ABSTRACT
Background: Adhesive capsulitis is the common issue in overall population. AC causes musculoskeletal disorders of the shoulder, which is a typical justification for loss of function and disability in patients and the greatest common features of AC are pain accompanying with progressive stiffness and lack of shoulder external rotation actions and loss of variable movement may also be present, sticking to the site of the maximally affected capsule. Objective: To compare the effects of Active release technique and Muscles energy technique on pain, ROM and functional disability in subacute adhesive capsulitis patients with trigger points. Methodology: A randomized clinical trial using a convenient sampling technique, the sample size of 74 with 37 in each group was selected and then divided into two groups, Group A received an active release technique and Group B received a muscle energy technique (37 ART and 37 METs). NPRS and SPADI were used as outcome measures to assess pain, range of motion, and functional disability in adhesive capsulitis with trigger points and data were collected at baseline and week 4 and follow-up at week 6 and the period was 9 months, and the age group was 40-60yrs taken into account for both men and women. Conclusion: The result of this study shows that both techniques are effective, but ART is more effective than METs in improving the pain, range of motion, and functional disability.
Keywords: Active Release Technique; Muscle Energy Technique; Adhesive Capsulitis; Trigger Points
Introduction
The shoulder is anatomically and functionally confused as it is one of the largest unrestrictedly mobile regions in the human body due to articulation at the glenohumeral joint. It carries the shoulder girdle, which unites the upper extremity to the axial skeleton via the sternoclavicular joint. The considerable variety of movement of the shoulder is at the expense of compact stability of the joint and its long-term hazard of dislocation and injury [1]. The shoulder joint, also as the glenohumeral joint, is a ball and socket joint with the greatest significant range of motion in the human body. Shoulder muscle tissue has a variety of characteristics, along with abduction, adduction, flexion, extension, internal and external rotation [2]. The primary muscle groups that maintain the shoulder joint is the rotator cuff muscle tissue. The four muscle tissues of the rotator cuff are the supraspinatus, infraspinatus, teres minor, and subscapularis. The muscle tissue of the rotator cuff connects anteriorly to the proximal humerus at the superior tubercle. The muscle mass of the rotator cuff provides extensive structural guidance for the glenohumeral joint and holds the humeral head in place by articulating with the scapula in the glenoid cavity [3]. The subscapularis arises from the subscapular fossa of the scapula and attaches to the lesser tuberosity in addition to part of the anterior shoulder joint. A large bursa separates the muscle from the neck of the scapula. The features of the subscapularis are achieved through internal rotation and abduction of the humerus [4].
The trapezius is a huge, triangular shaped muscle that lies at the back of the shoulder. The trapezius arises from the advanced element of the neckline within the occipital, cervical, and upper chest regions and enclosures on the lateral aspect of the clavicle, acromion, and spine of the scapula. The characteristic of the trapezius is both raising and raising the shoulder depending on whether the upper or lower muscle fibers are activated [5]. Shoulder function is a compromise between mobility and balance. Its great mobility is mainly due to the shape of the glenohumeral joint and the simultaneous movement of all segments of the shoulder girdle [6]. The shoulder is an extremely complex joint that is vital to many sports of daily life. The limited mobility of the shoulder is a serious scientific finding. An inclusive decline in shoulder range of motion is termed adhesive capsulitis, in reference to the actual attachment of the shoulder capsule to the humeral head. The three grades of this condition described are the pain level, the sticking level and the healing level Complaints of shoulder pain or movement problems are difficult to assess. Many shoulder disorders share similar signs, causes, triggering factors, and treatments. a few pathologic lesions can be found in a single joint [7]. Bivariate analyzes confirmed that diabetes, hypothyroidism, decreased body weight, decreased body mass index (BMI), and positive personal family history of idiopathic adhesive capsulitis were all hazard factors for idiopathic adhesive capsulitis [8]. 8-12 months study duration; we found that DM and associated hyperlipidemia were autonomic risk factors for AC. The risks are higher for older women. The results of the current study help to identify speculative patient groups to train for initial avoidance of AC and improve complete caution of first-class patients with DM [9]. Shoulder disorders, which include rotator cuff disease, adhesive capsulitis, glenohumeral OA, and other situations involving instability and humeral head fractures, affect a large percentage of the general population, with an expected factor incidence of 7 to 26%. Not uncommon assessments of people with shoulder problems consist of pain that can lead to problems performing everyday activities, which include dressing and bathing [10].
