ABSTRACT
Mortality and morbidity due to the novel severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2 or COVID-19) are associated with various clinical and nonclinical factors including HIV and health system-related factors. This study explores the temporal association of COVID-19 incidence and mortality with clinical and non-clinical factors through an ecological analysis of secondary data from 26 states in India. State-level outcome variables were COVID-19 cumulative incidence and mortality and the risk factors include Human Immunodeficiency Virus/ Acquired immunodeficiency syndrome (HIV/AIDS) incidence, mortality and PMTCT (prevention of mother-to-child transmission of HIV) needs, general vaccination coverage, poverty status, sex ratio, child sex ratio, obesity (Body Mass Index, BMI>25) and air travel risk ratio. Linear regression analysis was done to investigate the effect of covariates on COVID-19 mortality. The findings revealed that People Living with HIV/AIDS (PLHIV) are at higher risk for COVID-19 incidence and mortality, which suggests the need for focused interventions and uninterrupted access to Antiretroviral therapy (ART) and treatment for co-infections and comorbidities to mitigate the impact of COVID -19. The findings intend to provide insights to support and design India’s public health strategy for its response to the COVID-19 pandemic, especially among PLHIVs.
Keywords: SARS-CoV-2; COVID-19; HIV; BMI; Vaccine Coverage
Abbreviations: HIV/AIDS: Human Immunodeficiency Virus/ Acquired Immunodeficiency Syndrome; PLHIV: People Living with HIV/AIDS; ART: Antiretroviral Therapy; NCDs: Non-Communicable Diseases; SARS-CoV-2: Severe Acute Respiratory Syndrome Coronavirus-2; HIV: Human Immunodeficiency Virus; MoHFW: Ministry of Health and Family Welfare; WHO: World Health Organization; CDC: Center for Disease Control and Prevention; MMR: Measles Mumps Rubella
Introduction
The COVID-19 pandemic has already infected over 494 million people worldwide, leading to over 6 million deaths [1]. With about one-third of confirmed cases in Asia, India witnessed around 43 million infected cases with over 500,000 deaths as of April 2022 [2]. Ever since the first outbreak in December 2019, researchers have been reporting significant associations between mortality and morbidity due to severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2), causing the coronavirus disease 2019 (COVID-19) and various clinical and non-clinical factors, including Human Immunodeficiency Virus (HIV) infection, non-communicable diseases (NCDs), socioeconomic, demographic and health system factors [3-6]. Generation of context and geographic-specific evidence related to the factors associated with the SARS-CoV-2 infection and mortality is critical for policymakers to develop evidence-based strategies and targeted interventions such as age and vulnerability-specific prevention and control programmes. This study presents an analysis of the association between COVID-19 incidence, mortality and clinical and non-clinical factors, intending to provide an insight to support and design public health strategies for its response to the pandemic.
Methods
We compiled the data for two time periods, March to August 2020 and March to June 2021 from multiple secondary data sources for 26 states of India. Data related to COVID-19 incidence and mortality were obtained from the Ministry of Health and Family Welfare (MoHFW) website https://www.mohfw.gov. in/ and https://api.covid19india.org/csv/latest/state_wise.csv (last accessed on 1st July 2021). HIV related data were obtained from various technical reports published by the National AIDS Control Organization (NACO), Ministry of Health and Family Welfare (MoHFW), Government of India [7]. Data related to sociodemographic, economic characteristics, vaccination coverage as a measure for health system performance and average genderspecific body mass index (BMI) were obtained from National Family Health Survey (NFHS-4) factsheets [4,8,9]. As complete information on all variables could be obtained only for 26 states and UTs in the country, they were included in the analysis. We considered outcome variables such as cumulative confirmed COVID-19 incidence (burden) and mortality for the two different periods. HIV incidence, HIV prevalence, HIV mortality, PMTCT needs, general vaccination coverage, Sex-ratio, child sex ratio, the proportion of people in poverty, BMI and air-travel density (risk score) were considered as potential risk factors.
