Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
Seyed Kianoosh Naghibzadeh1, Hossein Lanjanian2, Bita Shalbafan3,4*, Fatemeh Abdi4 and Maryam S Daneshpour5*
Received: January 09, 2023; Published: January 24, 2023
*Corresponding author: Bita Shalbafan, Iranian Social Security Organization, Clinical Research Development Center of Labbafinejad Hospital, Shahid Beheshti University of Medical Sciences, Tehran, Iran Address: 9th Boostan, Pasdaran St. Tehran, Iran
Maryam S Daneshpour, Cellular, and Molecular Endocrine Research Center, Research Institute for Endocrine Sciences, Shahid Beheshti University of Medical Sciences, Tehran, Iran
DOI: 10.26717/BJSTR.2023.48.007623
COVID-19 threat is unlikely to fade soon since Global vaccination, as the best solution, is not being quickly realized. Thus, pre-exposure prophylaxis would be an available alternative strategy. This longitudinal retrospective study was done on 7696 patients referred to an Iranian hospital in the south of Tehran. The PCR result for COVID-19 and history of medications were gathered from the hospital HIS system. We investigated the possible chemoprophylaxis of the routinely recommend drugs for atherosclerosis risk control. Whit the aim of extracting the association of the pre-exposure drug history and COVID-19 history, the logistic regression model was used by adjusting for age, sex, and drug history six months before and after the pandemic. A total of 7696 individuals (12- 97 yrs), 3272 men (63±14 yrs), and 4424 women (62±13.4 yrs) were studied. Among them, 581(7%) with the COVID-19 infection; 575(7%) with a hospitalization history in 6 months before the pandemic; 5809(75%) with hypertension; 2428(32%) with Ischemic Heart Disease; 2323(30%) with diabetes mellitus; 2068(26%) on metformin; 4132(54%) on Atorvastatin; 4852(62%) on Aspirin; 3907(50%) on ARBs; 638 (8%) on ACEIs; multivariable regression analysis demonstrated the strong association between pre-exposure ASA or Atorvastatin consumption and hospitalization rate due to COVID-19 as an infection severity index. Moreover, COVID-19 hospitalization rates were decreased in female hypertensive cases with ARB in their drug histories. In hypertensive subjects, comorbidity of diabetes mellitus and HTN increase the COVID-19 hospitalization rate in men by 2 .930. Someone at risk of COVID-19 infection should control their blood pressure and hyperglycemia precisely, and not only strict BP and BS control but also, Aspirin and Atorvastatin as chemoprophylaxis is highly recommended. Even the overprotection and increasing self-care during an illness may also affect the exposure to the infection.
Keywords: COVID-19; Chemoprophylaxis; Aspirin; Atorvastatin; Arbs; Aceis; Hypertension; Diabetes Mellitus; Iran
Abbreviations: HTN: Hypertension; ACEIs: Angiotensin-Converting Enzyme Inhibitors; RAS: Renin-Angiotensin-Aldosterone System; SSIA: Social Security Insurance Agency; HIS: Hospital Information-System
The COVID-19 pandemic is a threat to human health worldwide, and in the current scenario, there is no specific drug against it; hence, repurposing of drugs is the best solution to the urgent need for safe and available treatments. According to recent evidence, mortality from COVID-19 has been associated with multiple organ failure, particularly cardiovascular and pulmonary dysfunction [1], and occurs mainly among middle-aged and elderly patients who suffered from pre-existing diseases such as hypertension (HTN), diabetes mellitus, and cardiovascular diseases [2]. HTN is one of the risk factors influencing the mortality and morbidity of the COVID-19. The inflammatory response evoked by COVID-19 may be exacerbated by the renin-angiotensin-aldosterone system [3]. On the other hand, in the pandemic, Hypertensive patients who controlled their blood pressure by angiotensin II receptor blockers (ARBs) have a better outcome in his hospitality date [4]. Angiotensin-converting enzyme inhibitors (ACEIs) and ARBs are among the agents inhibiting the renin-angiotensin-aldosterone system (RAS) and are prescribed to manage HTN in a large proportion of the patients. Although there has been a controversy over the continued ACEIs and ARBs medication in the setting of COVID-19 since using ACEIs and ARBs has been shown to increase expression of ACE2 receptor, the cellular receptor and entry point of SARS-COV-2, in animal studies. On the contrary, downregulation of ACE2 expression following SARS infection has been shown, which resulted in activation of RAS and progression of pneumonia. Thus, using ACEIs and ARBs may also be advantageous through blocking HTN of RAS due to ACE2 downregulation; hence, inhibiting acute pulmonary injury. Therefore, no sufficient clinical data indicate the positive or negative association between using ACEIs and ARBs in patients with COVID-19 [5].
