Abstract
Objective: This study aimed to investigate the alteration of intestinal flora before and after antibiotic therapy.
Methods: Pediatric patients admitted to the pediatric emergency center at Kitakyushu Municipal Yahata Hospital due to acute pneumonitis between April 2009 and August 2010 were enrolled. Patients treated with antibiotics were divided into two groups, butyric acid bacterium agents group and control group. Data on age, antibiotic type, duration of antibiotic therapy, occurrence of diarrhea, cultured bacteria before and after the antibiotic therapy were investigated.
Results: A total of 48 pediatric patients were included in this study, of which 26 patients were in the butyric acid bacterium agents group and 22 patients were in the control group. There was no significant change in the number of Escherichia coli (E. coli) detected in the butyric acid bacterium agents group, and the number of E. coli decreased almost to half after the antibiotic therapy. Although extended-spectrum beta-lactamase (ESBL)-producing E. coli was detected in five patients in the control group, no ESBLproducing E. coli was detected in the butyric acid bacterium agents group after the antibiotic therapy.
Conclusion: Notably, this study found that
a) ESBL-producing E. coli was present in some pediatric patients at the time of admission even before antibiotic therapy,
b) ESBL-producing E. coli may easily have appeared after antibiotic administration even for a short period,
c) Butyric acid bacterium agents administration may help patients maintain their resident intestinal flora, and
d) Butyric acid bacterium agents administration may help prevent colonization by ESBL-producing bacteria.
Keywords: Antibiotics; Pediatric Emergency, ESBL-Producing E.coli, Butyric Acid Bacterium, Pneumonitis
Abbreviations: E. coli: Escherichia coli; ESBL: Extended-Spectrum; ABPC/SBT: Ampicillin/Sulbactam; PIPC : Piperacillin; CTX: Cefotaxime; CAZ: Ceftazidime; AZT: Azacutam; CPDX-PR: Cefpodoxime Proxetil; MIC : MJinimum Inhibitory Concentration; CVA : Clavulanic Acid; ID : Identification
Introduction
Pneumonitis is an acute respiratory infection and the most common disease in pediatric patients. Although the first-line therapy for patients with moderate or severe pneumonitis is antibiotic administration, diarrhea induced by antibiotics is considered the most common adverse event. Moreover, alteration of intestinal flora is one cause of antibiotic-related diarrhea [1,2]. Although pneumonitis is one of the most common diseases treated with antibiotics, there are few reports about the effect of antibiotics on the intestinal resident flora in pediatric patients. In this prospective study, the characteristics of intestinal flora in pediatric pneumonitis patients were studied from bacterial cultures, before and after intravenous administration of antibiotics. Butyric acid bacterium agents administration may decrease the presence of diarrhea according to a few reports; hence it is speculated that this may affect the intestinal flora during antibiotic administration [3,4].
This study focused on the type of bacteria that produces extended-spectrum beta- lactamase (ESBL), which degrades the beta-lactam ring of cephem or penicillin. The beta-lactamaseproducing gene of Klebsiella pneumoniae or Escherichia coli (E. coli) degrades a wide range of antibiotics due to mutation and produces ESBL, which can degrade third- and fourth- generation cephems. Moreover, ESBL-producing bacteria are considered resistant against third- or fourth-generation cephems. Therefore, antibioticresistant bacterial infections have been a challenging problem in hospitals. Hence, this study aimed to determine whether butyric acid bacterium agents administration may help improve altered intestinal flora caused by antibiotic-related bacteria.
Methods
Patients
Pediatric patients who were admitted to the pediatric emergency center at Kitakyushu Municipal Yahata Hospital due to acute pneumonitis between April 2009 and August 2010 were included in this study.
Design
This prospective interventional study included pediatric pneumonitis patients who were treated with antibiotics such as ampicillin/sulbactam (ABPC/SBT), piperacillin (PIPC), or cefotaxime(CTX). Antibiotics were administered following the Japanese 2007 guidelines for the management of respiratory infectious disease [5].
ESBL-producing bacteria were defined based on clinical laboratory guidelines and standards. The sensitivities of ceftazidime (CAZ), CTX, azacutam (AZT), and cefpodoxime proxetil (CPDX-PR) were investigated. If the minimum inhibitory concentration (MIC) of CAZ, CTX, and AZT was more than 2, or that of CPDX-PR was more than 8, then the inhibition of bacterial growth was tested by addition of clavulanic acid (CVA). Bacteria were defined as ESBL if the MIC with CVA was 8 times lower than that without CVA. The types of antibiotics were decided based on the last digit of the patient’s identification (ID) number.