Detection of coracohumeral ligament thickening on noncontrast magnetic resonance imaging provides good accuracy for adhesive capsulitis, despite the fact that imaging is not required for prognosis. In general, adhesive capsulitis was thought to progress from a tough stage to a healing period lasting one to two years with comprehensive assessment of indicators and no therapy [11]. MRI can be used to illustration feature findings in diagnosing AC. Thickening of the CHL and capsule in the rotator cuff interval and complete abolition of the fat triangle below the coracoid incision proved to be the maximum characteristic MR findings visible with AC [12]. The Kinect can be used to measure shoulder ROM based on its distance using goniometric measurements and has become clinically relevant in diagnosing AC [13]. Adhesive capsulitis clinically presents with a restricted active and passive range of motion due to the formation of adhesions of the glenohumeral joint capsule. Radiographically it is a thickening of the capsule and rotator interval, risk factors consist of diabetes, hyperthyroidism and previous surgical treatment of the cervical spine [14]. The occurrence of adhesive capsulitis is about 3 percent in the overall population. It is uncommon in children, peaking between the ages of 40 and 70. Females are more commonly affected than males, but there is no known genetic or racial predisposition. People with the past of adhesive capsulitis are at greater hazard of exacerbating the situation on the contralateral side [15].
The recommended age at onset is usually 55 years. Females may be slightly more dominant (1.4:1). Usually, the non-dominant hand is pretentious. Remarkably, numerous comorbid autoimmune diseases have been shown to predispose sufferers to this situation, with thyroid problems and diabetes mellitus. In addition, liable on the duration of diabetes, diabetics often have worse treatment consequences [16]. The frequency of adhesive capsulitis of the shoulder increased to 24.9% in diabetics [17]. Frozen shoulder is often diagnosed in patients with a painful frozen shoulder. This period, first cast-off by Codman, does not designate a selected pathology. Instead, it relates to what he called many conditions that cause short rotator spasms or adhesions in the joint or bursa area [18]. Adhesive capsulitis has a pathogenesis that is unclear. According to the maximally regular theory, infection begins in the joint capsule and synovial fluid. Sensitive fibrosis and adhesions of the joint’s synovial lining are used to detect infection [19]. The pathology of the disease and its classification narrates to infection and the formation of enormous scar tissue. Adhesive capsulitis has historically been characterized as primary (idiopathic) or secondary (resulting from an underlying situation) [20]. Pain is usually given as originating in the deltoid muscle. Night-time ache is not uncommon, and patients generally cannot sleep on the affected side. Pain after repeated overhead activity is not a standard feature of this disorder and suggests pathology. The contracted, adherent capsule causes pain, mainly while their miles dilate abruptly, and creates a mechanical restriction on movement [21].
AC has been categorized as primary and secondary. Primary AC is considered by complete capsular infection and fibrosis that occurs with no identified advancing cause. Rather, secondary AC encompasses many situations that cause frozen shoulder, consisting of rotator cuff tears (RCT), glenohumeral or acromionic clavicular arthritis, and previous shoulder injuries or surgical treatments [22]. Adhesive capsulitis is characterised by shoulder discomfort and a markedly restricted range of motion. The pain is described as a dull, poorly localised discomfort that might radiate to the biceps. Reaching above or at the back of the back might also cause discomfort and stiffness. Fever, night sweats, lethargy, or unexplained weight loss should alert the naturopath to the possibility of an incidental prognosis, such as a tumour or an inflammatory illness. Cervical radiculopathy is indicated by the presence of neuropathic signs and symptoms [23]. The greatest common features of AC are pain accompanying with progressive stiffness and lack of shoulder external rotation actions. Loss of variable movement may also be present, sticking to the site of the maximally affected capsule. Pain may be anterior or posterior, sometimes extending across the bicep’s tendon, especially when lying on the mattress; however, in most cases the pain cannot be dependably located [24].
In general, three different grades can be identified: 1. Grade I (freezing) lasts ten to thirty-six weeks. The most common adverse effect is discomfort, which is worst in the nights and does not respond well to nonsteroidal anti-inflammatory medicines taken orally. The range of motion begins to be restricted at this point.
2. Grade II (frozen) having 4 to 12-month duration. The discomfort fades with time, but the stiffness stays, resulting in a near-complete loss of external rotation.
3. Grade III (thawing) can remain anywhere from 12 to 42 months, with some writers reporting stiffness lasting as long as seven years. Stiffness slowly fades and range of motion slowly returns throughout this period [25].
The predominant clinical finding in adhesive capsulitis is mobility restriction, which includes forward bending, abduction, and external and internal rotation. A patient’s sense of gait may also reveal a lack of the regular arm swing that occurs when walking as the condition advances. Examining the afflicted shoulder might potentially reveal muscular loss. Palpation may reveal an undefined soreness over the anterior and posterior shoulders; nevertheless, the predominant tenderness is atypical, indicating a different diagnosis or accompanying disease in the shoulder [26]. No laboratory tests are shown for diagnosis. Imaging is not specified. Typically, range of motion is lost in the following order: external rotation, abduction, internal rotation, forward flexion. Subsequent diagnostic physical examinations to gauge impingement and rotator cuff tendinopathy were negative: Neer impingement sign, Hawkins sign, pain provocation, Teres minor sag sign, and subscapularis lift-off tests [27]. It has been reported in the literature that the restricted range of motion (ROM) and ache may be the result of myofascial trigger points (MTrPs) in the muscle tissue of the shoulder girdle [28]. Patients with dynamic trigger points were also shown to have more impairment and worse sleep. A good treatment couturier to the mark of the aching shoulder muscle with active cause point should end up having a lasting end result. The response to the problem of various manual treatments has been an explosion in the literature on the treatment of patients with adhesive capsulitis. In individuals with painful adhesive capsulitis, recent study has revealed the benefits of trigger point stimulation and post isometric relaxation [29].
