Abstract
The rapid growth and uncontrolled utilization of episiotomies in most of the cities around the world have led to contrasted social, psychological, economic and health problems. These chirurgical operations are even nowadays very frequently practiced on pregnant women in rural areas during delivery, sometimes without a significant scientific indication. This study aimed to determine the frequency and indications of episiotomies practiced at the referral Hospital of the Kenge health zone (HGRCCK) in Kwango province to assess the efficacy of such a practice using data from a small survey based on health records coupled with an interview. The sample included 78 women having undergone an episiotomy randomly selected out of 1981 periurban pregnant women received at the maternity from January 2013 to December 2014. The study mainly used frequency distributions to analyze these data and found a crude rate of 3.6% in 2013 and 4.3% in 2014. This meant a mean annual rate of 3.95%, which is significantly below global standards set by WHO of 10 to 20%. Young women were the most affected by episiotomies, especially those which age ranged between 15 and 20 years old (representing 64.1%), followed by the 21-25 years old (25.6%). In terms of parity, the primiparians were the most vulnerable group with a record of 80.8% of episiotomies. The most indicated reasons for practicing such episiotomy operations encompassed maternal weakness at delivery (26.9%), fetal microsomal (25.6%), fetal suffering (15.4%), shoulders’ dystocia (12.8%) and, unfit seating presentation (10.3%). The immediate complications observed after delivery were bleeding (15.4%) and perinea cut (5.1%). Late complications included dyspareunia (12.8%) and scar’s pains (6.4%). There is thus a need to sensibly reduce the practice of episiotomies even though some practitioners recommend its systematic application on the primiparians due to its benefits.
Keywords: Child Delivery; Complication; Episiotomy; Frequency; Obstetrical Surgery
Introduction
Episiotomy is the most common surgical procedure performed on women. Its use is so routine that one seems to forget that it is a surgical procedure, with the risks, complications and consequences that entails [1]. Episiotomy is also among the most common acts in hospitals and clinics in rural areas. There is therefore a need to validate the relevance of its indications, as is customary for any medical procedure. WHO recommends that episiotomy be considered only during complicated vaginal delivery (siege, dystocia of the shoulders, vacuum extraction), scars of female genital mutilation, or complicated, poorly healed perineal tears, in which cases of fetal distress and fetal macrosomia [2]. Episiotomy is a very common medico-surgical procedure for primipara. It has become almost systematic in maternity hospitals. Although its systematization is recent, it remains an old medical practice since it was described for the first time in 1741 [3].
The episiotomy rate is not the same everywhere. This surgical practice varies from one country to another but also from one region to another within the same country. Hence the need for researchers to educate the medical profession, nurses and midwives to r complies with WHO recommendations to reduce this practice. At the current state of research, it is difficult to set an “ideal” rate of episiotomy. WHO, in the 1990s, recommended not to exceed 10 to 20% [4]. She speaks of cultural drift when this rate is> 20%.
In France, it represented 51% and rose to 71% among primiparous women compared with 36% for multiparous women in 1998. Between 2000-2003, this overall rate was 46% and has tended to decrease in recent years due to a reconsideration. from his indications. In England, the overall rate in 1980 was 52%. In primiparous women it was 70.5% compared to 38.3% for multiparous women. In 2002, this overall rate dropped to 13%. In the United - States, the overall rate was 65% in 1979 and fell to 19% in 2000. In Mexico the episiotomy rate in primiparous was 69% between 1995-1998; in Argentina, it stood at 86% between 1995- 1998. In Brazil it was 94% between 1995-1998. In Zimbabwe, the overall rate was 27% between 1997-1998. In Ethiopia, the overall rate was 5% between 1998 and 2001. In Nigeria, the overall rate was 55% in 1997. In Mali, it was 13.76% in 2004 [2,5].
Moreover, e comm it is customary for any medical procedure, episiotomy should be the collection of patient consent outside of life-threatening emergencies [4]. However, the survey carried out in some hospitals in France revealed that 85% of episiotomies are performed without a request for consent from the delivery professionals. This figure does not seem to have changed since 2005. If we compare what women say in the way they were informed by whether they had an episiotomy, we see that those who had an episiotomy are three times more numerous. to answer that they had information, but insufficient. It is likely that, confronted with the reality of the episiotomy, its realization, its suture, its consequences, the women discover on this occasion that they lacked in fact information [6].