Statistical Analysis
Binary associations between the independent and outcome variables were first explored using scatterplots. The associations were then quantified using spearman’s rank correlation to assess the relationship between the independent variables and outcomes variables such as cumulative COVID-19 incidence and mortality. All correlations were reported and factors that were significant at p-value of 0.1 were included in the ecological analysis. Linear regression models were fitted to assess the quantum of association of the covariates on the COVID-19 incidence and mortality. Separate models were fitted for the two time periods, March- August 2020 and March-June 2021 as there were differences in case identification strategies, reporting and other programmatic efforts. The covariates included in the regression model were: general vaccine coverage (as a measure of health systems performance), sex ratio, percentage below poverty line (as a measure of social determinant of health), BMI (as a measure of nutritional status, obesity), HIV prevalence, HIV incidence, HIV related mortality, PMTCT needs (as measures of population highly vulnerable to infection) and air travel risk. All variables in the regression models were standardized to convert them to the same scale.
Results
Association between COVID-19 Incidence and HIV, Health System Performance and Socio-Demographic, Economic Factors
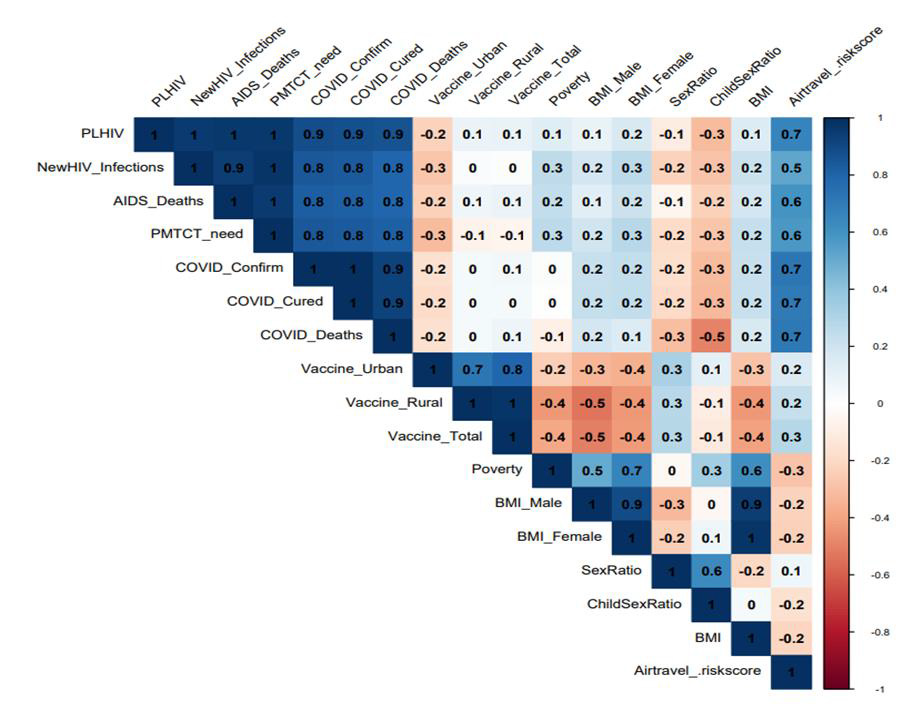
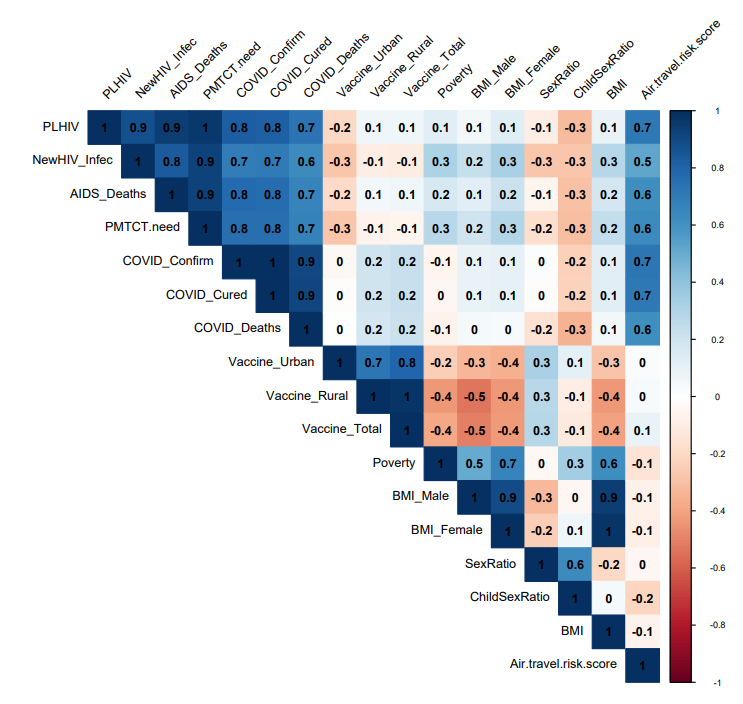
The correlation analyses (Figures 1 & 2) indicated strong positive association between COVID-19 incidence and HIV prevalence (r=0.9, p<0.001), HIV incidence (r=0.8, p<0.001), HIV related mortality (r=0.8, p<0.001) and Prevention of mother-tochild transmission (PMTCT) needs (r=0.8, p<0.001), during the time period from March to August 2020. Similarly, during the time period from March to June 2021, COVID-19 incidence was positively associated with HIV prevalence (r=0.8, p<0.001), incidence (r=0.7, p<0.001), AIDS mortality (r=0.8, p<0.001) and PMTCT needs (r=0.8, p<0.001). States with higher HIV incidence and AIDS related mortality showed a corresponding higher COVID-19 burden. The general vaccination coverage in urban areas, which is considered as a measure of health system performance indicated an inverse, albeit weak, association with COVID-19 burden (r=-0.2, p=0.4) indicating states with lower vaccination rates may have a higher number of cases in 2020. However, vaccination coverage in rural areas and overall vaccination coverage did not indicate any significant association with COVID-19 case burden in both periods. In terms of the socio-demographic, and economic situation, poverty rate did not indicate any significant association with COVID-19 incidence in both the time periods. However, sex ratio (r =-0.2, r=0) and child sex ratio (r=-0.3, r=-0.2) in both the periods of the analysis showed a weak negative association with COVID-19 incidence. Overall BMI in both the period of analysis (r=0.2, r=0.1) indicated a weak positive association with COVID-19 incidence. However, air travel risk ratio (r=0.7; r=0.7) indicated a strong positive association with COVID-19 incidence.
