Abstract
The therapies to regenerate periimplant bone tissues have attracted lots of attention these years. Neural crest-related stem cells (NCSCs), a group of cells containing heterogeneous stem/progenitor cells, are capable of homing to injured tissues and participating in periimplant bone regeneration. The amplification of autologous NCSCs potential in homing for self-repair/regeneration, therefore, might be considered as an alternative therapy except for traditional cell transplantation. However, the knowledge of the NCSCs homing and participation in bone regeneration is still known little. Cell homing has been regarded as a process of exit of hematopoietic stem cells from blood vessels by trans endothelization and subsequent migration. Here we broadly define cell homing as active recruitment of endogenous cells, including stem/progenitor cells, into an anatomic compartment. Accordingly, research is becoming increasingly focused on the homing and stimulation of native cells.
For the purpose of directly observing NCSCs involvement in periimplant bone repair, different animal models were established to make their oral-derived NCSCs reconstituted with cells regenerating periimplant bone tissues. Here, we present a histological study for delivering homing factors to the site of implant placement by incorporation to allogen bone substitute as stem cell carrier material. We further show therapeutic strategies focusing on the stimulation of endogenous cells to support periimplant bone repair. NCSCs were found to aggregate in the periimplant niches and emerge in newly-formed bones or fibers. Some of them also co-expressed markers of fibroblasts or osteoblasts. These results indicated that NCSCs might contribute to the formation of new fibers and periimplant bone tissue during periimplant bone regeneration. In conclusion, we speculated that autologous NCSCs can shift into the surgical sites created by implant placement and participating in periimplant bone tissue repair.
Keywords: Human Neural CrestRelated Stem Cells (hNCSCs); Stem Cell Homing (hNCSCs homing); Allogen Bone Substitutes; Verticular Augmentation of Alveolar Ridges; Patient Observation Study; Histologically Controlled Study; Immediate Implant Placement
Abbreviations: NCSCs: Neural Crest-Related Stem Cells; MSCs: Mesenchymal Stem Cells; NBF: New Bone Formation; SCTG: Subepithelial Connective Tissue Graft; PMMA: Poly methyl Methacrylate; EGF: Epidermal Growth Factor
Introduction
Contemporary dentistry restores missing teeth with dental implants or dentures. Dental implants, despite being the preferred treatment modality, can fail and have no ability to remodel with surrounding bone, which undergoes physiologically necessary remodelling throughout life [1]. Accordingly, there has been intensifying interest in the regeneration of orofacial tissues [2-4]. This increasing popularity of dental implant surgery has further created a heavy demand for dento-alveolar reconstruction. Insufficient alveolar contours may require bone grafting procedures to restore adequate bone volume before implant placement to counteract potentially harmful results, such as higher failure rates and unsatisfactory aesthetic results [5,6]. Recent regenerative technologies using stem cells have enhanced implant osseointegration [7,8]. Osseointegration, crucial for the success of an implant, is influenced by several factors such as treatment indication, implant material, implant surface, implant shape, treatment planning, implant surgery, and particularly by the quality and quantity of the bone.
The key problem for the placement of an oral implant is an inadequate amount of bone due to atrophy through periodontal diseases, traumata [9,10] or absorption of the jaw crest after tooth extraction or loss [11,12]. Due to the immunotolerance and the resulting bone quality, the gold standard for this procedure is still autologous bone harvested from the jaw or the iliac crest [13-18]. Bone may come from the host (autograft), a donor (allograft), or other sources such as xenograft, ceramics, and demineralized bone matrix [19]. Autologous grafts are often considered the clinical gold standard, because allografts, xenografts, and synthetic materials are associated with complications such as pathogen transmission, immune rejection, and suboptimal integration. Therefor autogenous bone graft remains the gold standard for the reconstruction of bony defects because it is the only graft material that exhibits the 4 desired properties of bone graft materials [20]:
a. osteogenesis
b. osteoinduction
c. osteoconduction and
d. osseointegration
Nevertheless, considerable drawbacks to its use have been noted [21,22]:
i) high morbidity at the donor site
ii) limited quantity of bone
iii) unpredictable quality of bone
iv) increased blood loss
v) increased operative time and
vi) donor site infection
However, these donor areas, especially the intraoral sides, are quantitatively limited; there is a higher morbidity accompanied with additional risks and complications for the patient [23]. To overcome the disadvantages of autologous bone grafts, over the last 30 years alternatives have been developed and proven to provide comparable outcomes in terms of bone quality and survival rates of oral implants placed into the grafts [24-27]. Allogeneic bone is the most commonly used alternative to the autogenous harvest [28], and the advantages of its use include convenience for the surgeon, decreased operative trauma and blood loss, absence of donor site morbidity, and greater availability of bone. Animal trials and randomized clinical studies were conducted to evaluate the benefits and disadvantages of bone substitutes available with regard to their osteoconductive properties and degradation characteristics [29-32]. Recent animal studies brought osteoconductivity in relationship with the process of dissolution in case of degradable materials [33-35]. According to degradation characteristics, grafting materials can generally be assigned to one of the following three groups: the non-degradable, slow- degradable, and fastdegradable group [36], [37].
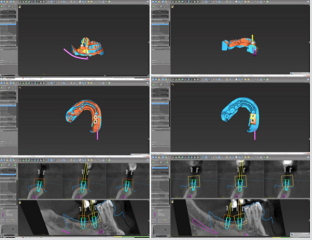
The use of allogenic bone blocks is well documented and allows a minimally-invasive approach to three-dimensional bone reconstruction. The availability of pre-operative digital cone-beam topographies allow an exact three-dimensional analysis of the defect morphology and the virtual computer-aided construction of a blockdummy, which can thereafter be transferred into the allogenic graft under sterile conditions [38]. Thus, the actual surgical procedure is reduced to the preparation of a surgical access, conditioning of the recipient bed, fixation of the graft and wound closure [39,40]. Disadvantages of allogenic bone blocks are the theoretical risk of transmitting infectious diseases, immunological aspects and the lack of osteoinductive and osteogenetic properties. By being solely osteoconductive, it must be assumed that graft incorporation and remodelling is slower and less effective compared to autogenous bone blocks, thus resulting in higher resorption rates. Since the implant shoulder is usually located at the outer surface of the grafted site, where most of the re- sorption takes place, it must be assumed, that crestal bone loss is higher in implants placed into bone grafted with allogenic blocks than in implants placed into non-augmented bone.