Trigger points are felt around the shoulder joints in frozen shoulder. Tender areas embedded in tight bands of rigid muscle are known as myofascial trigger points. These sites are always sensitive, preventing the muscle from fully extending and resulting in muscular weakness [30]. The trigger points in a frozen shoulder are commonly found in the subscapularis, supraspinatus, pectoralis major and minor, and deltoid. The thoracic fascia and inferior glenohumeral capsule are frequently constricted.30 Simons et al advices was followed. The beginning of the pressure pain was also assessed. The Visual Analogue Scale (VAS) and the Disability of the Arm, Shoulder, and Hand (DASH) scales were used to assess pain and function, respectively [31]. Adhesive capsulitis is usually a selflimiting condition with a high likelihood of spontaneous recovery between 18 to 30 months. The goal of treatment is to alleviate discomfort and improve range of motion. The Shoulder Pain and Disability Index (SPADI), Numerical Pain Rating Scale (NPRS), and Passive Range of Motion were three of the 27 outcomes (PROM). For SPADI, the postal evaluation was repeated after a year [32]. Lin- Fen Hsieh et al. showed in an RCT that supplementing conventional physiotherapy with hyaluronic acid injections does not bring any substantial additional advantage for the treatment of patients with ACS and may proliferation pointless medical expenses [33]. Most instances cure spontaneously, therefore treatment is conservative, albeit a small percentage of patients proceed to chronic impairment [34]. Physiotherapy is widely accepted as a crucial role in preserving mobility by preventing capsular constriction and retrieving range of motion as soon as symptoms allow, and it should be employed in the conservative treatment of adhesive capsulitis [35]. Joint mobilization techniques such as traction and gliding have been used to stretch the attached capsule and enhance physiological ancillary movements [36].
The stretch’s intensity should be proportional to the patient’s patience and the tissue’s physical endurance. It’s also crucial to educate the patient on the pathology and the self-limiting nature of the illness, as complete range of motion may never be regained [37]. Modalities, manual approaches, and therapeutic exercises are frequently employed in physiotherapeutic therapies for patients with frozen shoulder [38]. Electrotherapy modalities (also known as electrophysical agents) are forms of physical therapy that increase energy (electrical, sound, light, and heat) into the body to relieve pain and improve function. Therapeutic ultrasound, low-level laser treatment (LLLT), interferential current, transcutaneous electrical nerve stimulation (TENS), and pulsed electromagnetic field therapy are all examples of non-invasive therapies (PEMF) [39]. The contrast of the concomitant effects of MET and ART has not been studied because these techniques act quickly and reduce symptoms at trigger points quickly [40]. Another recent study by Russel et al. found that anxiety and sadness appear to be an essential element of ACS symptoms, and that physical therapy therapies in a group exercise class were more effective in reducing signs and symptoms because they focused on this aspect of the illness [41]. Sooner or later, when deciding on a physical treatment method for ACS it’s far vital to don’t forget the affected person’s signs and symptoms, degree of situation and popularity of various patterns of motion loss [42].
Material and Method
Study Design
Randomized Controlled Trial
Settings
Study will be conducted in Spot Rehab, Johar town, lahore.
Study Duration
9 months after the approval of synopsis.
Sample Size
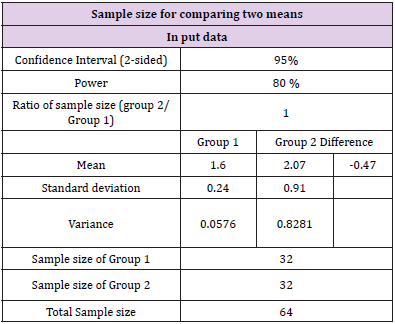
74 patients will be randomly divided into two equal groups of 37 each (Table 1). The calculated sample size using Painion as outcome measure is 32 in each group after adding 20% dropout the sample size will be 32+5=37 in each group [43].

Z1-α/2 Level of significance=95% [43].
μ1 Expected mean change in Pain in Control Group= 1.6 [43].
μ2 Expected mean change in Pain in Experimental Group= 2.07 [43].
δ1 Expected standard deviation in Control group=0.24 [43].
δ2 Expected standard deviation in Experimental group=0.91 [43].
Z1-β power of the study= 80%
n Expected sample size in a group= 32 [43].
After adding 20% drops out 32+5=37 in each group. [43].