Being practiced systematically in the obstetrical sector, one may wonder whether it is medico-surgical sister t o u t that in recent years, scientists advocating this gesture began remett in question its effectiveness, among other things because it was introduced without solid scientific evidence. Today, more and more voices are being raised to say that it should be used much more restrictively. These controversies have led some obstetricians to remett questioned the desirability of a principled episiotomy in women giving birth for the first time. “It is not necessary They said,” that in case of risk of big tear or if the duration of the expulsion is too prolonged “ [4]. So, our study screw has to determine the frequency of episiotomies performed in s the General Hospital of Catholic Conventionné reference (HGGRC) Kenge 1 and identify the heart’s guidance through a miniment identifies actions are posed.
Review of the Literature
Episiotomy is a banal gesture that causes no real debate in the daily practice of maternity. An episiotomy is an operation that consists of cutting the perineum from the posterior commissure of the vulva. It concerns the skin, the vaginal mucosa, the superficial muscles of the perineum and the pubral rectum. It is the most widely performed obstetric intervention worldwide [7,8]. This act has several expected benefits including the prevention of firstdegree perineal tears; preventing complicated perineal tears of the 2nd and 3rd degrees; protection of the pelvic floor and thus the prevention of urinary and faecal incontinence and, in general, prolapse; prevention of fetal distress; the prevention of certain dystocia [7].
One study showed a decrease in the use of episiotomy during instrumental delivery in the primipara does not significantly alter the rate of severe perineal tears and did not improve maternal symptoms postpartum. On the contrary, there has been a tendency to increase the rate of severe perineal tears, in agreement with other authors, and a significant increase in micturition disorders in the limited-use group of episiotomy. Perineal disorders are more often responsible for non-resumption of sexual intercourse and depressive symptoms for women in this group [8].
It has therefore been shown that primiparity remains one of the main determinants of the use of episiotomy with a significant increase for a maternal age of 25 to 29 years, corresponding to the average age of the first child in France, and a risk of episiotomy multiplied by 8.79 in case of single antecedent caesarean section. In addition, it has been shown that the duration of expulsive efforts between 25 and 35 minutes increases the use of episiotomy. As for the protective factors of episiotomy, we have noted: the history of intact perineum, the beginning of expulsive efforts in the case of a low presentation, and a duration of expulsive efforts of less than 25 minutes [9]. However, analysis of the literature shows generally that episiotomy did not beneficial actions on the pelvic floor, or on the healthy fetus. His practice must therefore be advocated selectively and restrictively. Most authors have shown that a rate above 30% is not accompanied by any of the expected benefits.
In 2005, the College of Gynecologists National Obstétriciens (CNGOF) issued recommendations practice of episiotomy. These recommendations noted that episiotomy does not have to be routine and set a goal of lowering the national rate to 30% or less of episiotomies compared to 47% in 2002-2003 [10]. A study carried out in France, establishes an association between freedom of movement and episiotomy, in primipares as in multiparas. The more the woman is free to move during work, the lower the episiotomy rates. For example, 40% of primiparas who can move during all work have an episiotomy, while the proportion is 46% for those who can move partially, and 53% for those who can not move. The trend is the same for multiparas, 11%, 18% and 21% [6].
There is also a link between consent and the suffering experienced by women after episiotomy. Women who have been asked for consent and who have accepted are less likely to have suffered, compared to women who have not been asked for consent (65% versus 78%). This aspect is important for women. There are at least two explanations to consider: the feeling of suffering depends on how the woman was treated, and the request for consent is part of good treatment. The most respectful consent teams would also pay more attention to s suite of episiotomy [6]. However, it is undeniable that serious perineal complications related to the absence of episiotomy or even caesarean section may lead many of us before magistrates in the current context [7]. Hence the necessities to raise this issue in a semi-urban environment like Kenge, DRC.
Materials and Methods
Description of the Study Environment
Our study was conducted at the Kenge Catholic Reference General Hospital (HGRCCK). Located on Dispensary Avenue in Kenge City, Capital of Kwango Province, Kenge Rural Health Zone, Democratic Republic of Congo (DRC). The hospital is 275 km from Kinshasa and its entrance is 1.5 km from the national road N°1 Kinshasa-Kiiwit
The HGRCCK is a state hospital established for the indigenous population since 1958. In January 1960 the Administrator of the territory, Mr. Noël Kikwa, completed the construction of the building that currently houses Internal Medicine. Shortly after independence, the clinic operated in the current building of the Provincial Health Inspectorate and Maternity in the pavilion where the operating theater is currently located.