Besides the provenance of a bone substitute, its sequential degradation guided by osteoclasts as part of the bone remodelling is thought to be most desirable for new bone formation [41]. Bone grafts release a myriad of molecules, including growth factors, which can target stem cells involved in bone regeneration. The presence of three critical ingredients, i.e. soluble molecular signals, responding cells with associated cell-surface receptors, and assembly of the extracellular matrix have been defined as a pre-requisite in order to predictably achieve this goal [42,43]. Therefore, one of the most utilized alternative materials is the allogenic human-derived bone grafting material assigned to the slow - degradable group [44]. While bone substitute materials are routinely used, especially vertical bone augmentation of the jaws is still a problematic step. Dental stem cells in combination with bone substitute materials may accelerate the augmentation of alveolar bone and perhaps, stem cell-based therapies can become an alternative to autologous, allogenic, or synthetic bone transplants and substitutes [45,46]. However, scaffolds are required for cell delivery, and here, commercially available bone substitute materials could be an excellent source for dental tissue engineering.
The additional use of palatal-derived ecto-mesenchymal stem cell homing from the human palate, as recently published by our research group could be a future trend to induce osteogenetic processes and therefore enhance the healing capabilities in critical size defects of the jaw [47-49]. Would it be possible to heal certain facial defects by cell homing and without cell transplantation in patients? How to induce cell homing? Are autologous cells always necessary? What are the scientific and business barriers associated with cell transplantation or cell homing approaches? Here, we will find answers to some of these critical questions.
Aim
Several tissue engineering approaches have been tried to stimulate bone formation. The addition of in vitro cultured mesenchymal stem cells (MSCs) has proven to stimulate osteogenesis. Preclinical and clinical studies have demonstrated the ability of bone marrow-derived stem and progenitor cells to regenerate various tissues, including bone [50]. To bypass the problem of selection, multiplication, and differentiation, most of the mentioned studies selected MSCs, multiplied them, and then differentiated them to the osteogenic lineage. These new approaches are contributing to the progress of periimplant bone regeneration but should be further studied using controlled randomized clinical trials [51]. As this is unreasonable to do in daily practice, in this patient observation study an approach was chosen in which allogenic bone blocks will be combined with neural crestrelated stem cells (NCSCs) taken from the subepithelial tissue of the human palate.
Neural Crest-Related Stem Cells (NCSCs)
Neural crest cells that form the vertebrate head skeleton migrate and interact with the surrounding tissues to shape the skull. NCSCs can tolerate low oxygen concentrations and have the potential for osteogenic, chondrogenic, and adipogenic differentiation, depending on the external stimulus by cytokines [52]. The neural crest was first described as the ‘‘Zwischenstrang’ (German, `zwischen`: between; `Strang´: cord) by the Swiss anatomist and cardiologist Wilhelm His. He described the neural crest as a transient embryonic structure appearing between the neural tube and epidermis during avian embryonic development. After neurulation, embryonic neural crest cells (NCCs) migrate out of their niche and engender ectodermal cell types (e.g. Schwann cells, peripheral neurons, melanocytes and keratinocytes) in addition to mesenchymal cells (cranial bones, cartilage and fat cells). Due to this intrinsic potential to give rise to cells of two germ layers (ectoderm and mesoderm), NCCs possess an extraordinarily high developmental potential surpassed only by totipotent cells of the zygote and pluripotent embryonic stem cells.
Adult, tissue-resident neural crest-derived stem cells (NCSCs) were long term believed to be an in vitro phenomenon. During the last 15 years, however, an emerging line of evidence supported the hypothesis that at least a limited number of adult NCSCs may exist in the human body even in the adulthood. NCSCs can be found in different tissues and organs, especially within the craniofacial region [53-59]. Such adult human NCSCs are able to undergo selfrenewal and possess a surprisingly high differentiation potential in vitro and in vivo (reviewed in [60]). Due to their easy accessibility and high plasticity, adult NCSCs represent an ideal stem cell type for the use in bone regeneration. Concerning the marker expression, most adult human NCSC populations are characterized by the expression of the intermediate filament Nestin, the surface receptor p75NTR (CD271) and the carbohydrate HNK-1 in addition to the neural crest specific transcription factors Snail and Twist in vitro and in vivo (see [60] for a full marker list).
The purpose of this study was to evaluate the potential of Adult Palatinum as a Novel source of stem cells in combination with transplantation of Spongiosa Bone Blocks (Osteograft® , Bingen, Germany) for one-stage bone augmentation and immediate implant placement. This combination of methods for vertical augmentation in difficult anatomical sites will be tested in in a multicentric, patient observation study histologically controlled. Therefore, the aim of this patient observation study clinical-histologically controlled, was to evaluate histologically the effect of a stem cell homing approach on the amount of newly formed bone mineralization using stem cell-supported human allogen bone as carrier material in vertical augmentation with immediate implant placement.
Material and Methods
Stem Cell Homing
Stem cell-based therapy has been one of the best documented approaches in regenerative medicine including the regenerative periodontology and implantology [61], promising cures for a multitude of diseases and disorders. However, the ex vivo expansion of stem cells and their in vivo delivery are restricted by the limited availability of stem cell sources, the excessive cost of commercialization, and the anticipated difficulties of clinical translation and regulatory approval. An alternative to adoptively transferred stem cells is cell populations already present in a patient’s body, including stem/progenitor cells, which can be actively attracted to sites of injury. This technique, known as endogenous stem cell homing, has the potential to provide new therapeutic options for in situ tissue regeneration. Such options would be less costly and complex than approaches that require substantial ex vivo cell manipulation and that use artificial vehicles for cell delivery. Tissue regeneration methods that rely on endogenous stem/progenitor cell homing, local tissue responses, and functional stimulation thus offer new insights into in vivo tissue engineering and hold great promise for the future of translational medicine.
