ABSTRACT
Background: Patients who sustain high-energy head and face trauma suffer considerable loss of teeth and alveolar as well as periodontal tissue. Sequelae cause poor aesthetic outcomes, dysarthria, masticatory disorders, and considerably reduce the patient’s quality of life. In most cases, a separate team would treat maxillofacial fractures and provide prostheses; hence, the treatment period was longer. However, the results of treatment with removable dentures were unsatisfactory.
Case Presentation: A 29-year-old young woman suffered a high-energy trauma due to a fall. Following surgery for a jaw fracture, she underwent occlusal reconstruction with Osseo integrated implants. The same team performed maxillofacial fracture surgery and implant occlusal reconstruction, and the series of treatment plans included bone grafting and periodontal plastic surgery.
Conclusion: The treatment proved successful after more than two years with no signs of peri-implantitis. The patient was highly satisfied with the results. The maxillofacial and oral implant is very useful in such traumatic cases. Moreover, it is beneficial for the oral and maxillofacial surgeon and dental implant therapist to perform the posttreatment occlusal reconstruction in the same team, because fewer surgical procedures may be possible. Aesthetic and functional maxillofacial implant treatment and a shortened treatment period can contribute to the early rehabilitation of patients.
Keywords: High-Energy Trauma; Maxillofacial Fracture; Periodontal Plastic Surgery; Early Rehabilitation
Abbreviations: HET: High-Energy Trauma; QOL: Quality of Life; GBR: Guided Bone Regeneration
Introduction
Severe maxillofacial fractures due to high-energy trauma often result in damage to the teeth and alveolar bone. Facial deformities and disfigurement, poor aesthetics, and articulation and masticatory disorders may delay the patient’s social rehabilitation and reduce postoperative quality of life (QOL). Therefore, it is important to achieve symmetric facial morphology and reliable occlusion reconstruction. Restoring morphology and function using conventional removable dentures is difficult. Maxillofacial implants are required for predictable occlusal reconstruction in patients with maxillofacial trauma. The periodontal tissue environment around the implant affects its long-term stability; therefore, a treatment plan involving bone augmentation (bone graft and GBR) and periodontal plastic surgery is required. Digital data and setup models can help with the treatment plan. In this case, mandibular mini-plate removal and bone augmentation for maxillary alveolar bone atrophy were performed at the same time according to the treatment plan. We believe that the reduction in surgical opportunities and treatment duration has helped patients to rehabilitate early. Herein we report cases in which patient satisfaction was high after treatment and good outcomes were obtained.
