BL (2007) Drug prescribing pattern at the medical outpatients’ clinic of a tertiary hospital in South-Western Nigeria. Pharmacoepidemiol Drug Saf 16(11):1244-1249.
- Martinez-Castaldi C, Silverstein M, Bauchnner H (2008) Child versus adult research: the gap in high quality study design. Paediatrics 122(1): 52-57.
- Cohen E, Uleryk E, Jasuja M, Parkin PC (1985) An absence of pediatric randomized controlled trials in general medical journals 60(2): 118- 123.
- Bourgeois FT, Murthy S, Pinto C, Olson kl, Ioannidis JP, et al. (2012) Paediatric versus adult conditions with high paediatric disease burden. Paediatric s 130(2): 285-292.
- Bootsma HP, Ricker L, Hekster YA, Hulsman J, Lambrechts D, et al. (2009) the impact of side effects on long term retention in three new antiepileptic drugs. Seizure 18(5): 237-331.
- Bootsma HP, Ricker L, Diepman L, Gehring J, Hulsman J, et al. (2008) long-term effects of levetiracetam and topiramate in clinical practice: A head-to-head comparison. Seizure 17(1): 19-26.
- Wong IC, Mawer GE, Sander JW, Lhatoo SD (2001) A Pharmacoepidemiologic study of factors influencing the outcome of treatment with lamotrigine in chronic epilepsy. Epilepsy 42(10): 1354- 1358.
- Lodise TP Jr, Lomaestro B, Drusano GL (2007) Piperacillin-tazobactam for pseudomonas aeruginosa infection: clinical implications of an extended infusion dosing strategy. Clin Infect Dis 44: 357-363.
- Hyuck L (2016) Prolonged or continuous infusion of IV Antibiotics as initial treatment strategy. Infect Chemother 48(2): 140-142.
- Grant M (2017) Prescribing generic drugs will reduce patient confusion and medication error. Monash University 2017.
- Sudhanthar S, Turner J, Thakur K, Sigal Y (2015) Improving low cost generic medication prescription rate in primary care pediatric practice. BMJ Quality Improvement Programme 4(1): 1-3.
- Mathew P (2015) Generic drug review and experiences from South India. J Family Med Prim Care 4(3): 319-323.
- Duerden MG, Hughes DA (2010) Generic and therapeutic substitution in the UK: are they a good thing? Br J Clin Pharmacol 70(3): 335-341.
- (2019) WHO Action programme on essential drugs; Guide to good prescribing. Geneva. Accessed online on 23 May 2019.
- Sodipo OO, Adedokuk A, Adejumo O (2017) Drug prescription pattern in a Nigerian teaching hospital. NJPF 8(4): 29-34.
- Akande TM, Oloye MO (2007) Prescription Pattern at a secondary health facility in Ilorin Nigeria. Annals of Afri. Med 6: 186-189.
- Tamuno I, Fadare J (2012) Drug prescription pattern in a Nigerian teaching hospital. Tropical Journal of Pharmaceutical Research 11(1): 146-152.
- Adebayo ET, Hussain NA (2010) Pattern of prescription drug use in Nigerian Army Hospitals. Annals of Afri. Med 9:152-158.
- Fadare JO, Adeoti AO, Desalu OO, Enwere OK (2016) The prescribing of generic medicines in Nigeria: knowledge, perceptions and attitudes of physicians 16(5): 639-650.
- Crook J (1979) Method of audit in drug use. In Duchene-Marulla ZP. Ed. Advances in Pharmacology and Therapeutics. Proceedings of 7th International Congress of Pharmacology, Paris, 1978. Oxford Pergamon Press pp. 189-195.
- Lee D, Bergman U (2000) Studies of Drug Utilization. In: Strom B (Eds.), Pharmacoepidemiology, 3rd (edn.). Chichester J Wiley pp. 463-481.

 Research Article
Research Article