Acetylsalicylic acid or Aspirin as a non-steroidal anti-inflammatory drug has anti-inflammatory, antithrombotic, and analgesic effects and inhibits the aggregation of platelets. Aspirin by irreversible inactivation of cyclooxygenase 1 (COX-1) inhibits thrombotic damage and also hinders thrombus formation. Aspirin reduces deep vein thrombosis (DVT) by inhibiting P-selectin. Furthermore, long-term low-dose Aspirin has been effective in preventing ischemic cardiovascular and cerebrovascular events [6]. TNFα and other inflammatory adipocytes, which increase in the presence of obesity and type 2 diabetes, will be decreased by metformin. These anti-inflammatory properties are through autophagy activating, triggering CD8 memory T cells, and M2 macrophages converting. The antioxidant activities of metformin can potentially help manage inflammatory responses occurring with COVID-19. The studies showed taking this drug could be associated with lower mortality for sepsis in patients suffering from pulmonary diseases, which suggests a potential beneficial effect in COVID-19 patients [7]. Statins are the biggest group in hyperlipidemia control have a promising association on COVID-19 patients by leading to higher expression of ACE2 [8]. Protection against coronary endothelial dysfunction due to COVID-19 has been suggested as the potential advantage for statin treatment [9]. There is a need for wellstructured clinical studies to clarify the controversies over using Aspirin, metformin, statins, and anti-hypertensive drugs in COVID-19 Infection severity. This longitudinal retrospective study was designed on regularly using drugs to investigate their association with the COVID-19 hospitalization.
In the current study, we included the patients admitted to Ayatollah Kashani Hospital (AKH) under the Iran Social Security Insurance Agency (SSIA) coverage in the south of Tehran. SSIA keeps the complete patients’ medication history, including prescription, medical history, and drug history, in the regular visits. This retrospective study was run in the AK hospital between Sep2019– Aug 2020. All procedures were under the ethics committee’s ethical standards on human subject research at Shahid Beheshti University of Medical Sciences (IR.SBMU.RETECH.REC.1399.576; 12. Oct.2020). We confirm that all procedures are performed in accordance with the relevant instructions. In this hospital, the patients’ follow-up was easy because it is a well-known and unique SSIA center in the south of Tehran that health cares are free of charge for Social Security Insured patients; also, it is not a referral or educational, medical center. Besides, SSIA has robust and reliable hospital informationsystem (HIS) software. This HIS creates a trustable databank that allows us to follow and revise in-patients and out-patients and medical and health care documents and informs us of the list of drugs obtaining from pharmacies in Tehran. Aforementioned, AKH HIS registered drug histories included in-patients and out-patients in the mentioned period were followed-up in the present study. According to the current study’s documentation, the patients with a positive drug history of atherosclerosis risk factors control were selected and classified according to (Table 1).
Atherosclerosis risk factors consist of HTN, ischemic heart disease, diabetes mellitus, hyperlipidemia, and hypercoagulability state. Finally, a comparison between six months before and after the COVID-19 pandemic hospitalization rate was made to investigate the relation of COVID-19 hospitalization and the history of Metformin, Atorvastatin, Gemfibrozil, ASA, ARB, ACEIs, and other antihypertensive drugs. We defined hospitalization labels in cases that stayed at least two successive nights in the hospital. The calculation of patients’ length of stays in the HIS system is based on date and not hours, so we exclude some patients admitted at midnight and are discharged at 6:00 AM of the next day due to normal CBC, CRP, and Lung CT Scan. Since the respiratory intensive care equipment (ICU) had been distributed in all hospital wards, we did not consider ICU ward admissions days as the severity index. If necessary, out-patient records and medication descriptions at the time of hospitalization, written twice in the nurse and physician admission report, are reviewed. Suppose there was any doubt about the final fate, the hospital secretory contact patient’s family. We labeled the patients who control their hyperglycemia only by oral anti-hyperglycemic agents like Metformin and (or) Glibenclamide as DM_o group and who use insulin (regular and/or NPH products) as DM_i group.
