Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
Budi Santoso* and Khusnul Khotimah
Received: October 13, 2022; Published: October 26, 2022
*Corresponding author: Budi Santoso, Research Center for Safety, Metrology, and Nuclear Quality Technology, National Research and Innovation Agency, Puspiptek Serpong Region, Indonesia.
DOI: 10.26717/BJSTR.2022.46.007407
In vivo and in-vitro specialist and medical service activities that use open radioactive sources require enumeration facilities for radiation protection equipment in control areas. At this time, the regulation is limited to the mandate of the head of BAPETEN Regulation No. 17 of 2012 concerning Radiation Safety in Nuclear Medicine. Article 35 explains only the implementation of the obligation to provide radiation protection equipment. It does not mention the requirements for counting radionuclides or radiopharmaceutical methods. Therefore, this research needs analysis regulation which requires the counting system method using the miles and Huberman qualitative methodology by reducing the presentation of data from other sources, SNI IEC/ TR 61948-1:2014 Regarding Radiation Counting Systems. The results show that the counting system method for measuring radionuclides in vivo in SNI IEC/TR 61948- 1:2014 includes energy calibration, sensitivity checks, initial window settings (presets), energy resolution, counting precision, background, and routine frequency tests. So, this regulation has completed the method of counting radiation systems for nuclear medicine instrumentation.
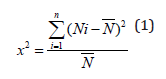
The counting loss of the radioactive test source determined by the count rate performance measurement in the acceptance test shall not exceed 5%. This provision refers to the calculation of radionuclides in the chi-square formula. The counting precision set n observations of count values (Ni) in a given time interval and average value (N) can be calculated. For each Ni measurement and constant time interval set, about 10.000 counts should be collected. The count should not exceed 10%. For 10 measurements, the chi-square value should be 3,3 ≤ 𝑋2 ≤ 16,9.
Keywords: Requirements, Test, Measuring, Protection
Nuclear medical radiation is in the form of energy emitted by atoms in the form of particles or waves used in the medical world, both for diagnostic and treatment (therapy) purposes. Radiation receives at any time, both from nature and not nature. Some radiations are beneficial or have a positive impact, but harmful or hurt the human body, animals, and plants. We cannot detect radiation directly with the five senses but use special equipment called radiation detectors, such as photographic film, Geiger Muller tubes (Geiger Muller counter), and scintillation counters. The recording results from interpreted as radiation energy absorbed by the whole body or tissues [1,2,3]. The amount of ionizing radiation energy absorbed by the body is the absorbed dose expressed in Gray (Gy) and for smaller units in milli Gray (mGy). The same dose for each type of radiation does not necessarily have the same biological effect because each ionizing radiation has a different ability to damage tissues or organs of the human body.
Because of this difference, an independent dose of the type of radiation, namely the equivalent dose in Sievert (Sv) units and millisieverts (mSv) for smaller units. The equivalent dose is the absorbed dose times the radiation weight factor. The radiation weight factor for electrons (beta radiation), photons (gamma), and X-rays is 1, while for alpha radiation it is 20. This means that alpha radiation can cause damage to body tissues 20 times greater than beta, gamma, and radiation. X-ray. With this equivalent dose, a 1 Sv dose from alpha radiation will cause the same damage as a 1 Sv dose from beta, gamma, and X-ray radiation [1,4,5,6] Radiation protection is part of the actions taken to minimize radiation exposure from the damaging effects of radiation. Each implementer of nuclear activities is required to apply for radiation protection, including in nuclear medicine, and is responsible for facilitating radiation protection activities, including the principles of radiation protection, radiation protection against occupational exposure, and radiation protection against medical exposure. Radiation protection requirements include justification, dose limitation, and application of optimization of radiation protection and safety [7]
However, the regulation availability still valid is the Regulation of the Head of Bapeten Number 17 of 2012 concerning Radiation Safety in Nuclear Medicine. In Article 35 paragraph [1]: The License Holder must ensure that the Dose Limit Value as referred to in Article 32 paragraph [8] is not exceeded, by a. performing the division of work areas; b. monitoring Radiation Exposure and radioactive contamination in the work area; c. monitoring the dose received by radiation workers; and d. conduct environmental radioactivity monitoring as well as paragraph [2] states The license holder in carrying out the obligations as referred to in paragraph [1] must provide radiation protection equipment. The regulation only mentions providing radiation protection equipment and divi sion of work areas. Not yet mentioned requirements for the method of counting radionuclides or radiopharmaceuticals as part of the control area. Such conditions need to be adapted to the needs of the implementation and development of science and technology in the radiation protection counting system. The radiation counting system is part of nuclear medicine instrumentation which is used to measure radionuclides in vivo and in vitro without imaging in the working area, which is divided into the control area and supervision area [9]. The control area includes the preparation, counting, and storage room for radionuclides and radiopharmaceuticals. Therefore, it is necessary to analyze the regulation of the radiation counting system method for nuclear medicine instrumentation to complete the radiation protection requirements that are not yet contained in the regulations that are already available in the Regulation of the Head of Bapeten Number 17 of 2012.