Sampling Technique
Convenient sampling technique
Sample Selection:
Inclusion Criteria:
1. Both male and female.
2. Participants having unilateral adhesive capsulitis.
3. Participants with sub-acute adhesive capsulitis.
4. Participants having age of 40-60 years [44].
Exclusion Criteria:
1. Patient with cervical radiculopathy.
2. Fractures of upper limb.
3. Thoracic outlet syndrome.
4. Post-traumatic.
Results (Table 2)
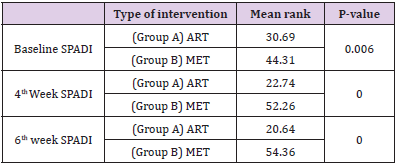
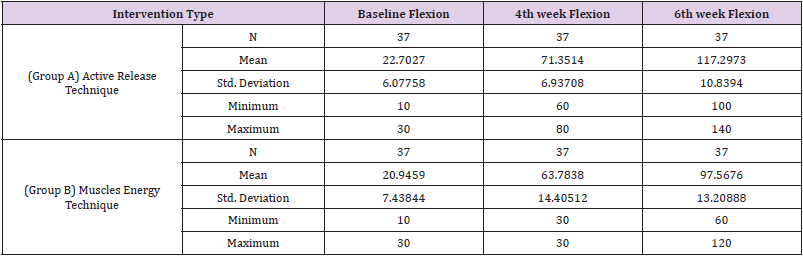
Between group comparison of (Group A) ART and (Group B) MET on the basis of NPRS. Mean rank of NPRS baseline reading of group 1 was 31.62 and for group 2 was 43.38 with, p value 0.12. Mean rank for NPRS 4th week reading was 25.85 for group 1 and 49.15 for group 2 with, p value 0.00. Mean rank for NPRS 6th week was 21.59 for group 1 and 53.41 for group 2 with, p value 0.00. The results show that there was a statistically significant difference between the groups with the p-value< 0.05. According to these results there is significant difference in ART and MET on NPRS scale (Table 2). Between group comparison of (Group A) ART and (Group B) MET on the basis of SPADI. Mean rank of SPADI baseline reading of group 1 was 30.69 and for group 2 was 44.31 with, p value 0.006. Mean rank for SPADI 4th week reading was 22.74 for group 1 and 52.26 for group 2 with, p value 0.00. Mean rank for SPADI 6th week was 52.26 for group 1 and 54.36 for group 2 with, p value 0.00. The results show that there was a statistically significant difference between the groups with the p-value< 0.05. According to these results there is significant difference in ART and MET on SPADI scale (Table 3). Baseline flexion, week 4th flexion and week 6th flexion across the group. In group B (MET) baseline flexion, mean (20.9459), Standard deviations (7.43844) maximum and minimum value was (30.00), (10.00). Week4_ROM flexion, mean 63.7838, standard deviation 14.40512, maximum 30.00 and minimum value was 30.00. Week6_ROM flexion, mean 97.5676 standard deviation 13.20888 maximum 120.00 and minimum value was 60.00 respectively (Table 4).
Table 4: Above table summarizes baseline flexion, week 4th flexion and week 6th flexion across the group. In group A (ART) baseline flexion, mean (22.7027), Standard deviations (6.07758) maximum and minimum value was (30.00), (10.00). Week4_ROM flexion, mean 71.3514, standard deviation 6.93708, maximum 80.00 and minimum value was 60.00. Week6_ROM flexion, mean 117.2973 standard deviation 10.83940 maximum 140.00 and minimum value was 100.00 respectively.