Figure 1: Correlation plot of COVID-19 incidence and mortality with independent variables for the year 2020.
Figure 2: Correlation plot of COVID-19 incidence and mortality with independent variables for the year 2021.
Association between COVID Mortality and HIV, Health System Performance and Socio-Demographic, Economic Factors
The magnitude of association between COVID-19 mortality and HIV related indicators that are HIV prevalence, HIV incidence, HIV related mortality and PMTCT needs were almost the same as COVID-19 incidence. COVID-19 mortality did not indicate any significant correlation with general vaccination coverage in both urban and rural areas. Poverty rate (r=-0.1; r=-0.1) indicated a very weak negative association with COVID-19 mortality in both periods. Similarly, sex ratio (r =-0.3, r= -0.2) and child sex ratio (r=-0.5, r=-0.3) showed a weak negative association in both the time periods with COVID 19 mortality. The analysis indicated a very weak association between BMI (r=0.2; r=0.1) and COVID-19 mortality in both the time periods However, air travel risk ratio (r=0.7, r=0.6) indicated a strong positive association with COVID 19 mortality. Some of the correlations, although not statistically significant, hint at important directional relationships between state-level COVID-19 disease burden, mortality and the covariates.
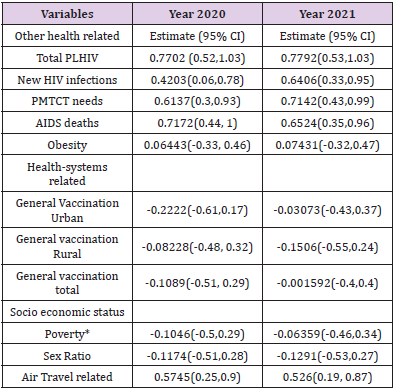
Factors Associated with COVID-19 Mortality
The regression analysis for the year 2020, indicated that for every additional case of PLHIV in the state, there is an increase of 0.77 units of COVID-19 mortality which is statistically significant. Similarly, new HIV infections, PMTCT needs, AIDS deaths and air travel risk scores of the states were found to be the significant predictors of COVID-19 mortality. Health systems performance, socio-demographic and economic factors did not show any significant association with COVID-19 mortality. Similar trends were observed for the year 2021, where the number of PLHIV, new HIV infections, PMTCT needs, AIDS deaths and air travel risk score of the states were found to be significant predictors of COVID-19 mortality (Table 1). A correlation plot of COVID-19 incidence and mortality with independent variables has been depicted in the choropleth map (Figures 1 & 2).
Table 1: Regression analysis to quantify change in COVID 19 mortality associated with the covariates.
Note: *Percentage of population below poverty line as defined for that year.