Case Presentation
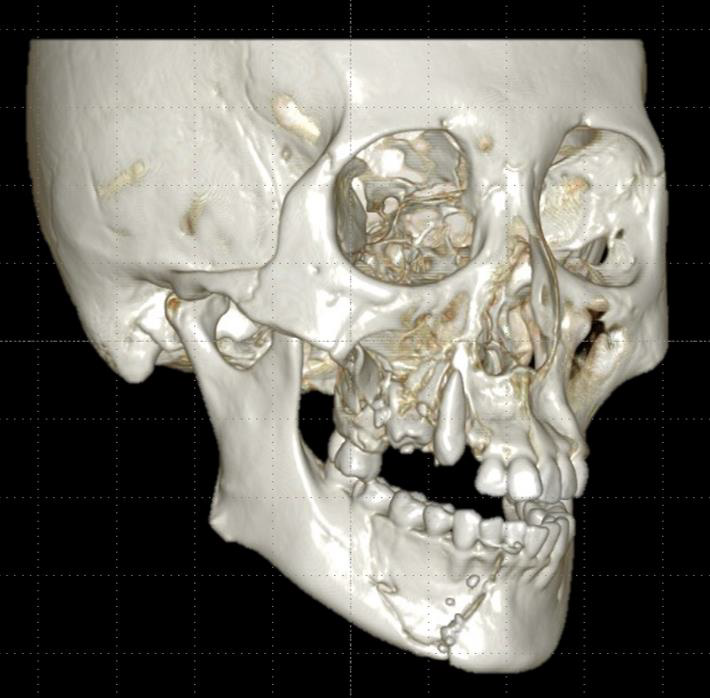
A 29-year-old woman accidentally fell at a construction site. It took an hour to rescue her from the site, and then she was brought to our emergency department for advanced trauma life support. She was fortunate to have no significant intracranial, spinal, or viscerotropic injuries. There were extensive abrasions and a subcutaneous hemorrhage on the face. The right mid-third of the face had recessed, and there was a deep laceration in the lower jaw. The frontal wall of the maxillary sinus was shattered and depressed, and the maxillary dentition was displaced inward, resulting in loss of continuity. Furthermore, the alveolar bone in the upper right 13–17 region presented with a comminuted fracture. Teeth 13, 15, and 16 were located within the fractured area. There was an insular depressed fracture in the right mandible, and the lower right 42– 46 dentition were displaced inwards, resulting in an open bite due to early occlusal contacts of the molars. There was a the right inferior alveolar nerve paralysis (Figures 1 & 2). We confirmed the preoperative and postoperative dentition and occlusal conditions before surgery via model surgery and formulated a surgical plan. The first surgery was performed under general anesthesia to restore the continuity of the jawbone and the dentition. As the zygomatic arch was intact, the frontal wall of the maxillary sinus and the maxillary dental arch were repositioned to restore the contour of the cheek. The dislocated tooth 13 was fixed within the dentition, whereas teeth 15 and 16 were excised due to the crushed alveolar bone and the maxillary sinus’s anterior wall. Tooth 14 had previously been extracted through an orthodontic procedure.
Figure 1: Facial 3DCT image at the time of initial treatment. The right maxilla has a crushed fracture. The upper right canine is dislocated and invaginated, and the upper right second premolar and first molar are invaded into the crushed bone. The right mandible has a depressed fracture, and the fracture line crosses the mental foramen.
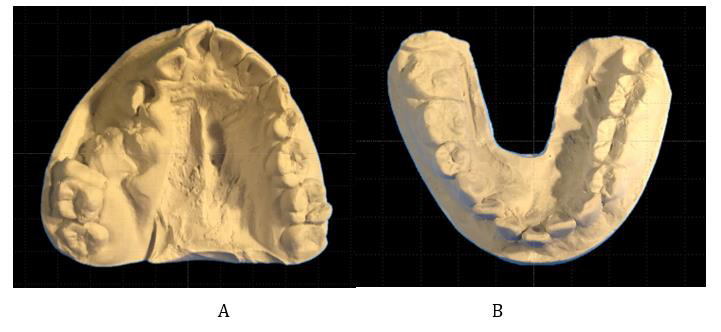
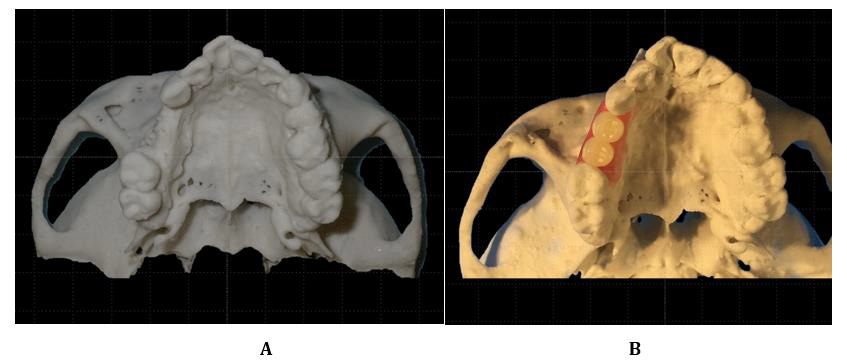
Figure 2: Examination models of the upper and lower dentitions.
A. The right maxillary dentition is displaced medially with loss of continuity. The upper right canine is dislocated, and the second premolar and first molar have deviated from the dentition. The right mandibular dentition is laterally displaced.