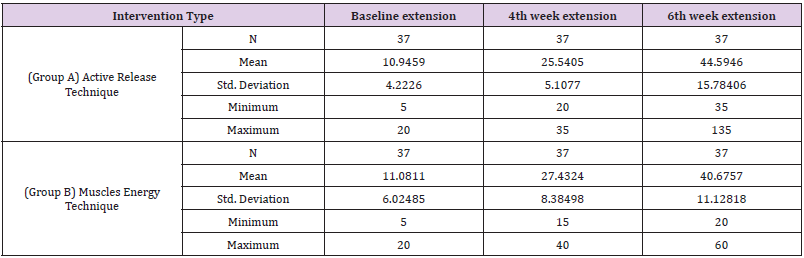
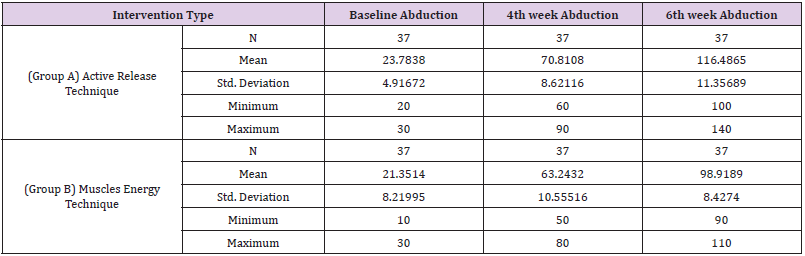
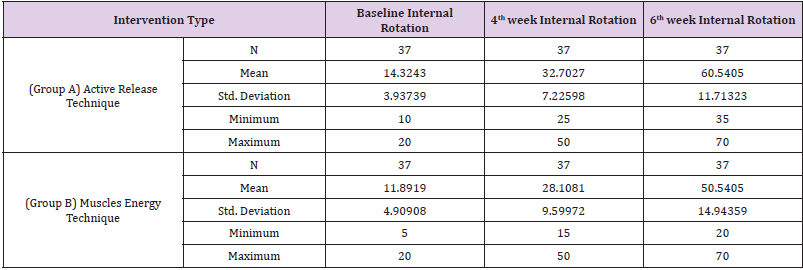
Baseline extension, week 4th extension and week 6th extension across the group. In group B (MET) baseline extension, mean (11.0811), Standard deviations (6.02485) maximum and minimum value was (20.00), (5.00). Week4_ROM extension, mean 27.4324, standard deviation 8.38498, maximum 40.00 and minimum value was 15.00. Week6_ROM extension, mean 40.6757 standard deviation 11.12818 maximum 60.00 and minimum value was 20.00 respectively (Table 5). Baseline abduction, week 4th abduction and week 6th abduction across the group. In group B (MET) baseline abduction, mean (21.3514), Standard deviations (8.21995) maximum and minimum value was (30.00) and (10.00). Week4_ ROM abduction, mean 63.2432, standard deviation 10.55516, maximum 80.00 and minimum value was 50.00. Week6_ROM abduction, mean 98.9189 standard deviation 8.42740 maximum 110.00 and minimum value was 90.00 respectively (Table 6). Baseline internal rotation, week 4th internal rotation and week 6th internal rotation across the group. In group B (MET) baseline internal rotation, mean (11.8919), Standard deviations (4.90908) maximum and minimum value was (20.00) and (5.00). Week4_ ROM internal rotation, mean 28.1081, standard deviation 9.59972, maximum 50.00 and minimum value was 15.00. Week6_ROM internal rotation, mean 50.5405 standard deviation 14.94359 maximum 70.00 and minimum value was 20.00 respectively (Table 7).
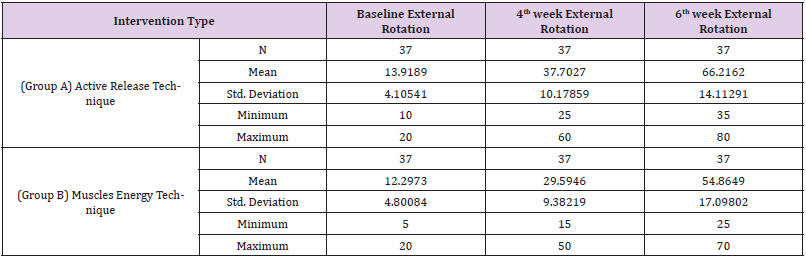
Baseline external rotation, week 4th external rotation and week 6th external rotation across the group. In group B (MET) baseline external rotation, mean (12.2973), Standard deviations (4.80084) maximum and minimum value was (20.00) and (5.00). Week4_ROM external rotation, mean 29.5946, standard deviation 9.38219, maximum 50.00 and minimum value was 15.00. Week6_ ROM external rotation, mean 54.8649 standard deviation 17.09802 maximum 70.00 and minimum value was 25.00 respectively. Statistically there was a difference between the two groups as p< 0.05 and within-group changes show that there was a significant change in baseline, 4th week, and 8th-week readings for NPRS, ROM and SPADI with p < 0.05 (Table 8).
Table 5: Above table summarizes baseline extension, week 4th extension and week 6th extension across the group. In group A (ART) baseline extension, mean (10.9459), Standard deviations 4.22260) maximum and minimum value was (20.00), (5.00). Week4_ROM extension, mean 25.5405, standard deviation 5.10770, maximum 35.00 and minimum value was 20.00. Week6_ROM extension, mean 44.5946 standard deviation 15.78406 maximum 135.00 and minimum value was 35.00 respectively.
Table 6: Above table summarizes baseline abduction, week 4th abduction and week 6th abduction across the group. In group A (ART) baseline abduction, mean (23.7838), Standard deviations (4.91672) maximum and minimum value was (30.00), (20.00). Week4_ROM extension, mean 70.8108, standard deviation 8.62116, maximum 90.00 and minimum value was 60.00. Week6_ROM abduction, mean 116.4865 standard deviation 11.35689 maximum 140.00 and minimum value was 100.00 respectively.
Table 7: Above table summarizes baseline internal rotation, week 4th internal rotation and week 6th internal rotation across the group. In group A (ART) baseline internal rotation, mean (14.3243), Standard deviations (3.93739) maximum and minimum value was (20.00), (10.00). Week4_ROM internal rotation, mean 32.7027, standard deviation 7.22598, maximum 50.00 and minimum value was 25.00. Week6_ROM internal rotation, mean 60.5405 standard deviation 11.71323 maximum 70.00 and minimum value was 35.00 respectively.