Although such methods that take advantage of the latent endogenous regenerative potential of the patient are promising for the repair of damaged tissue, they are in needs of further experimental support before application in alveolar bone regeneration procedures. The current application of endogenous ecto-mesenchymal stem cell homing in the alveolar bone for in situ guided bone (tissue) regeneration based on cell-instructive transplant and release technology to direct cell mobilization and recruitment. As a first step to addressing the limitations of stem cell delivery, we devised a cell-homing approach for vertical augmentation of alveolar bone combined with immediate placement of implants. Cell homing has been regarded as a process of exit of hematopoietic stem cells from blood vessels by transendothelization and subsequent migration. Here we broadly define cell homing as active recruitment of endogenous cells, including stem/progenitor cells, into an anatomic compartment. Cell homing offers a few advantages over cell transplantation for vertical bone augmentation in combination with immediate placement of implants:
A. Induced homing of human neural crest-related stem cells (hNCSCs) from the palate of the patients overcomes some of the key scientific, technical, commercialization, and regulatory issues associated with stem cell transplantation, such as potential contamination, excessive cost, immunorejection, pathogen transmission, and a lack of training of current clinicians to handle cells.
B. Prior instances of regulatory approval for innovative cell products.
C. Ease of clinical delivery of packaged and stored molecular delivery products.
D. Maximizes the body’s own regenerative capacity
The subepithelial connective tissue harvested from the palate of the patients was used as conduits for the homing of human neural crest-related stem cells (hNCSCs).
Innovative Therapeutic Concept
Our innovation describes a new and previously overlooked way to prepare the endogenous repairing stem cells based on their ectomesenchymal like phenotype (Molthera; PCT/EP2006/066221). In the future these exciting methods are likely to help reconcile the clinical and commercial pressures in the regenerative dental medicine (see Video).
Scaffolds
The regeneration of bone requires an adequate scaffold as well as cells that are capable to attach to the scaffold, proliferate, and differentiate. The dynamics of bone healing are controlled by growth factors, such as bone morphogenetic proteins. To promote these requirements, several strategies for bone and tissue regeneration have been developed. The discovery of stem cells and recent advances in cellular and molecular biology has led to the development of novel therapeutic strategies that aim at the regeneration of many tissues that were injured by disease. Tissue engineering is a multidisciplinary field that combines biology, engineering, and clinical science with the goal of generating new tissues and organs. It is a science based on fundamental principles that involves the identification of appropriate cells, the development of scaffolds and morphogenic signals required to induce cells to regenerate a tissue or organ. The use of allogen bone grafts with a stabilizing stem cell-containing subepithelial connective tissue graft is not limited to mature, fully mineralized bone. We decided to use in the experimental groups of this study stem cell-containing subepithelial connective tissue graft and allogenic human bone. As a carrier of our stem cell containing soft tissue from the palate, we have used sterile, high-safety (donor selection, virus testing, chemical cleaning, processing and sterilization) allograft bone product, derived of human donor bone (OsteoGraft™ block). The high biologic regeneration capability of this allogenic bone block results in a predictable clinical outcome.
Scaffolds
a) Preserved biomechanical properties
b) Sterile without antigenic effects
c) Storable at room temperature for 5 years
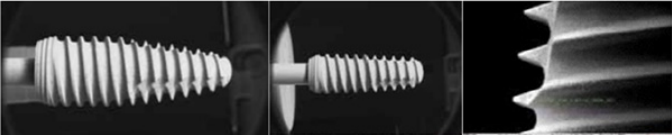
We used in the study the osteoconductive properties of the OsteoGraft™ blocks (Figure 1) supporting natural and controlled tissue remodelling.
Used Implants
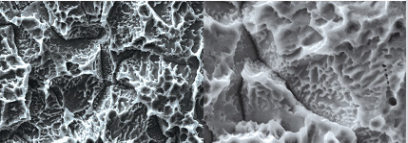
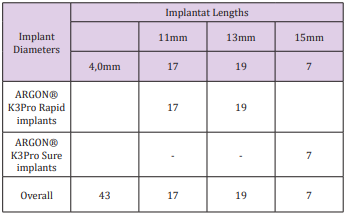
We used in the study ARGON® K3Pro Rapid and Sure implants (Figure 2 & 3), see Table 1.
General Considerations
The present study was designed as a multicentric, prospective, patient observation study at the Implant Centers, Praxisteam Hasslinghausen, Germany (WDG, MAV), at the Dental Implantology Kassel, Germany (BG), and at NAM Clinics, Bayerisch-Gmain, Germany (TF). 15 subjects (minimum age 18 years; 8 females / 7 males) were included. The mean age was 37 years (minimum: 27 years; maximum 74 years). All subjects received a pre-medication to minimize postoperative discomfort (e.g. pain, swelling or wound healing disturbances) using antibiotics (Clindamycin, 600 mg, two times a day, starting 1 day before the surgery, lasting for 5 days), and non-steroidal anti-inflammatory drugs (Ibuprofen 600 mg, one hour before the surgery, then as needed by the patient).
Protocol Specifications and Ethics Statement
This study has been approved by the ethics committee of the Zahnärztekammer Westfalen/Lippe and the University of Münster (Germany), AZ 2007-2009-f-s, 17/02/2014. The study has been conducted in accordance with the Declaration of Helsinki (Fifth Revision, 2004). Patients older than 18 years with need of dental implant placement were eligible if they had a maximum of 4 mm residual alveolar height. They had to be able to comply with studyrelated procedures, such as returning for follow-up examinations, exercising good oral hygiene, and being able to understand the nature of the proposed surgery. Written informed consent has been obtained prior to any study - related procedures. Exclusion criteria has been smoking, history, signs of malignancy, radiotherapy or chemotherapy, pregnancy or nursing, general contraindications for dental or surgical treatment, medications, treatments or diseases, which may have an effect on bone remodeling, bone or connective tissue metabolism, or an allergy to collagen. Primary parameter of the study was the new bone formation (NBF) including the histological assessment.