B. Model surgery was performed before the first surgery to clarify the posttreatment dentition imaging.
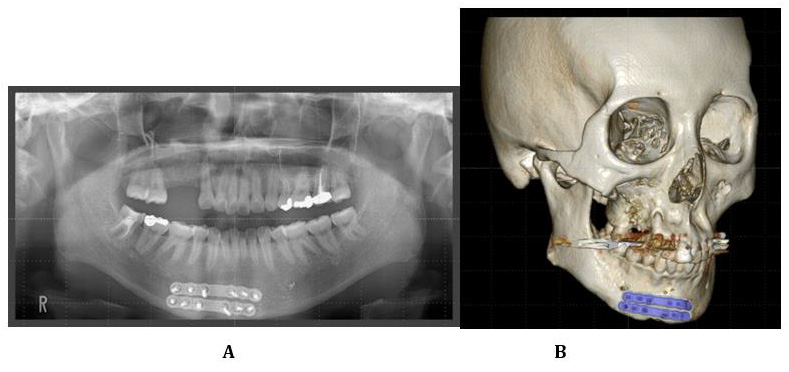
Figure 3: Radiographic images were obtained 6 months after open reduction and fixation.
A. Orthopantomograph showing the reduction of the upper right canine and its retention within the dentition.
B. 3DCT photograph demonstrating the healing of the fracture line after reduction and fixation with two titanium plates.
The mandibular fracture underwent open reduction and fixation using a titanium plate (Figures 3a & 3b). For the simulation and planning of the second surgery, we used CT digital data, its 3D plastic model, and a set up dentition model with the occlusal reconstruction. A close examination of the CT data revealed that the fractured tooth root remained in the bone and interfered with implant treatment. As the length of the dentition defect was atypical, the prosthesis decided was two premolars larger than the premolars on the healthy side. The amount of periodontal tissue deficiency was visualized by superimposing the set up dentition model with the 3D modeling model (Figures 4 & 5). Six months after the first operation, the second operation was performed for bone augmentation for the maxillary alveolar atrophy and mandibular mini-plate removal. Simultaneously, with the removal of the remaining tooth root at right maxillary, a 40 x 20mm cortical osteotomy was performed on the chin cortical bone from which the mandibular mini-plate had been removed. Half of the chin bone (20 × 20mm) was veneer grafted, and the other was crushed and filled in the gaps using titanium mesh (Figures 6a & 6b). There was no paresthesia in the anterior teeth of the mandible after bone collection. The patient underwent a third operation six months later. Due to trauma and the previous surgery, the scar on the tooth defect’s alveolar mucosa was visible, and the oral vestibule was narrowed. Non-mobile keratinized mucosa were required in the alveolar ridge mucosa of the dentition. Thus, vestibulopathy using atelocollagen was performed when the titanium mesh was removed. Two dental implants (Xive dental implants from DENTSPLY, Mannheim GERMANY) were placed on the alveolar ridge after the healing of the mucosa (4 months after vestibulopathy). The second-stage surgery was performed three months later, wherein the attached gingiva at the alveolar crest was extended to the oral vestibular side to obtain keratinized gingiva around the dental implant (Figure 7). The provisional restoration was used to harmonize the crown form and gingival morphology, and the final superstructure was attached about three years after the injury. The patient was fully satisfied with the aesthetic and functional properties. She responded to a maintenance system every 4-6 months and has maintained her oral hygiene with no signs of peri-implantitis (Figure 8).
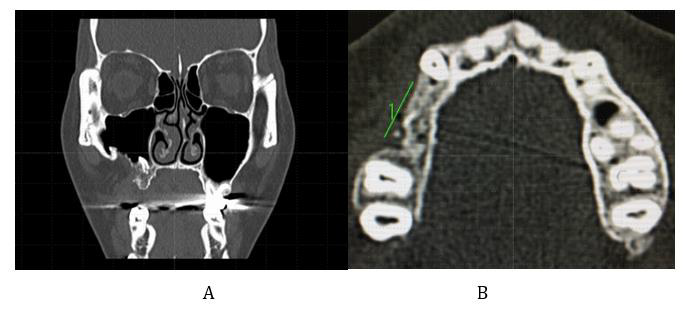
Figure 4: CT views of the jaws.
A. The coronal view shows that the fractured root of the upper right first molar within the bone is retained. The amount of alveolar bone required for dental implant placement is insufficient in terms of both height and width.
