Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
Saeed Taj Din1* and Maria Shabbir2
Received: Navember 01, 2022; Published: November 09, 2022
*Corresponding author: Saeed Taj Din, Associate Professor Orthopaedic surgery Azra Naheed Medical College Lahore, Pakistan
DOI: 10.26717/BJSTR.2022.47.007446
Background: Physiotherapeutic interventions are important part of coordinated treatment. Patients who are in ICU for prolong period they face cognitive, psychological, physical and functional problems. ICU survivors do receive rehabilitation. Physical therapy increase morbidity and decrease mortality in mechanical ventilated patients.
Objective: Aim of this study is to find out protocols used in ICU by physiotherapists.
Method: This was descriptive cross-sectional study. 100 physiotherapists were included in this study through convenient sampling technique from ICU of different hospitals in Pakistan. Study was completed in 6 months. Frequency tables, mean and standard deviations were used to analyses data.
Result: In cardiopulmonary conditions, respiratory muscle training is main treatment of choice. In neurological conditions NMES, sitting, standing and walking is treatment of choice in ICU protocol. In orthopedic conditions standing and walking are treatment of choice.
Conclusion: Most useful and common protocols are concluded through this study.
Keywords: Physiotherapy; Chest Physiotherapy; ICU; Intensive Care Unit
Physiotherapeutic interventions are important part of coordinated treatment. The aim of these interventions is to prevent impairments, medical complications and risk and to restore the selected aspects of functioning [1]. Weakness, immobility and deconditioning are common problems in mechanically ventilated patients who admitted in hospital for prolong period of time. Physical therapy may address these problems and beneficial if initiated early during intensive care unit (ICU) stay. Physical therapy practice in the ICU setting varies greatly from one setting to another. ICU’s physical therapy is part of usual care but delivery situation of physical therapy is often infrequent and irregularly [2]. Patients who are in ICU for prolong period they face cognitive, psychological, physical and functional problems. ICU survivors do receive rehabilitation.[3] Physical therapy decreases morbidity and mortality in mechanical ventilated patients [4]. The main physical therapy goal for hospitalization patients in ICU is to reduce the length of stay, mechanical ventilation, and pulmonary infection [5]. Muscular weakness develops during the ICU stay due to mechanical ventilation. Early mobilization of critically ill patients prevents muscular weakness and improve function [6]. Previous researches were conducted to find out effects and implementation of physical therapy protocols that reduced postoperative pain. This study will find out protocols of physiotherapy in ICU patients.
The decrease in functional performance, exercise capacity and quality of life in ICU survivors explains the need for rehabilitation during ICU stay. It is important to prevent or attenuate muscle de-conditioning as early as possible in patients with an expected prolonged bed rest. Recent scientific and clinical interest and evidence have given support for a safe and early physical activity and mobilization approach towards the critically ill patient by ICU team members. Despite the evidence, rehabilitation in ICUs is usually inadequate while better organized in weaning centers or respiratory intensive care units. The major reason is that the approach in rehabilitation is less driven by medical diagnosis and lack of focusing on deficiencies in the broader scope of health problems as defined in the International Classification of Functioning, Disability and Health. This classification helps to identify problems and use of interventions accordingly at the level of impairments of body structure (anatomical parts of the body, such as organs, limbs and their components) and body function (physiologic functions of body systems including psychological functions) as well as activity limitations (difficulties in performing physical activities) and participation restrictions (problems an individual may experience in involvement in daily life events). Physical activity and exercise should be performed with appropriate intensity and with appropriate exercise modality.
The risk of moving a critically ill patient is weighed against the risk of immobility and recumbence and requires stringent monitoring to ensure safety. Acutely ill, uncooperative patients will be treated with modalities such as passive range of motion, muscle stretching, splinting, body positioning, passive cycling with a bed cycle or electrical muscle stimulation that will not need cooperation of the patient and will put minimal stress on the cardiorespiratory system. On the other hand, the stable and cooperative patient beyond the acute illness phase but still on mechanical ventilation, will be mobilized on the edge of the bed, transferred to a chair, allowed to perform resistance muscle training or active cycling with a bed cycle or chair cycle and walk with or without assistance. Physiotherapists are involved in the prevention and treatment of de-conditioning and respiratory conditions in critically ill patients. Their role varies across units, hospitals, and countries and is appreciated by medical directors as well as patients. Physiotherapy assessment of critically ill patients is directed by impairment at a physiological and functional level and less by the medical diagnosis. Accurate and valid assessment of respiratory conditions, de-conditioning and related problems are of paramount importance for physiotherapists. In addition, physiotherapists can contribute to the patient’s overall well-being by providing emotional support with enhancing communication.