Statistical Analysis
Hospitalization was considered as a dependent dichotomous variable in this analysis. Blood pressure control drugs are limited to hypertensive people; besides, recent hospitalization is a risk factor for COVID-19 hospitalization; moreover, there is different COVOID-19 hospitalization rate between two sex; thus, at first, the association of pandemic hospitalization rate with hypertensive medication, hospitalization history, and sex was evaluated in a univariate method, independently. Consequently, all the analysis processes were done separately in four separated groups base on sex and hypertension history. The odds ratio with the 95% confidence interval was used to present hospitalization chance in each clinical subgroup. In the multivariable analysis, a hierarchical forward logistic regression analysis was used. Aging, hospitalization history, diabetes mellitus, and ischemic heart disease were inserted in the model as a block of the confounder variables. Another block containing the other drugs (Metformin, Atorvastatin, Gemfibrozil, ASA, and ARB, ACEIs, and other anti-HTN in hypertensive groups) was inserted forward likelihood ration base variable selection method in the analyzed model. The analysis was done with IBM SPSS version 26 (IBM SPSS Inc., Chicago, Ill.). A P-value less than 0.05 was considered a significant level.
The dug lists of 7696 individuals between 12-97 years old (%42 men 63±14; women 62±13.4) were examined six months before and after the start point (Sep2019-Feb2020; March 2020 – Aug 2020). Numbers and presents of diabetes mellitus (DM_o and DM_i), the incidence of ischemic heart disease, hyperlipidemia, and hypercoagulability state cases besides CVID-19 infection status were presented in the two groups of hypertensive and non-hypertensive subjects, (Table 2). According to (Table 3), HTN and sex have a statistically significant association with the COVID-19 hospitalization rate. In univariable analysis, pre-exposure Aspirin consumption showed a significant association with COVID-19 hospitalization in all groups; while, no significant association was observed in Atorvastatin groups (Table 4). A hierarchical forward logistic regression as the multivariable analysis model evaluated COVID-19 hospitalization association with ARB, ACEIs, other anti-hypertensive drugs, Atorvastatin, Gemfibrozil, ASA, and Metformin consider while aging, hospitalization history, diabetes mellitus, and ischemic heart disease, considered confounder variables (Table 5). Interestingly, Aspirin and Atorvastatin showed a significant protective association with COVID-19 hospitalization only in non-HTN groups. Moreover, ARBs have a statistically significant protective association with the COVID-19 hospitalization in the female-HTN group. DM_i medication in the male-HTN group has the COVID-19 hospitalization odd ratio of 2.93; nevertheless, DM_i medication in the female Non-HTN group has the COVID-19 hospitalization odd ratio of 6.57 with a marginal significance.
Table 3: Univariate analysis results of the association of the main risk factors with the COVID-19 hospitalization
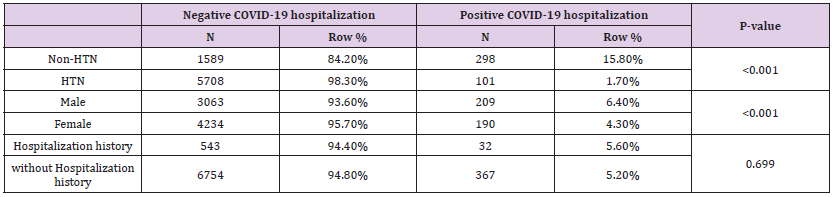
Table 4: Univariate analysis results of the association between risk factors and the COVID-19 hospitalization for both sex in HTN and non-HTN groups.
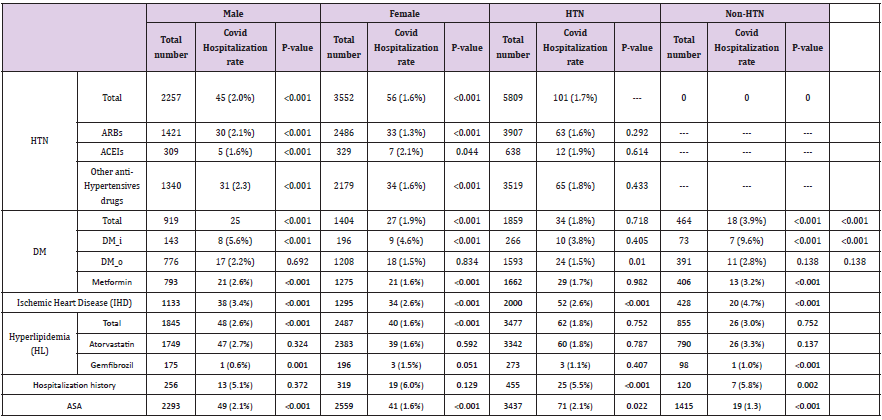
Table 5: Multivariable analysis results of the association between drug history and the COVID-19 hospitalization rate in both sex in non-hypertensive and hypertensive groups.