B. In the axial view, the length of the alveolar at the tooth loss was atypical. It was revealed that the premolars on the opposite side had 2.5 to 3 teeth.
Figure 5: The 3D model.
A. The maxillary 3D model’s occlusal view shows that the alveolar ridge of the upper right premolar is narrow, and implants cannot be placed.
B. Simulation of periodontal tissue in harmony with the prosthesis. The insufficient height and width of the periodontal tissue in the premolar region are clear. The size of the prosthesis was decided to be equal to that of two large premolars.
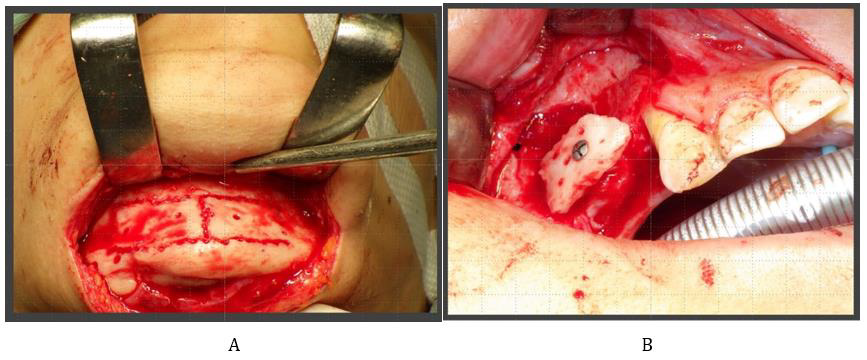
Figure 6: Surgerical view at the time of bone graft
A. Surgical field from which the titanium plate that was used to fix the mandibular fracture was removed. The cortical bone of the chin was osteotomized at 40 × 20mm.
B. One cortical bone (20 × 20mm) was veneer grafted to provide bone width and height. The other graft was crushed and filled within the veneer graft gaps and shaped with a titanium mesh.
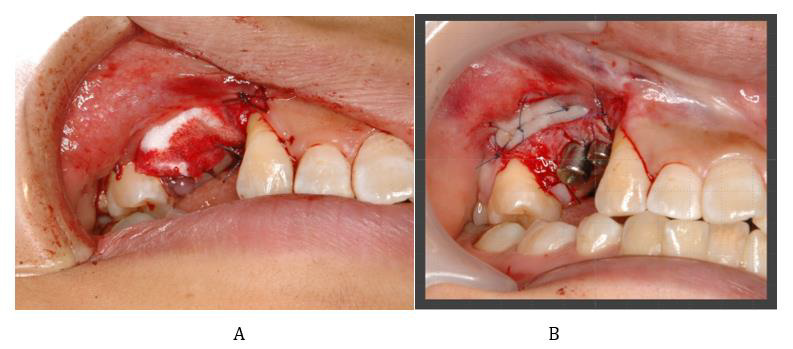
Figure 7: Periodontal plastic surgery was performed twice to obtain the attached keratinized mucosa.
A. Vestibuloplasty using atelocollagen was performed at the same time when the titanium mesh was removed.
B. The keratinized alveolar mucosa was moved apically when the second procedure was performed.
Figure 8: Results of the treatment.
A. Image showing the intraoral frontal view.
B. Image showing the intraoral occlusal view. The final prosthesis was fitted according to the treatment plan. The fixed implant prosthesis was supported by the keratinized mucosa and maintained in a favorable environment. Two years have passed since the last prosthesis was attached, and no peri-implantitis was observed.
C. Orthopantomograph 2 years after the superstructure was attached. No bone resorption was observed around the implant body.