The objective of this research was to identify physical therapy protocols in ICU patients.
Clinical decision making in ICU and rational management of patients is based on a tripod approach:
1. A knowledge of underlying pathophysiology and basis for general care
2. Scientific evidence and physiological treatment interventions
3. Clinical experience.
Effective clinical decision making and practice in the ICU demands specialized expertise and skills including advance and current knowledge in cardiopulmonary, multisystem physiology, pathophysiology and in surgical, nursing and pharmacological management. Physical therapists in ICU need to be first rate diagnosticians. Given the multitude of factors that contribute to impaired oxygen transport the therapist must able to analyzes these to define patients specific oxygen transport deficits and problems. Therefore, the ICU therapists must be capable of integrating large amount of objective information quickly, interpreting this information and integrating it to provide basis for treatment prescription. The integration of vast amount of multi organ system data is perhaps the single most important skill in ICU practice and treatment prescription. With this database the therapist must identify the indication for treatment and optimal timing of interventions. The condition of ICU patient can change rapidly; the therapist must work within narrow windows of opportunity to achieve an optimal treatment response. The goals of physiotherapy are to optimize oxygen transport, enhance mucous clearance that improves ventilation-perfusion matching, increase lung volumes, and reduce work of breathing [7]. The therapeutic goal is frequently focused on the prevention of secondary damage such as pneumonia or contractures, promotion of consciousness and sensory perception and strengthening of the muscles. The overall aim is to achieve the highest possible degree of mobility and independence with regard to self-care [8] Physical Therapy treatments in the ICU are judiciously selected in goal specific manner. General guideline treatment descend in a physiological hierarchy, mobilization, exercise and body positioning should be exploited first with respect to their direct and potent effects on oxygen transport by using conventional interventions such as manual techniques. Mobilization and exercise can be prescribed to effect three physiologically distinct outcomes based on their long-term effects, and their preventative effects. The treatment prescription needs to focus on specific effects of mobilization and exercises requthe in reversing or mitigating deficits in oxygen transport. The treatment protocols are different in each case and change frequently. The frequency depends on patient specific treatment goals. The aggressiveness of treatment depends on patient cooperation and tolerance. The patient oxygen reversed capacity needs to assessed to ensure that the patient can meet the demands of exercise stress. Objective and subjective measures of the patient’s tolerance to initial assessment and the observation of other members of the team help to establish this baseline. The purpose of this study was to assess the frequency of physical therapy, site of initiation of physical therapy, and patient outcomes comparing respiratory failure patients who received usual care compared with patients who received physical therapy from a Mobility Team using the mobility protocol [1]. The period of stay in the intensive care unit (ICU) often entails prolonged bed rest and can be devastating, leading to significant loss of functional ability. Patients who require prolonged mechanical ventilation are prone to high morbidity rates, high costs of care, and poor functional outcomes [9].
The role of physiotherapists in ICU, as stated by Stiller, is positioning, percussion, vibration, manual hyperinflation, coughing, tracheal suctioning, and breathing and limb exercises. The benefits of early mobilization include reductions in length of stay in the ICU and hospital, as well as improvements in strength and functional status. Early PT led rehabilitation of the critically ill patient has the potential to dramatically influence recovery and functional outcomes in this vulnerable patient group [10]. The treatment mainly consisted of airway clearance and graded mobilization. Airway clearance intervention included breathing exercises, bronchial drainage techniques, coughing, and incentive spirometry. Active- assisted and active joint movements were implemented both in bed and in the sitting position on the edge of the bed. The level of mobilization was set according to patient’s tolerance each day. Mobilization was graded as sitting in bed, sitting on the edge of the bed, standing and pre-ambulatory exercises and ambulation. Each physical therapy session included airway clearance intervention followed by exercises and mobilization [11]. Within the service of physiotherapy specifically, the drive to have treatments and interventions rooted in evidence-based practices is growing. However, as stated by Stiller and Wiles, patient satisfaction has been investigated for selected subgroups, but is still under-utilized within the intensive care unit (ICU) setting. Much of ICU-based research is focused on improving critical care management to increase survival and to reduce the long-term effects of ICU stay [12].