Patient Population
15 patients have been assessed for the study, see Figure 4.
Inclusion and Exclusion Criteria
Inclusion criteria were as follows: Subjects had to be able to understand the nature of the study and the study related procedures. Written informed consent was obtained according to international guidelines and the local law. The subjects must have been in the age of 18-75 years, systemically healthy, and in need of an augmentation to obtain a sufficient bone quantity for a proper implant placement. The subjects must have had a stable occlusal relationship with no pronounced bruxism. The augmentation sites must have been free from infection and/or extraction remnants with a radiological determined remaining bone height of approximately 4 mm ± 1 mm. Exclusion criteria were as follows: Alcohol or drug abuse as noted in patient records or in-patient history, smoking or health conditions, which did not permit a surgical procedure. Furthermore, reason to believe that the treatment might have had a negative effect on the subject’s physiological or psychological health (e.g. psychiatric problems).
Patients were excluded if they had infectious disease, heart disease or disease of the circulatory system, metabolic disease, bone metabolism disorders, disturbance of the haematopoetic system, haematological disorders, wound healing disturbances, disorders of the endocrine system (e.g. uncontrolled diabetes), local (e.g. tumors, ulcers etc.) or other contraindications for dental surgery as noted in patient records or in patient history. Furthermore, patients were not included if they were not able to give informed consent. Any disorders in the region of the prospective augmentation site such as previous tumours, chronic bone disease or previous irradiation were regarded as exclusion criteria. Female patients who were pregnant or breast feeding or female adults of reproductive potential not employing an effective method of birth control [postmenopausal state at least for 2 years, surgically sterile, hysterectomy or effective contraceptive method until placement of the final prosthetic restoration (condoms for women, diaphragm or contraceptive sponges, intrauterine device, hormonal contraception)] were excluded as well.
Sample Size Calculation
Based on reported results [62-65] it was assumed that the amount of mineralized bone in the augmented area after 3 months of healing will be 20% and after 4 months 25%. The standard deviation was set to ±12%, the alpha error to 0.05, and the power of the test to 0.80. This resulted in a minimum sample size of 15 subjects to obtain statistically reliable results. Since dropouts and withdrawals were anticipated, 20 subjects were included.
Step by Step Surgical Procedures
For experienced oral surgeons, allograft bone blocks for block augmentation are the only real alternative to harvesting patients own autogenic bone blocks, preventing well known risks as donorsite morbidity, infection risk, pain and loss in bone stability. As a carrier of our stem cell containing tissue we have used OsteoGraft™ block, a sterile, high- safety (donor selection, virus testing, chemical cleaning, processing and sterilization) allograft product, derived of human donor bone, processed by the DIZG - German Institute for Cell and Tissue Replacement, Berlin, Germany. For harvesting the stem cell-containing subepithelial connective tissue graft from the palate a horizontal incision to the bone has been made 5 mm from the palatal gingival margin and the micro- blade has been subsequently placed parallel to the long axis of the roots. Another horizontal incision has been made 2 mm coronal to the first incision and the periosteum has been dissected before removing the wedge of soft tissue.
An approximately 10×6mm subepithelial connective tissue graft (SCTG) has been harvested from the palate in the second premolar to second molar region as the source of Neural crestrelated stem cells (NCSCs). The SCTG trimmed precisely to adapt to the recipient site, see Table 2. After local anaesthesia with articaine (Ultracain® DS forte, Hoechst Marion Roussel, Frankfurt, Germany) a midcrestal incision was performed. A full-flap was prepared. Blood was collected from the wound and mixed with the bone substitute material. In case of sinus lifting a lateral window to the sinus maxillaris was prepared using a Piezotome 2™ (Acteon®) for the final steps. The Schneiderian membrane was elevated using Piezotome 2™ and a cavity for the bone substitute was created. After immediate placement of the implants together with the OsteoGraft™ block as carrier material for the stem cell-containing subepithelial connective tissue graft the mucoperiosteal flap was repositioned and closed with multiple interrupted and continuing sling sutures (Keydent PTFE Dental Suture 6-0 /Polytetrafluorethylen). The patients were seen 1, 3 and 7 days after surgery for evaluating the healing process. Seven to ten days after the surgery, the sutures were removed.
Harvesting of the Specimens
11 patients were allocated to the 3 months healing group (upper jaw subgroup) and 4 patients to the 4 months healing group (lower jaw subgroup). After the corresponding healing periods, a full-flap was prepared and the stem cell-supported allogen bone substitute or the remnants located. Hereby, the area of the bone augmentation could be clearly identified. Here, near to the implant position, the specimens were harvested using a trephine burr containing both, pristine and augmented bone.
Trephine burrs of standardized diameters were used to guarantee the removal of a specimen including the entire pristine bone and the entire augmented area.
CD 271-Based Magnetic Isolation of Human PalatalDerived NCSCs
Current clinical trials utilize neural crest-related stem cells (NCSCs) expanded in culture, however these interventions carry considerable costs and concerns pertaining to culture-induced losses of potency. This study assessed the feasibility of new clinical-grade technology to obtain uncultured NCSC isolates from human palate tissue sources based on immunomagnetic selection for CD271-positive cells. MACS MicroBeads are 50-nm superparamagnetic particles that are conjugated to highly specific antibody against the CD271 on the NCSC surface. Due to the small size, they do not activate cells and they will not saturate cell surface epitopes. CD271, also known as LNGFR (low-affinity nerve growth factor receptor) or p75NTR, belongs to the low-affinity neurotrophin receptor and the tumor necrosis factor receptor superfamily. CD271 is a well-known marker on neural crest-related stem cells.