The administration of butyric acid bacterium agents was also decided based on the last digit of the patient’s ID number. All patients were administered butyric acid bacterium agents from the first day of admission. The duration of antibiotic administration was 5 to 7 days, which was dependent on the patient’s condition or the results of the blood test and chest X-ray. Butyric acid bacterium agents had been continued during antibiotic administration. Patients were divided into two groups: those with butyric acid bacterium agents administration (butyric acid bacterium agents group) and those without butyric acid bacterium agents administration (control group). After every meal during the course of the antibiotic therapy, 1.0 g/day of butyric acid bacterium agents was given to the patients in butyric acid bacterium agents group. Fecal cultures were obtained before and after the antibiotic therapy. Data on age, antibiotic type, duration of antibiotic therapy, occurrence of diarrhea, cultured bacteria, and ESBL-producing bacteria before and after the antibiotic therapy were recorded. Diarrhea occurring after antibiotic administration was defined as diarrhea related to antibiotic administration. Data were analyzed by Fischer’s exact test. Values of p<0.05 were considered significant between groups. The parents of the enrolled patients provided informed and written consent. This study was approved by the ethical board of Kitakyushu Municipal Yahata Hospital (approval no. 30-025). All procedures were performed in accordance with the Declaration of Helsinki.
Results
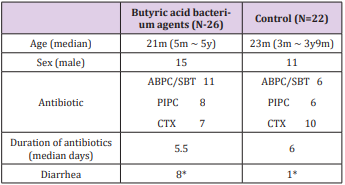
Over 4,000 pediatric patients are admitted to our hospital annually. A total of 48 pediatric patients whose parents provided informed consent were included in this study, of which 26 patients were in the butyric acid bacterium agents group and 22 patients were in the control group. Patient characteristics are shown in Table 1. The median age was 21 and 23 months in the butyric acid bacterium agents and control groups, respectively. The patients’ ages ranged from 3 months to 5 years. There were 15 and 11 male patients were in the butyric acid bacterium agents and control group, respectively. There was no significant difference in age or sex between the groups. Eleven patients were treated with SBT/ABPC, 8 patients were treated with PIPC, and 7 patients were treated with CTX in the butyric acid bacterium agents group. Six patients were treated with SBT/ABPC, 6 patients were treated with PIPC, and 10 patients were treated with CTX in the control group. The median duration of antibiotic administration was 5.5 days in the butyric acid bacterium agents group and 6 days in the control group.
Table 1: Characteristics of patients.
*P<0.05
ABPC/SBT; ampicillin/sulbactam, PIPC; piperacillin, CTX; cefotaxime
There was no significant difference in type of antibiotic and administration duration in the two groups. Eight patients in the butyric acid bacterium agents group and 1 patient in the control group suffered from antibiotic-related diarrhea. The details of the cultured bacteria are shown in Table 2. Resident flora such as Enterococcus spp. was detected in all patients before and after the antibiotic therapy. Before antibiotic therapy, E. coli was detected in 21 and 19 patients from the butyric acid bacterium agents and control groups, respectively. Although there was almost no remarkable change in the number of E. coli detected in the butyric acid bacterium agents group, the number of E. coli decreased almost to half after the antibiotic therapy. ESBL-producing E. coli was detected in 1 patient in the butyric acid bacterium agents group and in 2 patients in the control group before antibiotic therapy. Although ESBL-producing E. coli was detected in 5 patients in the control group, no ESBL-producing E. coli was detected in the butyric acid bacterium agents group after the antibiotic therapy. There was no significant difference between the two groups in the number of ESBL-producing E. coli after antibiotic therapy. The number of patients with antibiotic-related diarrhea was greater in the butyric acid bacterium agents group, but there was no remarkable relationship between ESBL-producing E. coli and antibiotic-related diarrhea.
Table 2: Results of fecal culture.
E. coli; Escherichia coli, ESBL; extemded-spectrum beta-lactamase
Discussion
This study aimed to determine whether butyric acid bacterium agents administration might help to improve altered intestinal flora after antibiotic administration. After the intervention, resident flora disappeared and their growth was inhibited by high concentrations of antibiotics secreted in the saliva, bile, or intestinal mucosa due to intravenous administration of antibiotics. The inhibition of resident flora increases antibiotic-resistant bacteria or pathogenic bacteria by absorbing the nutrition from the intestinal mucosa. This is considered the cause of diarrhea related to antibiotic use or sepsis. ESBL-producing E. coli was detected in 3 patients before administration of antibiotics at admission. Antibiotics are easily prescribed at the home clinic, which is thought to be related to colonization by ESBL-producing bacteria [6] Gooch et al. [7]. reported an incidence of antibiotic-related diarrhea of 8-30%. [7] In our pediatric emergency center, the incidence of diarrhea was 15.6%, which was not different from previous reports. Tiana et al. [8] compared respiratory infectious diseases in children treated with antibiotics and Lactobacillus agents and those who were not.