This study uses a qualitative method of inductive techniques by collecting supporting documents and compiling theory construction or comparing theory with other theories with Miles and Hubermann analysis, including the data collection process, reducing large, heterogeneous, and very complex data that needs to be organized in an in the form of a neat and detailed report (data reduction), data that has undergone reduction is reported in the form of systematic brief descriptions, tables, diagrams and narrative texts (data display), with such a presentation, a descriptive interpretation or a more detailed description is carried out. clear about the object of research (conclusion and verification) [10] Figure1.
Collecting data from the materials used in the form of secondary documents, namely SNI IEC/TR 61948-1:2014 Concerning Nuclear Medicine Instrumentation-Routine Testing-Part 1: Radiation Counting System4. This standard describes the test methods of counting instruments for measuring radionuclides in vivo and in vitro without imaging. Activity meters (dose calibrators) are excluded. The equation used is the chi-square equation.
The counting system was divided into in-vivo and in-vitro. In-vivo is an instrument designed to directly measure the activity of radioactive substances in the body. In-vitro is an instrument designed to estimate the activity of radioactive substances in samples [11,12,13]. From the data information obtained in SNI IEC/TR 61948-1:2014 Concerning Nuclear Medicine Instrumentation-Routine Test-Part 1: Radiation Counting Systems, routine test data includes tests with and without radioactive sources. If a radioactive test source is used, the count loss determined by the measurement of the performance of the count rate in the acceptance test shall not exceed 5%, unless otherwise stated to produce information on the counting system requirements [4] including:
Energy Calibration
The energy calibration procedure establishes the relationship between the pulse height analyzer (dial reading) window setting and photon energy. As part of the energy calibration, a reference point must be set on the energy scale. A radionuclide with photon energy suitable for the energy range used must be selected. The pulse height analyzer dial reading will be set to a value corresponding to the photon energy. Using a small window less than the photopeak FWHM, the high voltage and/or gain is varied until the maximum count level is observed. To determine/check the stability of the energy calibration over the entire energy range, the centerline of the photon peaks (photopeak) of radionuclides with different photon energies is determined. Keeping a narrow window, high voltage, and the same gain, a reading to observe the maximum count rate is determined, using at least three radionuclides with different photon energies covering the desired energy range.
Sensitivity Test
The sensitivity should be checked with reference sources containing long-lived radionuclides at appropriate photon energies. The measurement geometry and functional arrangement of the instrument must be defined and stated.
Initial Setting Window (Preset)
Inspection of the correction function from the initial setting window, radionuclides should be measured, first by the start of the appropriate window setting and secondly by the appropriate manual setting (window dial). Ideally, the count rate should be the same.
Energy Resolution
Determining the full width of the photon peak at half maximum (FWHM), the pulse height spectrum can be obtained by measuring the count rates at different dial readings using a narrow window. The energy window width should not exceed 1/5 the FWHM
Counting Precision
In the counting precision test, the chi-square test should be used. For a set of n observations of count values (Ni) in a given time interval, the average value (N) can be calculated. For each Ni measurement and constant time interval set, approximately 10,000 counts must be collected. The count should not exceed 10%. The chi-square value can be calculated using the chi-square equation (1) in the method used so that for 10 measurements, the chi-square value should be 3.3≤𝑋2 16.9
Background
Backgrounds must be specified for each commonly used energy and window setting.
Routine Test Frequency
Routine test frequency includes background and sensitivity tests with daily frequency, energy calibration tests, energy resolution, count precision and presets for windows with a frequency of twice a year.
The counting system method for measuring radionuclides in-vivo and in-vitro in SNI IEC/TR 61948-1:2014 About Nuclear Medicine Instrumentation-Routine Test-Part 1: Radiation Counting System contains energy calibration, sensitivity check, initial window settings (presets), energy resolution, counting precision, background, and test frequency routine. Finally, it can complement the counting radiation instrumentation method for nuclear medicine, which has not been in the Regulation of the Head of Bapeten Number 17 of 2012 concerning Radiation Safety in Nuclear Medicine.


