Abstract
Type 2 Diabetes Mellitus (T2DM) is a pathological condition that is increasingly more frequent in children and adolescents. The reasons for the onset of T2DM are the increasing levels of obesity and physical inactivity, with a consequent risk of developing metabolic disorders in early adulthood and a significant economical burden on public health. In this context, as part of a multicentric study to determine the reference values of Glycosylated Hemoglobin (HbA1c) in the healthy population, we analysed 157 samples of healthy paediatric subjects to describe HbA1c trends by gender and age. Whole blood samples were collected in K2-EDTA tubes, stored at -80°C and subsequently analysed by capillary electrophoresis. There were no significant differences in children HbA1c average values according to age groups for the same gender, however we observed HbA1c average concentration was significantly higher in males than females in age group 10-14 years (p < 0.05). The results of this study probably reflect the transient change in insulin sensitivity at onset of puberty. HbA1c measurement is not sufficient for the diagnosis of diabetes mellitus, but it could help paediatricians for early detection of the disease in children, together with the Oral Glucose Tolerance Test (OGTT). The results underline a statistical significance in the paediatric age group in which the onset of diabetes mellitus is most common.
Keywords: Glycosylated Hemoglobin (HbA1c); Diabetes; Gender; Paediatric Age
Abbreviations: T2DM: Type 2 Diabetes Mellitus; HbA1c: Glycosylated Hemoglobin; BMI: Body Mass Index; AGEs: Advanced Glycation End-Products; e-GST: Erythrocyte Glutathione Transferases; HSAox: Human Serum Albumin oxidized; OGTT: Oral Glucose Tolerance Test
Introduction
Type 2 Diabetes Mellitus (T2DM) is the most common type of diabetes. It usually occurs in adulthood, but it is constantly increasing in children and adolescents [1]. In most countries, T2DM incidence has increased alongside rapid cultural and social changes: ageing of the general population, increased urbanisation, reduced levels of physical activity, wrong eating habits such as increased consumption of sugar and fatty foods and low consumption of fruit and vegetable. Together with increasing levels of obesity and physical inactivity, T2DM represents a major public health problem worldwide with a large number of pathological implications [2]. Many children with T2DM risk can develop complications in early adulthood, determining a consequent significant burden for the family and for the society. Nowadays, the data that arouses the greatest concern is represented by the account 8-45% T2DM of all new cases of diabetes are reported among children and adolescents [1]. Most often, the disease is diagnosed around the age of 13-14 years, with an earlier onset in girls, suggesting that physiological insulin resistance during puberty may play an important role in this population [1]. In this context, as a part of a multicentric study to determine the reference values of Glycosylated Hemoglobin (HbA1c) in a young healthy population [3], we analysed paediatric subjects to describe HbA1c trend by gender and age.
Materials/Patients and Methods
One hundred fifty-seven healthy subjects were referred to the Policlinico Agostino Gemelli- University Hospital for routine surveillance and on this occasion, the samples were collected. The protocol was written according to the ethical guidelines of Helsinki Declaration. All participants enrolled in the study provided signed consent (by both parent and minor), before being enrolled in the study. Exclusion criteria were: anaemia (hemoglobin <11 g/dl) [4], basal glucose values >100 mg/dl, history of type 1 and 2 diabetes in any first-degree relative (parent, sibling), and presence of hemoglobinopathies. All analyzed subjects presented Body Mass Index (BMI) comprised between 18 and 25 kg/m2 and Caucasian race. Whole blood samples, obtained by venipuncture, were collected in K2-EDTA tubes and stored at -80°C. Samples were analysed by capillary electrophoresis (Capillarys 2-FP; Sebia, Lisses, France) using the same reagents production batch. All the samples were processed in the accredited Biochemistry Laboratory of the University Hospital Tor Vergata, Rome. All data was initially entered into an Excel spreadsheet (Microsoft, Redmond, WA, USA) and the statistical analysis was performed using the Statistical Social Package for Windows, version 17.0 (SPSS, Chicago, IL, USA) and ANOVA, with the “post-hoc Bonferroni test”, was used. A value of p < 0.05 was considered statistically significant.
Results
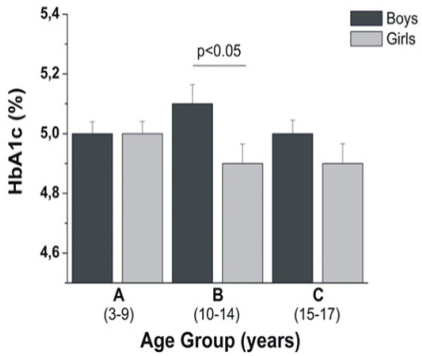
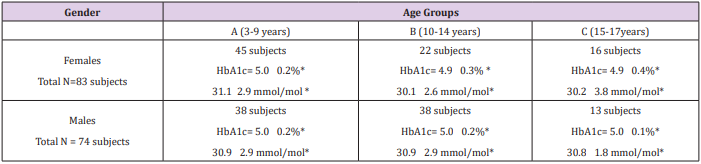
The study population has been divided into three subgroups based on age: A: 3-9 years, B: 10-14 years and C: 15-17 years. Moreover, the studied population was stratified by gender (Figure 1A). Data analysis showed in males a substantial equivalence in the average of HbA1c values in groups A (5.0 ± 0.2 %; 30.9 ± 2.9 mmol/ mol) and C (5.0 ± 0.1 %; 30.8 ± 1.8 mmol/mol), but not in the group B (5.1 ± 0.2; 31.8 ± 2.8 mmol/mol). Conversely, female showed HbA1c similar mean values, being slightly lower than the maximum value detected in the youngest group (group A, 5.0 ± 0.2 %; 31.1± 2.9 mmol/mol) with respect to group C (4.9 ± 0.4 %; 30.2 ± 3.8 mmol/ mol) and group B (4.9 ± 0.3 %; 30.1 ± 2.6 mmol/mol). There were no significant differences in HbA1c average values according to age group in the children of same gender. Furthermore, we compared the mean HbA1c values between males and females of the same age group. Finally results showed only for B group an average HbA1c concentration significantly greater in males than in females (p < 0.05; Figure 1B) (Table 1).