They reported that the number of antibiotic-related diarrhea was decreased by one third after Lactobacillus agents administration [3]. Kurata et al. [4] studied pediatric patients treated with antibiotics and butyric acid bacterium agents or antibiotics alone. They also reported that the rate of antibiotic-related diarrhea was decreased by one third in the butyric acid bacterium agents group [4]. In our study, the number of patients who suffered antibioticrelated diarrhea in the butyric acid bacterium agents group was higher than that in the control group. Although the number of E. coli remained within the normal range and that of ESBL-producing E. coli did not increase in the butyric acid bacterium agents group (Table 2), the reason for the increase in patients with diarrhea is unclear. Additional study is needed to reveal the relationship between intestinal flora and diarrhea. The number of normal E. coli decreased, but the number of ESBL-producing E. coli increased in the control group.
On the contrary, the number of normal E. coli was not decreased remarkably, and no ESBL-producing E. coli was detected in the butyric acid bacterium agents group after antibiotic therapy. Takahashi et al. [8] reported that the intestinal flora of patients with irritable bowel syndrome consisted of more Clostridium and less Lactobacillus compared with that of healthy adults [8]. In addition, butyric acid bacterium administration improved the intestinal flora of patients with irritable bowel syndrome and made it similar to that of healthy adults. From the previous reports, administration of butyric acid bacterium agents with antibiotic can be considered effective. There are some limitations to this study. First, the number of patients was very small, and the effect of differences in the antibiotic type could not be studied. Additionally, there was no data as to whether antibiotics were administered or not at the home clinic before admission; hence, it was difficult to accurately predict the condition of intestinal flora.
Conclusion
Notably, this study found that
a) ESBL-producing E. coli was present in some pediatric patients at the time of admission even before antibiotic therapy,
b) ESBL-producing E. coli may easily have appeared after antibiotic administration even for a short period,
c) Butyric acid bacterium agents administration may help patients maintain their resident intestinal flora, and
d) Butyric acid bacterium agents administration may help prevent colonization by ESBL-producing bacteria. Further study is needed on the current status of antibiotic administration at clinics and the type, dose, and duration of butyric acid bacterium agents administration.
Acknowledgement
T.I contributed to the literature search, study design, data collection, data analysis, data interpretation, and writing. J.K supervised the data analysis and data interpretation, and contributed critical revision.
References
- Nord CE, Kager L, Hemdahl A (1984) Impact of antimicrobial agents on the gastrointestinal microflora and the risk of infections. Am J Med 76(5): 99-106.
- Hooker KD, Dipiro JT (1988) Effect of antimicrobial therapy on bowel flora. Clin Pharm 7(12): 878-888.
- Arvola T, Laiho K, Torkkeli S, Mykkånen H, Salminen S, et al. (1999) Prophylactic Lactobacillus GG reduces antibiotic-associated diarrhea in children with respiratory infections: a randomized study. Pediatrics 104 (5): e64.
- Kurata S, Taki Y, Inoue K (1988) Preventive effect of butyric acid bacterium agents for diarrhea induced by antibiotic. Jpn J Pediatr 41(10): 211-216.
- Uehara S (2006) Japanese guidelines for the management of respiratory infectious diseases in children 2007. Jpn J Pediatr Pulmonol 17 (2): 184- 185.
- Yoshida H, Kusakari A, Takeuchi H (2009) The survey of using antibiotic to upper respiratory infection in outpatients at children’s clinic. J Ambul Gen Pediatr 12(1): 2-9.
- Gooch III WM, Blair E, Puopolo A, Paster RZ, Schwartz RH, et al. (1996) Effectiveness of five days of therapy with cefuroxime axetil suspension for treatment of acute otitis media. Pediatr Infect Dis J 15 (2): 157-164.
- Takahashi M, Cho T, Tho T (2001) Comparison of intestinal flora between irritable bowel syndrome patients and healthy adults and improvement by butyric acid bacterium agents. Jpn J Soc Clin Stud Intestinal Microflora 3(1): 45-47.

 Research Article
Research Article