Palatal tissues were isolated and immediately processed, under sterile conditions, with the mechanical disgregator Rigenera® system. First, the CD271+ cells are indirectly magnetically labeled with CD271 (LNGFR)-PE antibodies and Anti-PE Microbeads. Then, the cell suspension was loaded onto a MACS® Column, which is placed in the magnetic field of the MACS Separator. The magnetically labeled CD271+ cells are retained within the column. The unlabelled cells run through; this cell fraction is thus depleted of CD271+ cells. After removing the column from the magnetic field, the magnetically retained CD271+ cells were eluted as the positively selected cell fraction. The obtained suspension rich in NCSCs has been transplanted using the allogen bone carrier to the implant site, see video.
Histological Investigations
Calcified tissues, like bones, are among the most challenging tissues for histological research. However, especially with respect to dental or orthopaedic research, powerful histological techniques are necessary to study pathological conditions (standardized defect healing, and to investigate the molecular and cellular mechanisms of regeneration processes and functional recovery. The situation is even more complicated in bone regeneration research because here metallic implants or other devices made of various materials are often present, and the hard tissue-implant interface is of crucial interest in both biocompatibility and functional recovery research. After the cutting-grinding technique, embedding in technical resins is the most promising approach. Here we have been able to provide an optimized and standardized embedding and cutting technique using Technovit 9100 New. Using this technique, we have been able to perform enzyme histochemistry, and a great variety of classical histological stains. Specimens were dehydrated and embedded in methyl-methacrylate at approximately 4°C. Bigger specimens were then sectioned longitudinally in slices of 500 µm using an Exakt 310 saw and then grounded using an Exakt 400CS grinding disc to a final thickness of 50 µm. Smaller specimens were sectioned using a rotation microtome at a thickness of 5 µm. The sections were stained with Toluidin Blue.
Embedding in Methyl Methacrylate
Technovit 9100 New (Heraeus Kulzer, Wehrheim, Germany) is a polymethyl methacrylate (PMMA)-based technical resin as we described previously [66]. Briefly, the embedding procedure consists of four major steps: a Technovit 9100 New (Heraeus Kulzer, Wehrheim, Germany) is a poly methyl methacrylate (PMMA)-based technical resin that consists of several components:
a. a stabilized basic solution;
b. PMMA powder;
c. regulator;
d. hardener 1, which starts the polymerization reaction; and
e. hardener 2, which allows (in combination with hardener 1) a controlled polymerization at temperatures below 0°C. To prepare the working solutions, the basic solution must first be destabilized using a chromatography column with 50 g of aluminium oxide powder (AL3O2; particle size: 0.063-0.200 mm). The column should be filled with 1/4 glass wool and 3/4 aluminium oxide powder, leaving enough space to pour the solutions. One column filling is sufficient for 4l. The destabilization process should run continuosly and every 100 ml of destabilized solution should be stored and cooled immediately. The destabilized basic solution can be stored light protected at 4 °C for up to 4 weeks.
The embedding procedure consists of four major steps:
a) a general fixationfixation and dehydration step;
b) a pre-infiltration step;
c) an infiltration step; and
d) a polymerization steps.
The tissue blocks were sectioned at 5μm using a RM 2155 Microtome (Leica, Bensheim, Germany) using special size D carbide knives (Slee, Mainz, Germany). The preinfiltration solution consists of 1g of hardener 1 in 200 ml of destabilized basic solution. The infiltration solution consists of 250 ml of destabilized basic solution, 20 g of PMMA powder and 1 g of hardener 1. The final polymerization solution is prepared from a stock solution A (80 g of PMMA powder and 3 g of hardener 1, filled up to a final volume of 500 ml of destabilized basic solution) and a stock solution B (4 ml of hardener 2 and 2 ml of regulator, filled up to a final volume of 50 ml of destabilized basic solution). Both stock solutions can be stored at 4 °C and light protected for up to 2 weeks. Immediately before use, the cooled stock solutions A and B are mixed in the proportion 9 parts of stock solution A to 1 part of stock solution B. The polymerization process takes place at -4 °C in an adjustable temperature refrigerator. The polymerization interval is dependent on the volume of the polymerization mixture and on the consistency of the temperature at which polymerization is carried out.
Stains
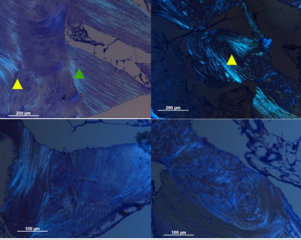
Toluidine Blue stain. For Toluidine Blue stain according to the standard procedure [67], rehydrated sections are incubated in 0.1% Toluidine Blue O (Sigma, Taufkirchen, Germany) for 20 s, washed in distilled water, dehydrated in a graded series of ethanol and mounted in Eukitt. Enzyme-based histochemical stains/Tartrateresistant acidic phosphatase (TRAP) stain. Rehydrated sections are first placed in 0.2 M acetate buffer (pH 5.0) for 20 min and then in freshly prepared TRAP staining solution containing naphthol-ASMX phosphate sodium salt as enzyme substrate and Fast Red TR salt as azo dye in 0.2 M acetate buffer (all from Sigma) for 120 min. After staining, the sections are washed in distilled water and mounted with Aquatex. Control sections are incubated in a solution that does not contain the substrate. No staining developed in these control sections. Especially for bone tissues, microscopic analysis using polarization optics (Figure 5) is an important tool to demonstrate the spatial organization of anisotropic structures like the collagen fibres in regenerating woven bone.
Figure 5: Polarization optics, Augmented area after 3 months (10 × magnification). Different orientations (arrow heads) of the collagen fibres in the cancellous periimplant bone are shown. Newly formed bone is represented by the arrow heads.
Results
Clinical Findings
Obviously, the CD271+ cell functions as a central signaling cell to local stem cells and osteoprogenitor cells in periimplant bone regeneration. The mechanism of NCSCs-supported grafts requires a complete milieu to regenerate quantities of functionally useful periimplant bone. CD271+ cell counts in a concentration of at least 5000/mL in allogen bone grafts are directly correlated to clinically successful periimplant bone regeneration. All the 15 patients show up after the immediate implant placement. The mean radiological height of the pristine bone was 4.7 ± 1.3 mm (min. 3 mm, max. 6 mm), results not shown.