In 1988, a partnership was signed between the German Government and the Congolese state including the Diocese of Kenge. It is thanks to this partnership that a project will be funded that rehabilitated the clinic and at the same time created the Kenge Rural Health Zone with Kenge Hospital 1, as the General Reference Hospital.
Its administrative and technical structure includes a management committee, a Kenge Rural Health Zone Framework Team and a Hospital Steering Committee. The Congolese state has ceded the management of this hospital to the non-profit organization Diocese of Kenge. Kenge HGRCC 1 offers a complementary package of activities and organizes curative, preventive and promotional activities.
Sampling Method and Data Collection Technique
The sample is a simple random and comprehensive randomized probability sample of all cases of episiotomy performed from 2013 to 2014. This study population consists of 78 women who had undergone episiotomy among the 1981 women who gave birth in this maternity ward. Our study covers the period from January 2013 to December 2014. In most cases, the investigator referred to patient records and observations made by surgeons and obstetricians at the hospital. But in some cases, the respondents were visited at home and questioned impromptu as they went about their housework.
Selection Criteria: Before including any subject in the study sample, the researcher first made sure that the person was female and of childbearing age. She also had to have had at least one episiotomy during previous deliveries between January 2013 and December 2014. Only women from a Kenge Health Zone household were included in the analysis.
Criteria Exclusion: The sample was meant to exclude any female subject living outside the Kenge Health Zone who had not undergone an episiotomy between January 2013 and December 2014.
Technical Analysis Data
The analysis was descriptive, based essentially on the calculation of frequencies. The data has been classified in tables and graphs have been used to facilitate the visibility of the calculated frequencies. The trends identified were based on the following formula:
Or,
f (%) = Relative frequency in percentage
FO = Frequency observed
FA = Expected frequency
Results and Discussion
Frequency Episiotomies
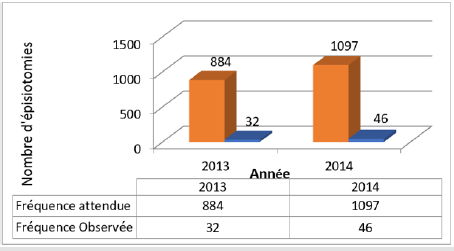
Figure 1 indicates that the frequency of episiotomies during the two years of study was 3.6% for the year 2013 and 4.3% for the year 2014. There is therefore an increase of 19.4% in 2014 compared to 2013. The overall annual rate was therefore 3.95%.
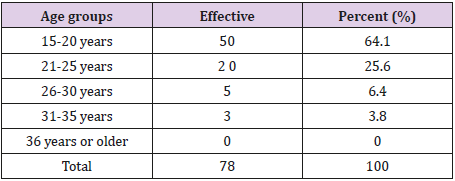
Regarding the distribution of respondents by age group, Table 1 reveals that those whose age is between 15-20 years accounted for 64.1% followed by that of 21-25 years with 25.6%. Respondents aged 26-30 accounted for 6.4% and those aged 31-35 3.8%. No cases were reported in the 36+ age group. These results show that age influences the practice of episiotomies.
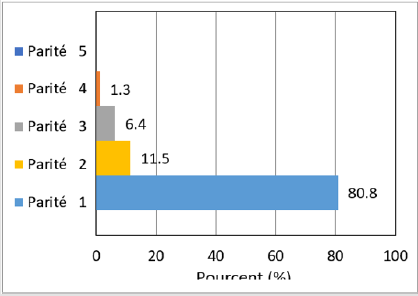
Figure 2 shows the proportion of episiotomies as a function of parity. It emerges that the primiparous ones underwent more episiotomies with 80,8%. Those who gave birth for the second time are in second place with 11.5%. Those who give birth for the third and fourth time represent respectively 6.4% and 1.3%. Those who gave birth 5 times or more did not undergo any episiotomy. These results show a link between parity and the use of episiotomy. The primiparous have undergone more episiotomies. This trend decreases with the number of births.