Discussion and Conclusion
High-energy trauma often involves maxillofacial and dental trauma. Traumatic injuries results in loss of jaw continuity, anatomical defects in alveolar hard and soft tissues, and tooth loss [1]. Maxillofacial dental implant treatment enables aesthetic and functional recovery of occlusal and masticatory dysfunction associated with tooth and alveolar bone defects [2,3]. This reconstruction process requires multiple surgeries to treat jaw fractures and implants. There are several benefits to having a maxillofacial surgeon perform oral reconstruction under a series of treatment plans. An important outcome of maxillofacial fractures is the restoration of midface symmetry and mandibular continuity. It is important to follow evidence-based treatment strategies for good results in maxillofacial fracture treatment [4]. Occlusal reconstruction is one of the greatest themes of treatment of the stomatognathic region. For implant-based occlusal reconstruction to be most effective over a long-term period, the implant structure must be placed in the proper position and the keratinized oral mucosa should have adequate thickness around the implant [5]. Recent 3D digital image treatment plans for preoperative diagnosis are interesting. If the maxillofacial surgeon plans bone and tissue augmentation that assumes the proper placement of the implant structure, the patient may be able to reintegrate into society with fewer surgeries and treatment periods. The minimum bone width and height of the alveolar ridge for dental implantation must be >5mm and >10mm, respectively [6]. Reports on the use of distraction osteogenesis, autologous bone grafting [7], titanium mesh tray, and iliac particulate cancellous bone and marrow transplantation (Ti- MESH method) [8,9] for bone defects have been published in the literature. The advantage of distraction osteogenesis is that the soft tissue can concurrently be expanded; however, the dynamic treatment period of several months is a major drawback.
In the Ti-MESH method, the biggest concern is the surgical invasion of the donor site. Expected results may not be obtained due to the titanium mesh’s adverse events (tray exposure and increased risk of infection) and remodeling resorption, leading to loss of the graft [10,11]. Autologous bone grafting, which has excellent bone formation ability, is the gold standard for bone regeneration. Bone grafting is considered optimal for complex and extensive bone loss due to trauma. The outcome of bone grafting is said to be influenced by the donor’s structure, developmental pattern, and anatomical site [12]. Bone graft planning requires consideration of 10%–20% of bone resorption [13]. It has been reported that the amount of the grafted bone absorbed is less generated through intramembranous ossification in the mandible than generated through endochondral ossification as observed in the iliac crest [14,15]. The highly calcified chin bone helps to make an early transition and is useful for providing the primary stability for the dental implants [15,16]. Typical donor sites in the oral cavity are chin, mandibular ramus, and maxillary tuberosity. The advantages of intraoral bone collection are that the surgical approach is easy, no separate surgical intervention is required for bone collection, and the close proximity of the donor to the recipe site can reduce surgical time. On the other hand, it is impossible to collect a large amount of bone. Common postoperative symptoms of chin bone graft include hypoesthesia and paresthesia of the anterior teeth of the mandible [17,18]. In this case, cortical chin bone was selected because it could be collected from the same surgical field at the same time. Alveolar bone grafting for an atrophic alveolar segment is ideal in iliac crest bone graft due to its abundant supply, but chin bone grafting is an option for localized alveolar bone defects in 2-3 teeth.
The keratinized mucosa in the alveolar ridge is often lost along with the alveolar bone following a jaw fracture. Alternatively, a scarred mucosa remains after several surgical procedures. The mobile non-keratinized mucosa around the dental implant is more likely to cause peri-implantitis [19]. Also, the development of a mucosal scar with poor blood flow is disadvantageous for bone formation. The presence of keratinized mucosa around the dental implants affects the long-term prognosis of the implant treatment [20]. Therefore, vestibuloplasty and free gingival grafts to acquire a keratinized mucosa [21] are required. The palatal mucosa or atelocollagen is effective as a recipient of mucosal grafts [22,23]. It is important to ensure that a keratinized mucosa (of 2mm) is present around the dental implant. At present, it is unclear when the periodontal mucosa should be treated [24]. The apically positioned flap technique is often performed at the same time as the secondary operation. However, oral mucosal defects after maxilla-orofacial trauma may require mucosal management before implant placement. For patients with severe facial fractures, strict adherence to a well-established and structured treatment protocol based on surgical experience provides an efficient, appropriate, and successful treatment. Furthermore, superior results for severe traumatic maxilla-orofacial injuries will be achieved if the treatment is combined with efficient occlusal reconstruction.
Declarations
Ethics Approval and Consent to Participate
This study was conducted following the World Medical Association’s ethical guidelines, as described in the Declaration of Helsinki released in 2013.
Consent for Publication
The patient provided written informed consent for publication of this case report and any accompanying images.