Histological Findings
11 patients were allocated to the 3 months sub-group, and 4 patients to the 4 months subgroup. 15 block specimens from the experimental group were available for histological analyses. Special attention was paid to heterotopic ossifications and signs of inflammation or potential tissue rejection reaction during the descriptive evaluation. The localization of newly formed bone was also noted. Polarized light microscopy is a powerful investigative tool because it provides a wealth of information about the topology of anisotropic structures. In Figure 5 different orientations (arrow heads) of the collagen fibres in the cancellous periimplant bone are shown. Toluidine blue is very well suited for detecting cell nuclei, osteoblasts and the underlying, non-calcified osteoid regions that consist mainly of chondroitin sulfate and osteocalcin. The toluidine blue technique was used to identify osteoblasts and characterize the degree of osteoblast activity. Histological slides demonstrated new bone formation at the site of implantation at 3 months. The presence of bone lining cells and osteoide demonstrate a direct ossification, while parts of the mineralized collagen are well incorporated and still visible after 3 months.
The inset in the lower right corner shows non-calcified osteoid and osteoid-forming osteoblasts (marked with yellow arrow) at higher magnification (Figure 6). At the site of implantation, osteoblasts and osteoclasts can be observed remodelling the newly formed bone (Figure 7). No fibrous encapsulation could be observed at 3 months after implantation. A clear differentiation of the bone substitute material from mineralized bone was possible in all specimens. In both subgroups, 3 months and 4 months, the remaining particles of the bone substitute material were closely surrounded by newly formed bone. A magnification of those areas revealed specific cells generally involved in bone regenerating processes (osteocytes, osteoblasts and osteoclasts), osteoid, vessels, and collagen connective tissue. Enzyme histochemistry comes into consideration when the catabolic center of an enzyme is untouched and remains active after fixation and embedding. This is the case with regard to tartrate-resistant acid phosphatase. Tartrate-resistant acid phosphatase (Figure 8) under normal circumstances is highly expressed by activated macrophages and osteoclasts. With respect to peri-implant bone, it is a highly specific osteoclastic marker and therefore an important parameter for the qualitative and quantitative determination of bone remodelling and regeneration processes. Note especially the TRAP-positive cells in Figure 8.
Figure 6: Representative histological slide (toluidine blue staining in different magnifications) of a patient treated with NCSCs in combination with allogen bone substitute as carrier material. Augmented area after 3 months (5 × magnification). (a) Toluidin colouration. Between the stem cell-supported allogen bone substitute trabeculae of newly formed bone (arrow head) are visible. These trabeculae are surrounded by osteoblasts. The inter-particular areas are filled with connective tissue and vessels are visible. The presence of bone lining cells and osteoide demonstrate a direct ossification, while parts of the mineralized collagen are well incorporated and still visible after 3 months. The inset in the lower right corner shows noncalcified osteoid and osteoid-forming osteoblasts (marked with yellow arrow) at higher magnification.
Figure 7: Representative histological slide (toluidine blue staining in different magnifications) of a patient treated with NCSCs in combination with allogen bone substitute as carrier material. Augmented area after 3 months (5 × magnification, Toluidin coloration). At the site of implantation, osteoblasts and osteoclasts can be observed remodelling the newly formed bone. No fibrous encapsulation could be observed at 3 months after implantation. A clear differentiation of the bone substitute material from mineralized bone was possible in all specimens. The remaining particles of the bone substitute material were closely surrounded by newly formed bone. A magnification of those areas revealed specific cells generally involved in bone regenerating processes (osteocytes, osteoblasts and osteoclasts), osteoid, vessels, and collagen connective tissue.
Figure 8: Representative histological slide (Tartrate-resistant acid phosphatase staining in different magnifications) of patients treated with NCSCs in combination with allogen bone substitute as carrier material. Tartrate-resistant acid phosphatase under normal circumstances is highly expressed by activated macrophages and osteoclasts. With respect to peri-implant bone, it is a highly specific osteoclastic marker and therefore an important parameter for the qualitative and quantitative determination of bone remodelling and regeneration processes. Note especially the TRAP-positive cells.
Discussion
Stem cell homing plays an important role in tissue engineering. However, little is known about the proliferation and differentiation of paldNCSCs on different types of materials. Several recent studies showed that neural crest-related stem cells can be isolated from mammalian craniofacial tissues such as periodontal ligament, dental pulp, and palate. These cells have in common that they form neurosphere-like clusters and proliferate in serum-free culture in the presence of fibroblast growth factor-2 (FGF-2) and epidermal growth factor (EGF). From this perspective, the human palate has been shown to be of critical importance in the regenerative process. Although it is clear, that cells residing in the subepithelial soft tissues of the palate can achieve bone regeneration, this population is heterogenous, but it is not known which subpopulations can achieve regeneration. In 2007 our research group first describes the characterization and neuronal differentiation capacity of stem cells derived from inflamed periodontal tissues [55].
These so called periodontal-derived neural crest- related stem cells (pdNCSCs) were isolated by minimally invasive periodontal surgery and cultured as so-called dentaspheres under serum-free conditions in the presence of FGF-2 and EGF. Thus, we looked for a novel source of stem cells from the oral cavity being highly suited for regenerative purposes. In 2009 Widera et al. described for the first time the presence of nestin - positive neural crestrelated stem cells within Meissner corpuscles and Merkel cellneurite complexes located in the hard palate of adult Wistar rats (paldNCSCs). Characterization of NCSCs by RT-PCR and flow cytometry revealed expression of several stem cell markers, such as Nestin and Sox2 as well as STRO-1 and CD146. The paldNCSCs could be propagated as dentaspheres under serum-free conditions. Further differentiation studies proved this concept and revealed that paldNCSCs exhibit an osteogenic differentiation capacity, too. The osteogenic differentiation capacity of paldNCSCs was markedly developed suggesting that these cells might be a suitable cellular tool for bone regeneration purposes [56].