There is increasing evidence demonstrating that early progressive mobilization of patients in the intensive care unit (ICU) is safe, with a low rate of adverse events and beneficial in terms of its positive effect on patients’ functional ability and its potential to reduce ICU and hospital length of stay. Despite this evidence, barriers to the mobilization of ICU patients have been identified which have the potential to decrease the uptake of research findings into clinical practice. These barriers include patient-related factors such as cardiovascular, respiratory and/or neurological disability, level of consciousness, pain/discomfort and the site of vascular/other invasive lines. These barriers to the mobilization of ICU patients were predominantly identified from data reported in clinical studies or staff surveys investigating broad mobilization/rehabilitation practices in the ICU [13]. A new clinical specialist physiotherapist post was created, with a focus on improving rehabilitation within critical care. The appointed individual devised the QI intervention, which involved the creation of a critical care physiotherapy subteam with a focus on rehabilitation, a senior physiotherapist obtained from the Queen Elizabeth Hospital Birmingham charity [14]. The efficacy of ‘chest physiotherapy’ on short-term patient physiological outcomes has been studied extensively and there is moderate-to-strong evidence in support of its role. The safety of physiotherapy treatment in ICU has also recently been established. In addition, there is growing evidence for the role of exercise rehabilitation beginning in ICU and extending to beyond ICU discharge. Urgent research is required by physiotherapists to establish the effectiveness of such treatments [15]. Physical therapy practice in the ICU setting varies greatly from one setting to another [6]. One reason for the observed variability in the delivery of physical therapy to ICU patients may be the lack of a uniform protocolled approach for ICU delivery of physical therapy. Such protocols exist for other ICU interventions: weaning from mechanical ventilation, liberation from sedation, and early goal directed therapies for severe sepsis [7].
A self-structured tool was used to collect the data about physiotherapy protocols used by physiotherapists in ICU. Validity of the tool was checked by taking approval from 10 senior Physiotherapists. Data collection tool was filled by physiotherapists. Consent was taken from physiotherapists. And tool was given to the physiotherapists with detailed discussion about aim of the study.
Study Design
The study was a descriptive cross sectional study.
Setting
Intensive Care Unit departments of major hospitals nationally.
Study Population
Male and female physiotherapists working in Intensive Care Unit.
Duration of Study
The study took 6 months.
The sample size was calculated by using following formula and parameters:
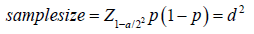
Htm
Z, - Is standard normal sulfate (at 3’ié ttj›e 1
ertnr{P<0.05} lt k 1.96 and at l°.i o, 1errortP<0.01)
It Is 2.58). As in zna|orit¿ of studies P Jues aic
considered slgrdAcuic below 0.03 hen¢c 1.96 Is used
p - Exjiectcd proportion In population based on pztvtous studies or pilot studies.
d - Absolute ezzor or piectsien - I-lxs to be decided &’nsczrchr
Z=l.96
P=0.595%
D=0.05
As prevalence of Physiotherapists in ICU is very low i.e. 0.005%, minimum sample size calculated was 100 i.e. 20 from each province of Pakistan.
Convenient sampling technique was used for study.
Inclusion Criteria
Male and female physiotherapists working in ICU.
Exclusion Criteria
1. Not willing to participate.
2. Neglected or unaware of physiotherapy services in ICU.
An informed consent was taken first from hospital’s higher management after that from Physiotherapists working in ICU. The data from the Physiotherapists was collected with the help of’ questionnaire mentioning protocols used for patients admitted in ICU.
The ethical committee of hospitals approved to conduct the study in their hospitals. We took informed consents from participants and ensured confidentiality. All ethical issue taken into account during research.
The data was analyzed through SPSS v21. Qualitative variables were shown as frequencies and quantitative variables were studied as mean and standard deviations.