Discussion
The study highlights the significant relationship between HIV prevalence, HIV incidence, HIV related mortality, PMTCT needs and COVID-19 incidence and mortality. The findings corroborate with a population-based cohort analysis that indicated 2.9 times (95 CI: 1·96–4·30) higher risk for PLHIV dying from COVID-19 after adjusting for age and sex, compared to the general population [4]. A meta-analysis indicated a higher mortality rate due to COVID-19 among PLHIV (3.44%) compared to COVID-19 patients without HIV infection (0.42%)[10]. In addition, cohorts of hospitalized PLHIV with COVID-19 in London and New York have revealed higher rates of severe disease requiring hospitalization relative to those without an HIV diagnosis and higher mortality even with a suppressed viral load on ART [9,11-14]. The increased risk assumption for adverse COVID-19 outcomes among PLHIV is found to be based on their immunosuppressed clinical status since, HIV infection is long associated with increased susceptibility to opportunistic infections because of the abnormal humoral and T-cell mediated immune responses [15,16].
On the other hand, HIV/SARS‐CoV‐2 co-infected patients may have mortality benefits from the immunosuppressive state [17,18]. Though concerns were raised by the World Health Organization (WHO) and Center for Disease Control and Prevention (CDC) for population at high risk including PLHIV for severe health outcomes due to COVID-19, factors like immunological and virological status of PLHIV with consumption of antiretroviral treatment (ART) might play a role in the outcome of COVID-19 infection [19,20]. The high prevalence of critical underlying co-infections among PLHIVs, in comparison to HIV-negative individuals, is found responsible for higher mortality rates due to COVID-19 and not only the HIV positive status of individuals [21]. However, adequate caution and care are required while managing COVID-19 patients with immunosuppressive conditions [15,22,23]. This study indicates protective effect of general vaccination in the reduction of COVID-19 deaths. According to literature, universal Bacillus Calmette-Guerin (BCG) vaccination policy in countries, and the rate of BCG vaccination are correlated with reduced mortality rates due to COVID-19 [24-26]. Further, it has shown to produce broad protection against viral infections and sepsis [27]. Studies have also highlighted reduced COVID-19 infection, severity and death rates among patients vaccinated with measles mumps rubella (MMR) compared to the population in the same age range without vaccination [28-31]. Supporting these findings, another study indicated higher death rates due to COVID-19 with delayed MMR vaccination programs [32].
In terms of socio-demographic and economic variables, sex ratio and child sex ratio were found to be negatively associated with COVID-19 mortality. These findings are in corroboration with a few studies indicating that infectious disease threats and deaths including COVID-19 disproportionately affect the population from less developed geographies [33-35]. According to the study, a very weak positive association was found between BMI which is a proxy for co-morbidity of obesity, and mortality due to COVID-19. However, several studies indicated higher mortality among older, people with obesity and diabetes with complications [8,36]. According to a study, frequency of obesity (BMI > 30kg/m2, 47.6%) and severe obesity (BMI > 35 kg/m2, 28.2%) was found to be higher among patients with COVID-19 infection compared to non-SARSCov- 2 respiratory disease patients (25.2% and 10.8%, respectively) [37]. Similarly, another study demonstrated higher mean values of BMI of COVID-19 infected patients who needed ICU care (25.5kg/ m2), compared with the general group (22.0kg/m2) [38]. Another systematic review suggested obesity as a prospective predictor of poor outcomes in patients with COVID-19, in all continents [39]. Data from China’s Centers for Disease Control shows that 7.3% of those with diabetes who were later diagnosed with COVID-19 died and for those with no other co-morbidity, the mortality rate was lower at 0.9% [40]. Similar studies in Italy documented that 99% of deaths were among those with at least one or other health condition, showing the highest rates among patients with three or more illnesses [41].
Conclusion
The study gained insights on the associated factors that could increase the risk of COVID-19 incidence and mortality. The study provided evidence that PLHIVs are at higher risk for COVID-19 incidence and mortality, which suggests the need for focused interventions among PLHIV, especially during a pandemic of this kind. It is also critical that there is uninterrupted access to treatment services such as ART and treatments for co-infections and comorbidities to mitigate the impact of COVID -19. As there is a higher risk for COVID-19 incidence and mortality among people with underlying chronic illness and comorbidities, public health strategies should focus on early detection, diagnosis and timely initiation of treatment.
Author’s Contributions
All authors approved the final manuscript.
Conflict of Interest
The authors declare no conflict of interest.