Table 8: Above table summarizes baseline external rotation, week 4th external rotation and week 6th external rotation across the group. In group A (ART) baseline external rotation, mean (13.9189), Standard deviations (4.10541) maximum and minimum value was (20.00), (10.00). Week4_ROM external rotation, mean 37.7027, standard deviation 10.17859, maximum 60.00 and minimum value was 25.00. Week6_ROM external rotation, mean 66.2162 standard deviation 14.11291 maximum 80.00 and minimum value was 35.00 respectively.
Discussion
The study meant to define the effect of the active release technique and the muscle energy technique on pain, range of motion and functional disability in subacute adhesive capsulitis patients with trigger points using a numerical pain rating scale and shoulder pain and disability index, and to compare the effects of the two exercises, in the 4th and 6th week. In this study, the Active Release Technique had positive and immediate effects, confirming a reduction in pain and functional disability. Exercise interventions will be beneficial in relieving pain and associated musculoskeletal disorders due to trigger points in adhesive capsulitis. Active release technique and muscle energy technique are very important for the well-being of patients with trigger points in adhesive capsulitis. Statistically, there is significant differences were found between ART and MET with a p-value (p<0.05). According to an experimental study conducted in 2019 to determine the effectiveness of the active release technique and muscle energy technique on subscapularis trigger points with measuring tools were VAS, SPADI and Universal Goniometery. Significant improvement in Group A (Active Release Technique) than Group B (Muscle Energy Technique) and C (Conventional Therapy or Routine Physical Therapy) in the treatment of subscapularis trigger points [45]. In 2019, an experimental study to parallel the efficacy among the muscle energy technique and the Cyriax technique versus the mobilization technique in adhesive capsulitis and after the treatments analysis showed that the Muscle Energy Technique with Mobilization Technique shows greater improvement than Cyriax’s Deep Friction Technique with Mobilization Technique [45].
Another study was conducted in 2016. The purpose of this study was to compare the effect of two manual treatments, namely the active release technique (ART) and the muscle energy technique (MET), on upper trapezius trigger points. Both manual techniques of ART and MET increase range of motion and reduce symptoms of LTrPs in the upper trapezius equally, with no technique superior to the other [40]. In 2016, a study to see Spencer MET affected pain and functional impairment in people with adhesive capsulitis of the shoulder joint, and subjects were randomly allocated in two groups, Group A received conventional treatment plus METs, and Group B received conventional treatment alone and the results for Both groups showed substantial improvement, but the Spencer MET is more effective than conventional treatment in improving function in patients with adhesive capsulitis [46]. In 2013, the most innovative therapeutic approach developed for idiopathic adhesive capsulitis, in which 30 participants of two groups of 15 participants receive Maitland mobilization, and Muscle Energy Technique (MET) and pain alleviation was reported greater in the MET group, ROM improvement was seen more in the Maitland mobilization group [47]. Another study was conducted in 2017.
The aim of this study is to determine the immediate effects of the active release technique (ART) in patients with adhesive capsulitis. The statistical analysis is performed by comparing the means before and after the test, shows a highly significant increase in the range of motion at the shoulder joint and a decrease in pain intensity, and shows that the Active Release technique is effective in patients with adhesive capsulitis [ subacute stage] [48]. Another study in 2015 to determine the value of the proprioceptive neuromuscular facilitation (PNF) and muscle energy techniques (MET) in the treatment of adhesive capsulitis of the shoulder and after two weeks of post interventional assessment the results shows that individuals with adhesive capsulitis, the proprioceptive neuromuscular facilitation approach proved effective in relieving pain, restoring ROM, and restoring function [49]. All of these studies proved that Active release technique and Muscle energy technique are effective maneuvers in reducing shoulder pain and disability.
References
- Miniato MA, Anand P, Varacallo M (2021) Anatomy, shoulder and upper limb, shoulder. Stat Pearls: Stat Pearls Publishing.
- McCausland C, Sawyer E, Eovaldi BJ, Varacallo M (2018) Anatomy, shoulder and upper limb, shoulder muscles.
- Eovaldi BJ, Varacallo M (2018) Anatomy, shoulder and upper limb, shoulder muscles. StatPearls Treasure Island, FL: Stat Pearls.
- Aguirre K, Mudreac A, Kiel J (2021) Anatomy, shoulder and upper limb, subscapularis muscle. Stat Pearls: Stat Pearls Publishing.
- Gasbarro G, Bondow B, Debski R (2017) Clinical anatomy and stabilizers of the glenohumeral joint. Annals of Joint 2(10).
- Veeger H, Van Der Helm F (2007) Shoulder function: the perfect compromise between mobility and stability. Journal of biomechanics 40(10): 2119-2129.