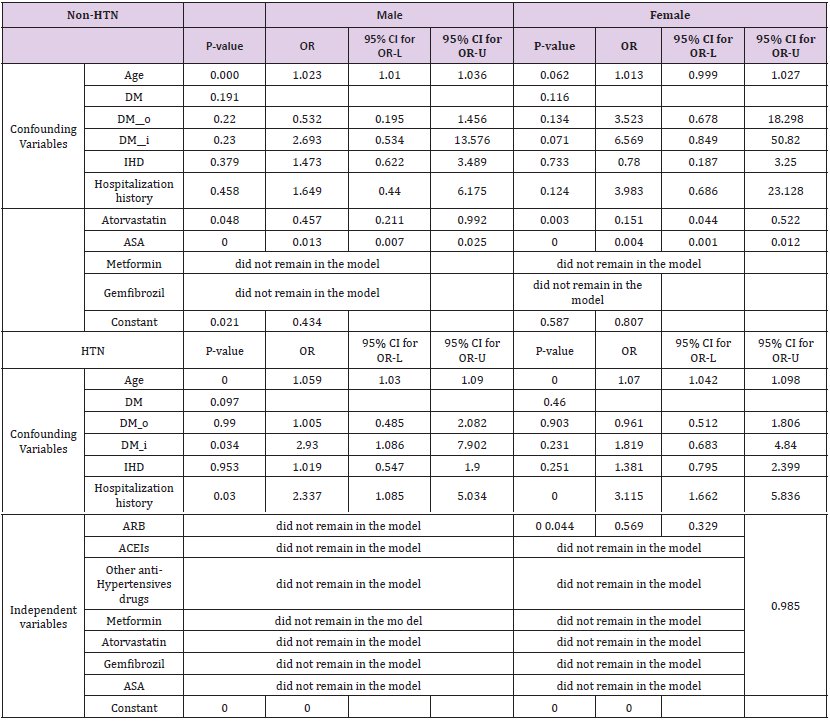
Hospitalization rate as the COVID-19 infection severity index was evaluated in this study. Our finding demonstrated that Aspirin and Atorvastatin had a negative association with COVID-19 hospitalization in non-hypertensive patients to COVID-19 hospitalization. Also, ARBs showed a negative association with COVID-19 hospitalization in the female HTN- group to COVID-19 hospitalization rate too. DM_i statistical findings are different; in female-non HTN groups has an incremental pattern, but the male-HTN group has decremented pattern in the COVID-19 hospitalization rate in comparison to before the COVID-19 pandemic. Hospitalization time has a substantial social and financial pressure on the medical system during a pandemic; thus, evaluating the association between hospitalization rate and drug history has an important priority. Our primary concern in the present study was to propose chemoprophylaxis as a solution to reduce this time. According to our results, the COVID-19 hospitalization rate in non-hypertensive male and female groups who took Aspirin reduced by 0.013 and 0.004, respectively. These findings indicate the negative association of Aspirin only on the non-hypertensive groups. However, some previous studies and clinical trials did not agree upon Aspirin’s effects during the pandemic. Aliae et al. recommended the early use of Aspirin in COVID-19 patients, although they emphasize the urgent need for clinical trials in this area [10]. In a retrospective observational study, antiplatelet medications did not affect the disease outcome [11]. Recruited 52 cases with low-dose Aspirin and 131 cases without Aspirin prescription in Tongji Hospital in Wuhan, showed no difference in in-hospital mortality between the Aspirin and non-aspirin groups.