References
- (2021) Worldometer, Coronavirus Pandemic Update 2020.
- (2021) GOI, COVID-19 Statewise Status: Ministry of Health and Family Welfare, Government of India, 2020.
- Sanyaolu A, Okorie C, Marinkovic A, Patidar R, Younis K, et al. (2020) Comorbidity and its Impact on Patients with COVID-19. SN Compr Clin Med 2(8): 1069-1076.
- Bhaskaran K, Rentsch CT, Mac Kenna B, Schultze A, Mehrkar A, et al. (2021) HIV infection and COVID-19 death: a population-based cohort analysis of UK primary care data and linked national death registrations within the OpenSAFELY platform. The Lancet HIV 8(1): e24-e32.
- Williamson EJ, Walker AJ, Bhaskaran K, Bacon S, Bates C, et al. (2020) Factors associated with COVID-19-related death using OpenSAFELY. Nature 584(7821): 430-436.
- Ejaz H, Alsrhani A, Zafar A, Javed H, Junaid K, et al. (2020) COVID-19 and comorbidities: Deleterious impact on infected patients. Journal of Infection and Public Health 13(12): 1833-1839.
- (2021) GOI, National AIDS Control Organization Ministry of Health and Family Welfare, Government of India 2020.
- Geretti AM, Stockdale AJ, Kelly SH, Cevik M, Collins S, et al. (2021) Outcomes of Coronavirus Disease 2019 (COVID-19) Related Hospitalization Among People with Human Immunodeficiency Virus (HIV) in the ISARIC World Health Organization (WHO) Clinical Characterization Protocol (UK): A Prospective Observational Study. Clin Infect Dis 73(7): e2095-e106.
- Blanco JL, Ambrosioni J, Garcia F, Martínez E, Soriano A, et al. (2020) COVID-19 in patients with HIV: clinical case series. The Lancet HIV 7(5): e314-e316.
- Dong Y, Li Z, Ding S, Liu S, Tang Z, et al. (2021) HIV infection and risk of COVID-19 mortality: A meta-analysis. Medicine 100(26): e26573.
- Gervasoni C, Meraviglia P, Riva A, Giacomelli A, Oreni L, et al. (2020) Clinical Features and Outcomes of Patients With Human Immunodeficiency Virus With COVID-19. Clin Infect Dis 71(16): 2276-2278.
- Härter G, Spinner CD, Roider J, Bickel M, Krznaric I, et al. (2020) COVID-19 in people living with human immunodeficiency virus: a case series of 33 patients. Infection 48(5): 681-686.
- Tesoriero JM, Swain C AE, Pierce JL, Zamboni L, Wu M, et al. (2021) COVID-19 Outcomes Among Persons Living With or Without Diagnosed HIV Infection in New York State. JAMA Network Open 4(2): e2037069.
- Mellor MM, Bast AC, Jones NR, Roberts NW, Ordóñez Mena JM, et al. (2021) Risk of adverse coronavirus disease 2019 outcomes for people living with HIV. AIDS (London, England) 35(4): F1-F10.
- Mirzaei H, Mc Farland W, Karamouzian M, Sharifi H (2021) COVID-19 Among People Living with HIV: A Systematic Review. AIDS Behav 25(1): 85-92.
- Chang CC, Crane M, Zhou J, Mina M, Post JJ, et al. (2013) HIV and co-infections. Immunol Rev 254(1): 114-142.
- Qin C, Zhou L, Hu Z, Zhang S, Yang S, et al. (2020) Dysregulation of Immune Response in Patients With Coronavirus 2019 (COVID-19) in Wuhan, China. Clin Infect Dis 71(15): 762-768.
- Mascolo S, Romanelli A, Carleo MA, Esposito V (2020) Could HIV infection alter the clinical course of SARS-CoV-2 infection? When less is better. Journal of Medical Virology 92(10): 1777-1778.
- (2021) CDC, Estimated COVID-19 Burden: Centers for Disease Control and Prevention.
- (2021) WHO, Coronavirus disease (COVID-19) pandemic: World Health Organization.
- Hadi YB, Naqvi SFZ, Kupec JT, Sarwari AR (2020) Characteristics and outcomes of COVID-19 in patients with HIV: a multicentre research network study. AIDS 34(13): F3-F8.
- Garrido Hernansaiz H, Heylen E, Bharat S, Ramakrishna J, Ekstrand ML (2016) Stigmas, symptom severity and perceived social support predict quality of life for PLHIV in urban Indian context. Health Qual Life Outcomes 14(1): 152.