Indeed, cells derived from palate were found to have specific properties, such as increased proliferation rates, and representative of a regenerative phenotype as shown by our research group [47,56,68]. Thus, the current studies of our research group demonstrate that using a paldNCSCs-rich tissue from patients seems to be a simple and reliable method for improving the alveolar bone quality [69]. Based on the hypothesis that the number of NCSCs is secondary, the individual potential of NCSCs to survive high stress and chemotactically attract osteogenic progenitor cells will dominate. As the augmentation material is far from local blood supply, it can be assumed that a natural selection procedure will be applied to the cells (Stem Cell Homing). As blood and oxygen supply are reestablished, the NCSCs could then unfold their full potential. As we have learned from previous studies mechanical properties such as surface characteristics are decisive for a successful osteogenic differentiation of paldNCSCs [69]. Our study proposed therefore that stem cell-supported human allogen bone materials such as commercially available bone substitutes OsteoGraft™ block are superior for dental tissue engineering.
Therefore, stem cell- supported human allogen bone substitute as stem cell homing was analyzed. This clinical-histological investigation compared the amount and mineralization of newly formed bone using a stem cell-supported allogen bone substitute material in vertical augmentation after two different healing periods. It was noted that in the subgroup with sinus lifting no perforation of the Schneiderian membrane occurred during the surgery due to our piezosurgical approach. In the present study, bone tissue samples were clinically harvested using a standardized trephine burr with a diameter of 2mm. During the histological evaluations, specimens retrieved after 3 months and after 4 months of healing were compared. The influence of the healing time on the neoformation of mineralized bone was of special interest. Representative histological samples of different treatment groups are given in Figure 5. Detailed descriptive evaluation of the histological samples revealed the presence of osteoid and ‘‘bone lining cells’’ as histological characteristics of mainly direct ossification (Figure 6). Periimplant bone seemed to be less mature.
It was shown that the neoformation of mineralized bone occurred predominately around and adjacent to the stem cellsupported allogen bone substitute, which is consistent with the currently available literature [29,63,70]. Histologically, there was a close contact of the newly formed mineralized bone and the stem cell-supported allogen bone substitute in both of the subgroups (3 months and 4 months). The histological results clearly point to the previously described osteoinductive potential of the applied neural crest-related stem cells derived from the human palate [61]. Enhanced formation of unmineralized extracellular matrix and an enhanced mineral apposition rate adjacent to the degrading allogen bone scaffolds were accompanied by an increased osteoclastic bone surface, which resulted in higher bone mass and a tendency to a more mature trabecular bone structure around the allogen bone scaffolds. These results show that stem cell-supported allogen bone scaffolds induce extended peri-implant bone remodeling with a good biocompatibility.
Conclusion
Since the results of the present investigation did not show a difference in stem cell-supported allogen bone substitute using sinus lifting procedures in the upper jaw after 3 months healing and using stem cell-supported allogen bone substitute in the lower jaw after 4 months healing, it is suggested that an immediate implant placement in a stem cell-supported allogen bone substitute is clinically acceptable with sufficient primary stability. We conclude that stem cell-supported human allogen bone material are suitable for paldNC stem cell attachment and proliferation using stem cell homing. Within the frame of the present investigation, there is a lack of long-term data on the survival rates of implants and restorations in such patients. This needs to be evaluated in future studies.
References
- Friedenstein AJ, Piatetzky Shapiro II, Petrakova KV (1966) Osteogenesis in transplants of bone marrow cells. J Embryol Exp Morphol 16(3): 381- 390.
- Fellows CR, Matta C, Zakany R, Khan IM, Mobasheri A (2016) Adipose, Bone Marrow and Synovial Joint-Derived Mesenchymal Stem Cells for Cartilage Repair. Front Genet 7: 213.
- Park JS, Suryaprakash S, Lao YH, Leong KW (2015) Engineering mesenchymal stem cells for regenerative medicine and drug delivery. Methods Elsevier Inc 84: 3-16.
- Bielby R, Jones E, McGonagle D (2007) The role of mesenchymal stem cells in maintenance and repair of bone. Injury 38(Suppl 1): S26-S32.
- Giannoudis P V, Jones E, Einhorn TA (2011) Fracture healing and bone repair. Injury 42(6): 549-550.
- Loi F, Córdova LA, Pajarinen J, Lin T, Yao Z, et al. (2016) Inflammation, fracture and bone repair. Bone. Elsevier 86: 119-130.
- Tim CR, Bossini PS, Kido HW, Malavazi I, von Zeska Kress MR, et al. (2015) Effects of low-level laser therapy on the expression of osteogenic genes during the initial stages of bone healing in rats: a microarray analysis. Lasers Med Sci 30(9): 2325-2333.
- Lewandowska Łańcucka J, Fiejdasz S, Rodzik Ł, Łatkiewicz A, Nowakowska M (2015) Novel hybrid materials for preparation of bone tissue engineering scaffolds. J Mater Sci Mater Med 26(9): 231.
- Cheung RCF, Ng TB, Wong JH, Chan WY (2015) Chitosan: An update on potential biomedical and pharmaceutical applications. Mar Drugs 13(8): 5156-5186.
- Kumar RMN V, Muzzarelli RAA, Sashiwa H, Domb AJ (2004) Chitosan chemistry and phamaceutical perspective. Chem Rev 104(12):6017- 6084.
- Asthana S, Goyal P, Dhar R, KU, Pampanaboina NB, Christakiran J, et al. (2015) Evaluation extracellular matrix-chitosan composite films for wound healing application. J Mater Sci Mater Med 26(8): 220.
- Upadhyay J, Kumar A, Gupta K, Mandal M (2015) Investigation of physical and biological properties of polypyrrole nanotubes - chitosan nanocomposites. Carbohydr Polym 132: 481-489.
- Kaderli S, Boulocher C, Pillet E, Watrelot Virieux D, Rougemont AL, et al. (2015) A novel biocompatible hyaluronic acid-chitosan hybrid hydrogel for osteoarthrosis therapy. Int J Pharm 483(1-2): 158-168.