Indications of Episiotomies
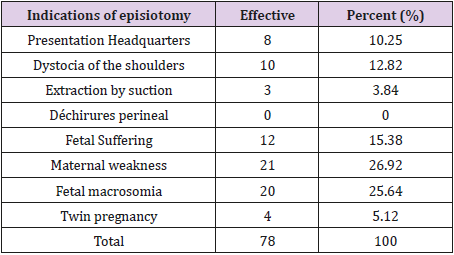
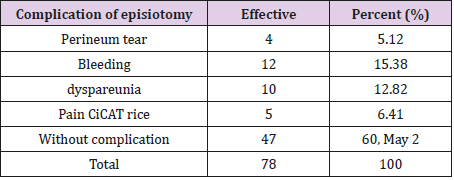
Table 2 presents the indications of episiotomies performed. This proportion is 26.92% for maternal weakness; 25.64% for fetal macrosomia; 15.38 for fetal suffering; 12.82% for shoulder dystocia; 10.25% for the seat presentation; 5.12% for twin pregnancies and finally 3.84% for suction extraction and 0% for scars for sexual mutilation and perineal tears. In addition, 15.38% of episiotomy complications were observed in terms of bleeding; 12.82% of complications from dyspareunia; 6.41% due to scar pain; and 5.12% of complications from a perineal tear (Table 3). The vast majority of 60.25% had no complications. It should be noted here that some complications were observed while the women were still in the maternity ward, while others (dyspareunia, scar pain) were reported during post-natal consultations.
Discussion of Results
Discussion on the Frequency of Episiotomies
This study showed that for the first year (2013), the frequency of episiotomies was 3.6% and 4.3% for the second year (2014). There is a 19.4% increase in episiotomies between 2013 and 2014 with an average annual rate of 3.95%. Although there is a slight increase in episiotomy in 2014 compared to 2013, their overall rate is in the standards set by the WHO, ie 10 to 20% [2]. This rate of HGRCCK episiotomies remains lower than that of the Mans obstetrics department in France, which drastically fell by 30% to 5%, in three years, thanks to the efforts of Dr. Jacques Mouchel [4].
The results of women with episiotomies show that age influences the practice of episiotomies. Women aged between 15- 20 years accounted for 64.1% followed by women aged 21-25 with 25.6%. Respondents aged 26-30 accounted for 6.4% and those aged 31-35 3.8%. No cases were reported in the 36+ age group. We clearly observe younger ones were more exposed to episiotomies than older ones. More women increased in age less there were episiotomies. These results are similar to those found by Aissata [2] in the Gynecology-Obstetrics Department of Somine Dolo Hospital in Mali and Coulibaly [5] in the Gynecology and Obstetrics Department of Gabriel-Touré Hospital in Mali.
The distribution according to parity showed that primiparous women alone underwent 80.8% episiotomies. Women who gave birth for the second time came in second with 11.5%. Third and fourth place were women who gave birth three times (6.4%) and four times (1.3%). Those who gave birth 5 times or more did not undergo any episiotomy. These results show a link between parity and the use of episiotomy. The primiparous have undergone more episiotomies. This trend decreases with the number of births. These results confirm those of several studies, notably that of CIANE [6] who found that in France the episiotomy rate for women at first birth was 47% in 2010-2013 and 16% for multiparous women, almost three times less than for primiparas. Aissata [2] found in Mali a rate of 83.30% among primiparas.
Discussion on Indications of Episiotomies
In addressing the indications for episiotomies, Table 3 shows that 26.92% were performed for maternal weakness; 25.64% for fetal macrosomia; 15.38% for fetal suffering; 12.82% for shoulder dystocia; 10.25% for the seat presentation; 5.12% for twin pregnancies and finally 3.84% for suction extraction and 0% for scars for sexual mutilation and perineal tears. At the current state of knowledge, indications of episiotomy are the subject of several controversies [9]. While some continue to recommend it systematically (Anglo-Saxon authors), others (the French) think that it should be applied restrictively but its indications are left to the discretion of the birth attendant [10,11].
Episiotomy is not an act without maternal complications, it is in itself a perineal lesion with significant morbidity [10]. Many women who gave birth (60.25%) did not have complications after episiotomy. The complications observed were classified into two groups: immediate complications observed while women were still in the maternity ward, such as bleeding (15.38%) and tears in the perineum (5.12%) and late complications observed during postnatal consultations such as dyspareunia (12.82%) and scar pain (6.41%). These results corroborate those of Aissata [2].
Conclusion and Recommendations
Conclusion
Episiotomies are among the most common acts of obstetrics. While some authors recommend that it be practiced because of its benefits, others doubt its relevance. Most specialists agree on the need to reduce it significantly, although some believe it is a routine application for primiparous women. However, the relevance of its indications continues to divide these specialists. But WHO recommends that episiotomy be considered only in the following cases: complicated vaginal delivery (siege, dystocia of the shoulders, vacuum extraction), scars of female genital mutilation or complete malformed complete perineal tears mastered and fetal suffering?