- Baek MS, Lee MT, Kim WY, Choi JC, Jung SY (2021) COVID-19-related outcomes in immunocompromised patients: A nationwide study in Korea. PLOS ONE 16(10): e0257641.
- Hidvégi M, Nichelatti M (2020) Bacillus Calmette-Guerin vaccination Policy and Consumption of Ammonium Chloride-Enriched Confectioneries May Be Factors Reducing COVID-19 Death Rates in Europe. Isr Med Assoc J 22(8): 501-504.
- Joy M, Malavika B, Asirvatham ES, Sudarsanam TD, Jeyaseelan L (2021) Is BCG associated with reduced incidence of COVID-19? A meta-regression of global data from 160 countries. Clin Epidemiol Glob Health 9: 202-203.
- Miller A, Reandelar MJ, Fasciglione K, Roumenova V, Li Y, et al. (2020) Correlation between universal BCG vaccination policy and reduced mortality for COVID-19. medRxiv: 20042937.
- Moorlag SJCFM, Arts RJW, Van Crevel R, Netea MG (2019) Non-specific effects of BCG vaccine on viral infections. Clinical Microbiology and Infection 25(12): 1473-1478.
- Taheri Soodejani M, Basti M, Tabatabaei SM, Rajabkhah K (2021) Measles, mumps, and rubella (MMR) vaccine and COVID-19: a systematic review. Int J Mol Epidemiol Genet 12(3): 35-39.
- Lundberg L, Bygdell M, Stukat von Feilitzen G, Woxenius S, Ohlsson C, et al. (2021) Recent MMR vaccination in health care workers and Covid-19: A test negative case-control study. Vaccine 39(32): 4414-4418.
- Ashford JW, Gold JE, Huenergardt MA, Katz RBA, Strand SE, et al. (2021) MMR Vaccination: A Potential Strategy to Reduce Severity and Mortality of COVID-19 Illness. Am J Med 134(2): 153-155.
- Hupert N, Marín Hernández D, Gao B, Águas R, Nixon Douglas F (2022) Heterologous vaccination interventions to reduce pandemic morbidity and mortality: Modeling the US winter 2020 COVID-19 wave. Proceedings of the National Academy of Sciences 119(3): e2025448119.
- Gold J (2020) MMR Vaccine Appears to Confer Strong Protection from COVID-19: Few Deaths from SARS-CoV-2 in Highly Vaccinated Populations.
- Bloom DE, Cadarette D (2019) Infectious Disease Threats in the Twenty-First Century: Strengthening the Global Response. Front Immunol 10: 549.
- Quinn SC, Kumar S (2014) Health inequalities and infectious disease epidemics: a challenge for global health security. Biosecur Bioterror 12(5): 263-273.
- Asirvatham ES, Lakshmanan J, Sarman CJ, Joy M (2020) Demystifying the varying case fatality rates (CFR) of COVID-19 in India: Lessons learned and future directions. J Infect Dev Ctries 14(10): 1128-1135.
- Djaharuddin I, Munawwarah S, Nurulita A, Ilyas M, Tabri NA, et al. (2021) Comorbidities and mortality in COVID-19 patients. Gaceta Sanitaria 35: S530-S532.
- Simonnet A, Chetboun M, Poissy J, Raverdy V, Noulette J, et al. (2020) High Prevalence of Obesity in Severe Acute Respiratory Syndrome Coronavirus-2 (SARS-CoV-2) Requiring Invasive Mechanical Ventilation. Obesity (Silver Spring) 28(7): 1195-1199.
- Peng YD, Meng K, Guan HQ, Leng L, Zhu RR, et al. (2020) Clinical characteristics and outcomes of 112 cardiovascular disease patients infected by 2019-nCoV. Zhonghua Xin Xue Guan Bing Za Zhi 48(6): 450-455.
- Tamara A, Tahapary DL (2020) Obesity as a predictor for a poor prognosis of COVID-19: A systematic review. Diabetes Metab Syndr 14(4): 655-659.
- Caballero AE, Ceriello A, Misra A, Aschner P, Mc Donnell ME, et al. (2020) COVID-19 in people living with diabetes: An international consensus. J Diabetes Complications 34(9): 107671.
- Ebhardt T, Remondini C, Bertacche M (2020) 99% of Those Who Died from Virus Had Other Illness, Italy Says 2020.

 Research Article
Research Article