Figure 1: HbA1c % mean concentration, stratified by gender and age, in non-diabetic children and adolescent. Error bar represents standard error.
Table 1: HbA1c % by gender and age groups.
*Data expressed as mean standard deviation.
Note: HbA1c, Glycosylated hemoglobin; N, number
Discussion
The current American Diabetes Association recommendations suggest that HbA1c values for diabetic children are between 7.5% and 8.5% (58 and 69 mmol/mol) up to six years of age. Subsequently, with ageing, percentage values of HbA1c should be less than 8% (64 mmol/mol) in children aged 6 to 13 years and less than 7.5% (58 mmol/mol) in those aged 13 to 18 years. There are different reports that provide reference values for HbA1c among American population aged 5-24 years, who were evaluated by age, gender, race/ethnicity, education, parental history of diabetes, overweight, and glucose status [5]. The results of these studies showed that average HbA1c levels were high in group aged 10-14 years. This might reflect, the transient change in insulin sensitivity at onset of puberty. A large study determined levels of fasting serum insulin, glucose and HbA1c relating to European pre-pubertal children [6]. Our data are agree with this paper in the range age analysed (3- 11 years), while our study provided values for HbA1c distribution among individuals aged 3–17 years differentiated by age and gender also including pubertal age. Furthermore, we showed no statistical differences by gender in pediatric age, except for group B. The difference in this group (10-14 years) is probably explained by the age of menarche for females and consequently for the protective action of sexual hormones.
The average HbA1c values for each age and gender group were substantially similar, although slightly higher in males. The HbA1c mean values of girls, compared to the adult females [3] is almost constant, this finding suggests that HbA1c, during the life of women, increases only in case of pre-diabetic state and/or diabetic disease. In males, on the other hand, the mean HbA1c remains constant up to 45 years old, increasing over the years. This fact supports the evidence that the abdominal fat deposition in males is a predisposing factor in insulin resistance, with subsequent increase of HbA1c values. HbA1c measurement is not sufficient for the diagnosis of diabetes, but it could help paediatricians for early detection of the disease in children, together with the use of the Oral Glucose Tolerance Test (OGTT) [7]. In diabetic condition, it is frequent to observe an increase in oxidative stress, correlated to an increased production of Advanced Glycation End-Products (AGEs). Therefore, in a subsequent study it would be interesting to monitor the oxido-reductive state in children, by quantifying Erythrocyte Glutathione Transferases (e-GST) and Oxidized Albumin (HSAox) [8-10].
Conclusion
Our results underline a statistical significance related to gender difference in the age group, where the DMT2 onset is frequent. This work provides preliminary data that requires further study; however, it may be useful oversee the HbA1C trend in children and adolescent populations.
References
- Temneanu OR, Trandafir LM, Purcarea MR (2016) Type 2 diabetes mellitus in children and adolescents: A relatively new clinical problem within pediatric practice. J Med Life 9: 235-239.
- IDF Diabetes Atlas Group (2015) Update of mortality attributable to diabetes for the IDF Diabetes Atlas: Estimates for the year 2013. Diabetes Res Clin Pract 109: 461-465.
- Pieri M, Pignalosa S, Zenobi R, Callà C, Martino FG, et al. (2016) Reference intervals for HbA1c partitioned for gender and age: A multicenter study. Acta Diabetol 53: 1053-1056.
- World Health Organization (2011) Haemoglobin concentrations for the diagnosis of anaemia and assessment of severity. Vitamin and Mineral Nutrition Information System.
- Saaddine JB, Fagot-Campagna A, Rolka D, Narayan KM, Geiss L, et al. (2002) Distribution of HbA (1c) levels for children and young adults in the U.S.: Third national health and nutrition examination survey. Diabetes Care 25: 1326-1330.
- Peplies J, Jiménez Pavón D, Savva SC, Buck C, Günther K, et al. (2014) Percentiles of fasting serum insulin, glucose, HbA1c and HOMA-IR in pre-pubertal normal weight European children from the IDEFICS cohort. Int J Obes (Lond) 38(Suppl 2): S39-S47.
- Chilelli NC, Cosma C, Ragazzi E, Burlina S, Zaninotto M (2014) Screening with HbA1c identifies only one in two individuals with diagnosis of prediabetes at oral glucose tolerance test: Findings in a real-world Caucasian population. Acta Diabetol 51: 875-882.
- Noce A, Fabrini R, Bocedi A, Di Daniele (2015) N Erythrocyte glutathione transferase in uremic diabetic patients: additional data. Acta Diabetol 52: 813-815.
- Noce A, Fabrini R, Dessì M, Bocedi A, Santini S, et al. (2014) Erythrocyte glutathione transferase activity: a possible early biomarker for blood toxicity in uremic diabetic patients. Acta Diabetol 51: 219-224.
- Bocedi, A.; Noce, A.; Rovella, V.; Marrone, G.; Cattani, G.; Iappelli, M.; De Paolis, P.; Iaria, G.; Sforza, D.; Gallu, M., et al (2018). Erythrocyte glutathione transferase in kidney transplantation: a probe for kidney detoxification efficiency. Cell Death Dis, 9, 288.

 Short Communication
Short Communication