- Siegel LB, Cohen NJ, Gall EP (1999) Adhesive capsulitis: a sticky issue. American family physician 59(7): 1843.
- Wang K, Ho V, Hunter-Smith DJ, Beh PS, Smith KM, et al. (2013) Risk factors in idiopathic adhesive capsulitis: a case control study. Journal of shoulder and elbow surgery 22(7): e24-e9.
- Sui-Foon Lo, Ssu-Wei Chu, Chih-Hsin Muo, Nai-Hsin Meng, Li-Wei Chou, et al. (2014) Diabetes mellitus and accompanying hyperlipidemia are independent risk factors for adhesive capsulitis: a nationwide population-based cohort study (version 2). Rheumatology international 34(1): 67-74.
- Page MJ, O’Connor DA, Malek M, et al. (2019) Patients’ experience of shoulder disorders: a systematic review of qualitative studies for the OMERACT Shoulder Core Domain Set. Rheumatology 58(8): 1410-1421.
- Ramirez J (2019) Adhesive capsulitis: diagnosis and management. American family physician 99(5): 297-300.
- Wen Zhao, Xiaofeng Zheng, Yuying Liu, Wenlu Yang, Vardan Amirbekian, et al. (2012) An MRI study of symptomatic adhesive capsulitis. PLoS One 7(10): e47277.
- Lee SH, Yoon C, Chung SG, Hee Chan Kim, Youngbin Kwak, et al. (2015) Measurement of shoulder range of motion in patients with adhesive capsulitis using a Kinect. PloS one 10(6): e0129398.
- Redler LH, Dennis ER (2019) Treatment of adhesive capsulitis of the shoulder. JAAOS-Journal of the American Academy of Orthopaedic Surgeons 27(12): e544-e54.
- Ewald A (2011) Adhesive capsulitis: a review. American family physician 83(4): 417-22.
- St Angelo JM, Fabiano SE (2018) Adhesive capsulitis.
- Ahmad S, Rafi MS, Siddiqui IA, Hamidi K, Faruq NM (2012) The frequency of adhesive capsulitis in diabetes mellitus patients. Pak J Rehabilit 1(2): 49-55.
- Neviaser AS, Neviaser RJ (2011) Adhesive capsulitis of the shoulder. JAAOS-Journal of the American Academy of Orthopaedic Surgeons 19(9): 536-542.
- Brue S, Valentin A, Forssblad M, Werner S, Mikkelsen C, et al. (2007) Idiopathic adhesive capsulitis of the shoulder: a review. Knee Surgery, Sports Traumatology. Arthroscopy 15(8): 1048-1054.
- Chiaramonte R, Bonfiglio M, Chisari S (2020) A significant relationship between personality traits and adhesive capsulitis. Revista da Associação Médica Brasileira 66: 166-173.
- Ahn K-S, Kang CH, Oh Y-W, Jeong W-K (2012) Correlation between magnetic resonance imaging and clinical impairment in patients with adhesive capsulitis. Skeletal radiology 41(10): 1301-1308.
- D’Orsi GM, Via AG, Frizziero A, Oliva F (2012) Treatment of adhesive capsulitis: a review. Muscles, ligaments and tendons journal 2(2): 70.
- Donatelli R, Ruivo R, Thurner M, Ibrahim MI (2014) New concepts in restoring shoulder elevation in a stiff and painful shoulder patient. Physical Therapy in Sport 15(1): 3-14.
- Harris G, Bou‐Haidar P, Harris C (2013) Adhesive capsulitis: review of imaging and treatment. Journal of medical imaging and radiation oncology 57(6): 633-643.
- Marcello Zappia, Francesco Di Pietto, Alberto Aliprandi, Simona Pozza, Paola De Petro, et al. (2016) Multi-modal imaging of adhesive capsulitis of the shoulder. Insights into imaging 7(3): 365-371.
- Marcio Schiefer, Patricia F Santos Teixeira, Cesar Fontenelle, Tiago Carminatti, Daniel A Santos, et al. (2017) Prevalence of hypothyroidism in patients with frozen shoulder. Journal of shoulder and elbow surgery 26(1): 49-55.
- Jordan CL, Rhon DI (2012) Differential diagnosis and management of ankylosing spondylitis masked as adhesive capsulitis: a resident's case problem. Journal of orthopaedic & sports physical therapy 42(10): 842-852.
- Kalia V, Mani S, Kumar SP (2021) Short-term effect of myofascial trigger point dry-needling in patients with Adhesive Capsulitis. Journal of bodywork and movement therapies 25: 146-50.
- Jeyakumar S, Alagesan J, Jayashree P (2016) A comparative study on the effectiveness of myofascial trigger point release and maitland techniques in adhesive capsulitis of shoulder. International Journal of Medical and Health Research 2: 1-7.
- Gurudut P, Welling A, Kudchadkar G (2019) Combined Effect of Gross and Focused Myofascial Release Technique on Trigger Points and Mobility in Subjects with Frozen Shoulder-A Pilot Study.