Recommendations
In view of the foregoing, it is recommended to the Kenge Catholic Conventional Reference General Hospital (HGRCCK) to organize training sessions to enable midwives and midwives to be retrained on new approaches to health. of the Mother of the Newborn and the Child (MNCH). Midwives must consider standards issued by WHO to avoid routine episiotomy practice; increase awareness to enable pregnant women to perform the 4 prenatal consultations recommended by WHO, which can facilitate good preparation for childbirth.
Summary
The rapid growth and sometimes uncontrolled use of episiotomies in most cities around the world has led to unexpected socio-psychological and economic consequences as well as contrasting health problems. However, episiotomy also becomes the most frequently performed surgical procedure in pregnant women living in rural areas during delivery, sometimes without a valid scientific indication. This study aimed to determine the frequency of episiotomies performed at the Kenge Catholic Reference General Hospital (HGRCCK) and to identify their indications through a minicensus of the acts performed in order to analyze the effectiveness of this practice. The sample was random and consisted of 78 women who had an episiotomy among the 1981 peri-urban women who gave birth in this maternity unit during the period from January 2013 to December 2014. The study mainly used the frequency distribution to analyze these data and found a 19.4% increase in episiotomies between 2013 (3.6%) and 2014 (4.3%) with an annual average of 3.95%.
This overall rate is significantly good to compare with the standards set by the WHO (between 10 to 20%). Young women were the most affected: 64.1% for the 15-20 age group and 25.6% for the 21-25 age group. The distribution according to parity shows that 80.8% of episiotomies were performed on primiparas. As for indications for episiotomies, 26.9% were made for maternal weakness; 25.6% for fetal macrosomia; 15.4% for fetal distress; 12.8% for shoulder dystocia; 10.3% for the seat presentation. The immediate complications observed were bleeding (15.4%) and tears in the perineum (5.1%) and late complications observed were dyspareunia (12.8%) and scar pain (6.4%). Thus, there is a need to significantly reduce the practice of episiotomies even if some are due to its systematic application to primiparous in terms of its benefits.
References
- Barbara K Rothman (1993) Encyclopedia of childbearing: Critical perspectives. Oryx Press pp. 126.
- Aissata S (2008) Episiotomy: The suture technique “a thread a knot” at the Gynecology-Obstetrics department of the Somine Dolo hospital: about 300 cases. Thesis, Faculty of Medicine of Pharmacy and Odonto- Stomatology, University of Bamako, Mali.
- Dutruge A (1995) Childbirth and medical patriarchy. Episiotomy p. 47- 49.
- Gogniat LF (2003) Routine episiotomy: An unfounded practice. Swiss Midwife 3: 24-29.
- Coulibaly M (2005) Episiotomy in the gyneco-obstetrics department of Gabriel-Toure Hospital. Thesis of Medicine, University of Bamako, Mali.
- (2013) CIANE, Interassociative Committee around the Birth 2013. Episiotomy: State of the art and experience of women. Births Survey File No. 6.
- Maillet R, Martin A, Riethmuller D (2004) Are there too many or too few episiotomies? Extract of updates in Gynecology and Obstetrics-Volume XXVIII, Twenty-Eighth National Days, National College of Gynecologists and Obstetricians French. Paris, France.
- Cabrieres A (2015) Instrumental extraction by Thierry’s spatulas in the primiparous: Maternal and neonatal impact of a decrease in the practice of episiotomy, thesis for the state diploma of doctor
- Iaconelli J (2014) The use of episiotomy: determinants of the practice of midwives. Study at the maternity hospital of Port-Royal. Memory to obtain the State Diploma of Midwifery, Faculty of Medicine of Paris Descartes, School of Midwifery Baudelocque, University Paris Descartes, France.
- (2005) CNGO, National College of Gynecologists Obstetricians (2005) Recommendations for clinical practice episiotomy. Gynecol Obstet Fertil 34: 275-279.
- Lacaille G (2016) Episiotomy: A month later. Prospective, descriptive and unicentric study of 30 patients. Mémoire, majeutical branch, Faculty of Medicine and Maïeutics, Catholic University of Lille, France.

 Research Article
Research Article