Pre-hospitalization taking of low-dose Aspirin was not associated with the clinical outcome of COVID-19 infections in patients hospitalized with CAD [6]. It worth mentioning that our results demonstrate a strong association between pre-exposure to Aspirin and the COVID-19 hospitalization only in non-HTN cases. Simultaneously, the other studies had focused on the HTN groups, or there is considerable ambiguity about the HTN in their considered population. Also, our results are in agreement with the pre-exposure prophylactic effect of Atorvastatin in non-hypertensive cases. There are odd ratios of 0.457 and 0.151 in males and females with a statistically significant association with COVID-19 hospitalization in Atorvastatin positive drug history group against negative ones. Except for the hyperlipidemia role, Statins have several well-known effects like anti-inflammation, antithrombotic, and immunomodulation. So, they may mitigate endothelial dysfunction and dysregulated inflammation in COVID-19 infection [12]. A significant association between taking the statin and reducing mortality in patients with COVID19 was not observed by (Peymani, et al [13]). A statistically significant inverse relationship between typical COVID-19 symptoms self-reported by the participants and self-reported statin therapy also has been reported by a total of 3654 individuals in Lower Saxony, Germany, who participated in an online symptom-tracking survey [14]. In a Meta-analysis, some opposite findings favored the efficiency of statin reduction in DM-o patients by 30% and discredited the suggestion of harms using statins in COVID-19 patients [15]. It worth mentioning that we omitted the hyperlipidemia from the confounder variable list since, unexpectedly, this variable showed a statistically significant protective association with COVID-19 hospitalization (data not shown).
We believe this result was rooted in that almost all hyperlipidemia patients have Atorvastatin or Gemfibrozil medication; therefore, we put away hyperlipidemia from the model and observed the protective association of Atorvastatin and COVID-19 hospitalization. Thus, we should be careful of disease side effects and the off-label effects of prescriptive drugs to control them. Similarly, in a population of 71 consecutive patients with a pre-existing chronic cardiovascular disease, suffer from COVID-19, statins have significantly reduced the risk of mortality of the COVID-19 [16]. Again, we argue that in our results, a strong protective association between the preexposure of Aspirin and COVID-19 hospitalization only in nonhypertensive cases was detected; while focusing on the patients with cardiovascular disease or cases with an ambiguous history of HTN is the main limitations of previous studies. However, we only found an association with the ARBs and reduced COVID-19 hospitalization rate in the hypertensive-female group. These findings support by previous reports about sex dependency in ARBs efficacy in male hypertensive cases [17]. A survey on the clinical outcomes during COVID-19 showed that hospitalization mortality rates for hypertensive cases on ACEI or ARB, ACEI, and ARB were 26.7%,32.7%, and 30.6%, respectively [18]. In another study on the drug interactions with COVID-19 treatments, results do not support stopping treatment with ACEI and ARBs in well-controlled patients with mild (Stage 1) HTN and COVID-19 infection [19].
In a retrospective observational study, a higher risk of infection in the groups with ACEIs or ARBs medication history was not confirmed [20], and the same results were reported by (Aleksova, et al. [21]). Lanza et al. argued that RAS inhibitors increase ACE2 expression in hypertensive patients and recommend their use as a COVID-19 therapeutic [22,23]. We emphasize that our model had been adjusted for different confounders. Therefore, we argue that the previous reports on a higher rate of hospitalization in HTN cases on ARBs or ACEIs may not be related to the off-label effects of the drugs and can be due to the disease side effects or even the medical care due to HTN or diabetes mellitus. COVID-19 infection is mediated by binding the viral spike protein to the human ACE2 receptor, following the spike protein’s activation TMPRSS2 [24] where ACE2 is a vital element of the HTN pathophysiology. On the other hand, due to COVID-19 infection, the immune system’s dysregulation results in a cytokine storm [25]. ACE2 levels are regulated directly by cytokines [26]; thus, the decrease in ACE2 levels can be preceded by a viral infection and indicate the immune and inflammatory responses against the infected tissues [25]. The immune system task is to tackle any foreign organisms’ invasion after injury. However, this action comes at the cost of collateral damage when the immune system overreacts to internal injuries, such as pre-existing HTN [27]. Wang et al. observed an association between HTN and survival rate [28], and Grasselli et al. reported HTN as the most common comorbidity observed with COVID-19 [29]. Our data’s remarkable result is that HTN per se increases the hospitalization rate in the COVID-19 pandemic.