- Jorge H Villafañe, Maria P Lopez-Royo, Pablo Herrero, Kristin Valdes, Raquel Cantero-Téllez, et al. (2019) Prevalence of myofascial trigger points in poststroke patients with painful shoulders: A cross‐sectional study. Pm &R 11(10): 1077-1082.
- Sharma SP, Bærheim A, Moe-Nilssen R, Kvåle A (2016) Adhesive capsulitis of the shoulder, treatment with corticosteroid, corticosteroid with distension or treatment-as-usual; a randomised controlled trial in primary care. BMC musculoskeletal disorders 17(1): 1-10.
- Hsieh LF, Hsu WC, Lin YJ, Chang HL, Chen CC, et al. (2012) Addition of intra-articular hyaluronate injection to physical therapy program produces no extra benefits in patients with adhesive capsulitis of the shoulder: a randomized controlled trial. Archives of physical medicine and rehabilitation 93(6): 957-964.
- Brandon KK Fields, Matthew R Skalski, Dakshesh B Patel, Eric A White, Anderanik Tomasian, et al. (2019) Adhesive capsulitis: review of imaging findings, pathophysiology, clinical presentation, and treatment options. Skeletal radiology 48(8): 1171-1184.
- Wilson J, Russell S, Walton MJ (2015) The management of frozen shoulder. Current Physical Medicine and Rehabilitation Reports 3(2): 181-187.
- Paul A, Rajkumar JS, Peter S, Lambert L (2014) Effectiveness of sustained stretching of the inferior capsule in the management of a frozen shoulder. Clinical Orthopaedics and Related Research® 472(7): 2262-2268.
- Martin J Kelley, Michael A Shaffer, John E Kuhn, Lori A Michener, Amee L Seitz, et al. (2013) Shoulder pain and mobility deficits: adhesive capsulitis: clinical practice guidelines linked to the international classification of functioning, disability, and health from the Orthopaedic Section of the American Physical Therapy Association. Journal of orthopaedic & sports physical therapy 43(5): A1-A31.
- Page P, Labbe A (2010) Adhesive capsulitis: use the evidence to integrate your interventions. North American journal of sports physical therapy: NAJSPT 5(4): 266.
- Page MJ, Green S, Kramer S, Johnston RV, McBain B (2014) Buchbinder R. Electrotherapy modalities for adhesive capsulitis (frozen shoulder). Cochrane Database of Systematic Reviews (10).
- Sadria G, Hosseini M, Rezasoltani A, Bagheban AA, Davari A, et al. (2017) A comparison of the effect of the active release and muscle energy techniques on the latent trigger points of the upper trapezius. Journal of bodywork and movement therapies 21(4): 920-925.
- Russell S, Jariwala A, Conlon R, Selfe J, Richards J, et al. (2014) A blinded, randomized, controlled trial assessing conservative management strategies for frozen shoulder. Journal of shoulder and elbow surgery 23(4): 500-507.
- Struyf F, Meeus M (2014) Current evidence on physical therapy in patients with adhesive capsulitis: what are we missing? Clinical rheumatology 33(5): 593-600.
- Shetty SS, Shah RR (2020) Effect of Maitland Technique (Posterior Glide) with Muscle Energy Technique for Subscapularis Muscle on Adhesive Capsulitis. Website: www ijpot com 14(02): 2203.
- Vijayan V, Jayabharathi S (2019) A comparative study on effectiveness of muscle energy technique versus Cyriax’s deep friction technique in adhesive capsulitis. INDIAN ASSOCIATION OF BIOMEDICAL SCIENTISTS (IABMS) org 39(4): 622-627.
- Yatheendra Kumar G,Sudhakar S, Sudhan SG, Sivajyothi N, Senthil Selvam P, et al. (2017) Effectiveness of active release technique and muscle energy technique in adhesive capsulitis.
- Contractor ES, Agnihotri DS, Patel RM (2016) Effect of spencer muscle energy technique on pain and functional disability in cases of adhesive capsulitis of shoulder joint. IAIM 3(8): 126-131.
- Suri SA, Anand M (2013) Comparative study on the effectiveness of Maitland mobilization technique versus muscle energy technique in treatment of shoulder adhesive capsulitis. Indian Journal of Physiotherapy & Occupational Therapy-An International Journal 7(4): 1-6.
- Rajalaxmi V, Vasanthi S, Sathya S, K Kirupa (2021) Efficacy of Dynamic VS Closed Kinematic Exercise Combined with Stretching in Adhesive Capsulitis-a double blinded randomized controlled trial. Bangladesh Journal of Medical Science 20(2): 368-373.
- Ravichandran H, Balamurugan J (2015) Effect of proprioceptive neuromuscular facilitation stretch and muscle energy technique in the management of adhesive capsulitis of the shoulder. Saudi journal of sports medicine 15(2): 170.

 Research Article
Research Article