Majority of the physiotherapists working in ICU were male 85%. It has been seen that in majority of cases part time physiotherapy services has been deployed in ICU 72%. Exact ICU protocols have not been found in majority of cases (68%). In cardiopulmonary conditions it has found that majority of the physiotherapists used respiratory muscle training 100%, joint range of motion 96%, sitting 95%, standing 92%, walking 91%. But NMES and cycle ergometer has used less i.e. 3% and 8% respectively. In neurological conditions, majority of physiotherapists uses joint range of motion 98%, sitting position 97%, standing position 96%, and respiratory muscle training 100%, walking practice 98% and NMES by 97%. Very least physiotherapistsuse cycle ergometer 4%. In orthopedic conditions majority of therapists use joint range of motion 100%, sitting position 100%, standing and waling also 100%, NMES 95%. Respiratory muscle training and cycle ergometer is used by 4% and 3% respectively. In other conditions for which patients are admitted in ICU, majority of physiotherapists use joint range of motion 84%, sitting by 44%, standing 50%, respiratory muscle training 45%, walking 38%, NMES 25% and cycle ergometer 23%.
In cardiopulmonary conditions, respiratory muscle training is main treatment of choice. In neurological conditions NMES, sitting, standing and walking is treatment of choice in Intensive Care Unit protocol. In orthopedic conditions standing and walking are treatment of choice.
Goal of physiotherapy treatment in cardiopulmonary patients in ICU is to enhance perfusion through respiratory training. Similar results were found in previous study where physiotherapy in ICU met the goals of optimizing oxygen saturation, enhancing mucociliary clearance that improved ventilation-perfusion ratio, increase in lung volumes and reduce work of breathing [7]. In neurological and orthopedic conditions joint range of motion, sitting, standing and walking prevents contracture, improves mobility, prevent joint stiffness and maintains muscle strength. Moreover improvement on consciousness and sensory perception and strengthening of the muscles overall achieve the highest possible degree of mobility and independence with regard to self-care [8]. Physiotherapy protocols improve functional capacity of the patient and decrease the hospital stay time. Patients who require prolonged mechanical ventilation are prone to high morbidity rates, high costs of care, and poor functional outcomes. Physiotherapy in ICU will encounter these problems [9]. Change of position from sitting to standing and walking enhance the functional level of the patient. The role of physiotherapists in ICU, as stated by Stiller was in positioning, percussion, vibration, manual hyperinflation, coughing, tracheal suctioning, deep breathing and limb exercises. The benefits of early mobilization include reductions in length of stay in the ICU and hospital as well as improvements in strength and functional status. Early PT led rehabilitation of the critically ill patient has the potential to dramatically influence recovery and functional outcomes in this vulnerable patient group [10].
In orthopedic conditions early mobilizations including siting, standing and waking is very important. It is encouraged by physiotherapists and orthopedics both. There is increasing evidence demonstrating that early progressive mobilization of patients in the intensive care unit (ICU) is safe, with a low rate of adverse events, and beneficial in terms of its positive effect on patients’ functional ability and its potential to reduce ICU and hospital length of stay. Despite these evidence, barriers to the mobilization of ICU patients have been identified which have the potential to decrease the uptake of research findings into clinical practice. These barriers include patient-related factors such as cardiovascular, respiratory and/or neurological instability, level of consciousness, pain/discomfort, and the site of vascular/other invasive lines. These barriers to the mobilization of ICU patients were predominantly identified from data reported in clinical studies or staff surveys investigating broad mobilization/rehabilitation practices in the ICU [13]. Cycle ergometer has been found to be discoiimged by our findings. It might be reason that cycle ergometer is easily available in ICU of the hospitals. Our study has found very strong evidence of use of respiratory muscle training and chest physiotherapy in cardiopulmonary conditions and other conditions as well. The efficacy of ‘chest physiotherapy’ on short-term patient physiological outcomes has been studied extensively and there is moderate-to-strong evidence in support of its role. In addition, there is growing evidence for the role of exercise rehabilitation beginning in ICU and extending to beyond ICU discharge. Urgent research is required by physiotherapists to establish the effectiveness of such treatments [l5].
Certain limitations were faced during the course of the study.
1. Due to limited time follow up of the patients was of only 6 months.
2. Random Sampling technique could not be used.
3. All types of ICU patients could not be included.
It is declared that no funding taken for this study. There was no ethical issue.
Participants identity secured throughout the study.
There was no conflict of interest.