Immune responses underlie fatality rates, or severity of COVID-19 infection outcomes is sex-dependent [30,31]. Regarding this evidence supported by our results presented in Tables 3 & 4 to more evaluate the sex and HTN association with COVID-19 hospitalization, the second analytic plan was designed to divide total cases into crossed subgroups based on sex HTN in PMH. In a report from 5700 patients hospitalized with COVID-19 in the New York City area, the most common comorbidities were hypertension (56.6%), obesity (41.7%), and diabetes mellitus (33.8%) [18]. In the other study, pre-existing hypertension, cardiovascular disease, stroke, diabetes mellitus, chronic kidney disease, heart failure, lung disease, or obesity predispose to increased COVID-19 mortality [32]. As aforementioned, we consider diabetes mellitus as a block of the confounder variables. On the other hand, we divided the diabetic people into two groups. However, the univariant analysis showed a significant association between DM and COVID-19 hospitalization; according to the multivariable analysis results presented in Table 5, we only observed significant results for the DM_i in the hypertensive male case as a risk factor with a p-value of 0.034 the hazard ratio was 2.930. Here, we did not find any association between the DM_o group with the COVID-19 hospitalization. Although recent discussions point out that oral hypoglycemic agents such as Sodium- Glucose-Transporter-2 inhibitors (SGLT-2i), Glucagon-Like-Peptide-1 Receptor Agonists (GLP-1RAs), Pioglitazone, and even insulin might be harmful to COVID-19 individuals with diabetes mellitus, limited evidence is available on metformin for the same [33]. In the other study, including 104 patients in the metformin and 179 patients in the no-metformin group, Hyperglycemia control by metformin was associated with decreased mortality [34].
There are several significant strengths to this study to note. We considered each group’s history of medication, including the hospitalization rates before the pandemic, and compared the. COVID_19 hospitalization rates with the hospitalization history rate. We had access to the suspected peoples’ PCR-test results; these help us build a reliable statistical model. However, this study’s limitations were the selective studied cohort that includes the insurance people south of the Tehran region that mainly belong to a specific socioeconomic class with the same nutrition regime. Thus there may be unknown confounders and or habits that affect the results.
Moreover, limitations in the population size and imbalance between the different clinical groups make it easy to generalize results easily. Another limitation was the unavailability of biochemical laboratory findings, so we could not define which indication causes Atorvastatin’s prescription for patients. It is the reason for ignoring the hyperlipidemia in our study. Also, no strong supports in review articles pushed us to ignore the hyperlipidemia effect on COVID-19 infection severity.
We propose that a balance between blood pressure control and RAS inhibitors. Therefore, it is essential to optimize blood pressure control in hypertensive patients and carefully monitor cardiovascular and other complications in the COVID-19 infection period. Moreover, the comorbidity of DM_i and HTN significantly increases the risk of hospitalization due to covid-19 infection severity. Taking Aspirin or Atorvastatin has a possible chemoprophylactic effect in nonhypertensive patients in the pre-exposure phase. For the ARBs, only a sex association in the female hypertensive cases was observed. Finally, we should be careful of disease side effects and the off-label effects of prescriptive drugs to control them. Furthermore, overprotection and increasing health care during an epidemic may also affect the exposure to the infection. Thus, there should be molecular mechanism studies besides the clinical trials on the chemoprophylaxis effects of Aspirin, Atorvastatin, blood pressure control, and anti-hyperglycemic agents.
Funding
There was no funding for this study.
Declarations of interest
None.
Ethics Approval and Consent to Participate
All procedures were under the ethics committee’s ethical standards on human subject research at Shahid Beheshti University of Medical Sciences (IR.SBMU.RETECH.REC.1399.576; 12. Oct.2020). The Social Security Patient Support Committee has given us access to information and they have supervised the data collection process. Of course, this information did not contain the identities of the individuals, and each person was identified by a unique code. Since, we did not do any interventions in the treatment process of individuals and only the database and registered documents were used, there is no need for consent. We confirm that all procedures are performed in accordance with the relevant instructions.
Submission Declaration and Verification
We declare that this manuscript is original, has not been published before, and is not currently being considered for publication elsewhere.
Acknowledgment
We wish to thank Tehran Social Security Insurance Agency for deep cooperation in data access from HIS system, especially Mr. Alireza Shahraki, for reliable data gathering. We also thank Dr. Mandana Mohyeddin Bonab and Dr. Vahideh Nasr for this idea and Dr. M.M. Naghizade for statistical consults. Finally, we appreciate the Research Institute for Endocrine Sciences, Shahid Beheshti University of Medical Sciences, for its support.