- Yan XZ, van den Beucken JJJP, Cai X, Yu N, Jansen JA, et al. (2015) Periodontal Tissue Regeneration Using Enzymatically Solidified Chitosan Hydrogels With or Without Cell Loading. Tissue Eng. Part A 21(5-6): 1066-1076.
- Azarpira MR, Shahcheraghi GH, Ayatollahi M, Geramizadeh B (2015) Tissue engineering strategy using mesenchymal stem cell-based chitosan scafolds in growth plate surgery: A preliminary study in rabbits. Orthop Traumatol Surg Res 101(5): 601-605.
- Yan XZ, Nijhuis AWG, Van Den Beucken JJJP, Both SK, Jansen JA, et al. (2014) Enzymatic control of chitosan gelation for delivery of periodontal ligament cells. Macromol Biosci 14(7): 1004-1014.
- Freier T, Koh HS, Kazazian K, Shoichet MS (2005) Controlling cell adhesion and degradation of chitosan films by N-acetylation. Biomaterials 26(29): 5872-5878.
- Masuda T, Ueno Y, Kitabatake N (2001) Sweetness and enzymatic activity of lysozyme. J Agric Food Chem 49(10): 4937-4941.
- Zhang L, Chan C (2010) Isolation and enrichment of rat mesenchymal stem cells (MSCs) and separation of single-colony derived MSCs. J Vis Exp 37: 1852.
- Tim CR, Bossini PS, Kido HW, Malavazi I, Von Zeska Kress MR, Carazzolle MF, et al. (2016) Effects of low level laser therapy on inflammatory and angiogenic gene expression during the process of bone healing: A microarray analysis. J Photochem Photobiol B Biol 154: 8-15.
- Saraiva JA, Fonseca TS, Silva GF, Sasso Cerri E, Guerreiro Tanomaru JM, Tanomaru Filho M, et al. (2018) Reduced interleukin-6 immuno expression and birefringent collagen formation indicate that MTA Plus and MTA Fillapex are biocompatible. Biomed Mater 13(3): 035002.
- Kang Q, Sun MH, Cheng H, Peng Y, Montag AG, et al. (2004) Characterization of the distinct orthotopic bone-forming activity of 14 BMPs using recombinant adenovirus-mediated gene delivery. Gene Ther 11(17): 1312-1320.
- Zhang X, Schwarz EM, Young DA, Edward Puzas J, Rosier RN, et al. (2002) Cyclooxygenase-2 regulates mesenchymal cell differentiation into the osteoblast lineage and is critically involved in bone repair. J Clin Invest 109(11): 1405-1415.
- Wlodarczyk D, Méricq JP, Soussan L, Bouyer D, Faur C (2017) Enzymatic gelation to prepare chitosan gels: Study of gelation kinetics and identification of limiting parameters for controlled gel morphology. Int J Biol Macromol 107(Pt A): 1175-1183.
- Hollinger JO, Kleinschmidt JC (1990) The Critical Size Defect as an experimental Model To Test Bone Repair Materials. J Craniofac Surg 1(1): 60-68.
- Vieira AE, Repeke CE, De Barros Ferreira S, Colavite PM, Biguetti CC, et al. (2015) Intramembranous bone healing process subsequent to tooth extraction in mice: Micro-computed tomography, histomorphometric and molecular characterization. PLoS One 10(5): 1-22.
- Jang JW, Lee JS, Jung UW, Kim CS, Cho KS (2016) In vivo evaluation of commercially available gel-type polyethylene glycol membrane for carrier of recombinant human bone morphogenetic protein-2. J Oral Maxillofac Surg 75(2): 297-313.
- Du M, Zhu T, Duan X, Ge S, Li N, et al. (2017) Acellular dermal matrix loading with bFGF achieves similar acceleration of bone regeneration to BMP-2 via differential effects on recruitment, proliferation and sustained osteodifferentiation of mesenchymal stem cells. Mater Sci Eng C Mater Biol Appl 70(Pt 1): 62-70.
- Lohmann P, Willuweit A, Neffe AT, Geisler S, Gebauer TP, Beer S, et al. (2016) Bone regeneration induced by a 3D architectured hydrogel in a rat critical-size calvarial defect. Biomaterials 113: 158-169.
- Cui J, Liang J, Wen Y, Sun X, Li T, et al. (2014) In vitro and in vivo evaluation of chitosan/β-glycerol phosphate composite membrane for guided bone regeneration. J Biomed Mater Res 102(9): 2911-2917.
- Junqueira LCU, Bignolas G, Brentani RR (1979) Picrosirius staining plus polarization microscopy, a specific method for collagen detection in tissue sections. Histochem J 11(4): 447-455.
- Takagi K, Urist MR (1982) The reaction of the dura to bone morphogenetic protein (BMP) in repair of skull defects. Ann Surg 196(1): 100-109.
- Saler M, Caliogna L, Botta L, Benazzo F, Riva F, et al. (2017) hASC and DFAT, Multipotent Stem Cells for Regenerative Medicine: A Comparison of Their Potential Differentiation In Vitro. Int. J Mol Sci 18(12): 2699.
- Tai PWL, Wu H, Van Wijnen AJ, Stein GS, Stein JL, et al. (2017) Genomewide DNase hypersensitivity, and occupancy of RUNX2 and CTCF reveal a highly dynamic gene regulome during MC3T3 pre-osteoblast differentiation. PLoS One 12: 1-23.
- Son HE, Kim EJ, Jang WG (2017) Curcumin induces osteoblast differentiation through mild-endoplasmic reticulum stress-mediated such as BMP2 on osteoblast cells. Life Sci 193: 34-39.
- Brennan Speranza TC, Conigrave AD (2015) Osteocalcin: an osteoblastderived polypeptide hormone that modulates whole body energy metabolism. Calcif Tissue Int 96(1): 1-10.
- Ferron M, Lacombe J (2014) Regulation of energy metabolism by the skeleton: Osteocalcin and beyond. Arch Biochem Biophys 561: 137-146.
- Wei J, Karsenty G (2015) An overview of the metabolic functions of osteocalcin. Rev Endocr Metab Disord 16(2): 93-98.

 Research Article
Research Article