Availability of Data and Materials
The datasets generated and/or analyzed during the current study are not publicly available due to inconsistent language expression but are available from the corresponding author upon reasonable request.
Competing Interests
The authors declare that they have no competing interests.
Funding
This research did not receive any specific funding from public, commercial, or not-for-profit agencies.
Authors’ Contributions
All authors have made substantial contributions to the conception and design of the study. KA and GU, YA and CK, and TK and TO have been involved in data collection, analysis, and interpretation respectively. TK drafted the manuscript. All authors revised the manuscript critically and have read and approved the final version of the manuscript.
Acknowledgement
The authors would like to thank Enago (www.enago.jp) for the English language review.
References
- Kanno T, Sukegawa S, Nariai Y, Tatsumi H, Ishibashi H, et al. (2014) Surgical treatment of comminuted mandibular fractures using a low-profile locking mandibular reconstruction plate system. Ann Maxillofac Surg 4(2): 144-149.
- Ormianer Z, Piek D, Livne S, Lavi D, Zafrir G, et al. (2012) Retrospective clinical evaluation of tapered implants: 10-year follow-up of delayed and immediate placement of maxillary implants. Implant Dent 21(4): 350-356.
- Pjetursson BE, Asgeirsson AG, Zwahlen M, Sailer I (2014) Improvements in implant dentistry over the last decade: comparison of survival and complication rates in older and newer publications. Int J Oral Maxillofac Implants 29: 308-324.
- Audigé L, Cornelius CP, Ieva AD, Prein J, CMF Classification Group (2014) The first AO classification system for fractures of the craniomaxillofacial skeleton: rationale, methodological background, developmental process, and objectives. Craniomaxillofac Trauma Reconstr 7(1): S006-S014.
- Gellrich NC, Rahlf B, Zimmerer R, Pott PC, Rana M (2017) A new concept for implant-borne dental rehabilitation; how to overcome the biological weak-spot of conventional dental implants? Head Face Med 13(1): 17.
- Kataoka T, Akagi Y, Kagawa C, Sasaki R, Okamoto T, et al. (2019) A case of effective oral rehabilitation after mandibular resection. Clin Case Rep 7(11): 2143-2148.
- Aghaloo TL, Moy PK (2007) Which hard tissue augmentation techniques are the most successful in furnishing bony support for implant placement? Int J Oral Maxillofac Implants 22: 49-70.
- Iino M, Shimizu H, Kasahara H (2000) Alveolar ridge augmentation using autogenous iliac cancellous bone graft combined with Micro-Titanium Augmentation Mesh and subsequent dental implant insertion. Asian J Oral Maxillofac Surg 12(1): 187-194.
- Yamada H, Nakaoka K, Horiuchi T, Kumagai K, Ikawa T, et al. (2014) Mandibular reconstruction using custom-made titanium mesh tray and particulate cancellous bone and marrow harvested from bilateral posterior ilia. J Plast Surg Hand Surg 48(3): 183-190.
- Louis PJ, Gutta R, Said Al Naief N, Bartolucci AA (2008) Reconstruction of the maxilla and mandible with particulate bone graft and titanium mesh for implant placement. J Oral Maxillofac Surg 66(2): 235-245.
- Kumar BP, Venkatesh V, Kumar KA, Yadav BY, Mohan SR (2016) Mandibular reconstruction: overview. J Maxillofac Oral Surg 15(4): 425-441.
- Hassani A, Khojasteh A, Shamsabad AN (2005) The anterior palate as a donor site in maxillofacial bone grafting: A quantitative anatomic study. J Oral Maxillofac Surg 63(8): 1196-1200.
- Aghaloo TL, Moy PK (2007) Which hard tissue augmentation techniques are the most successful in furnishing bony support for implant placement? Int J Oral Maxillofac Implants 22: 49-70.
- Koole R, Bosker H, van der Dussen FN (1989) Late secondary autogenous bone grafting in cleft patients comparing mandibular (ectomesenchymal) and iliac crest (mesenchymal) grafts. J Craniomaxillofac Surg 17(1): 28-30.
- Mish CM, Mish CE, Resnik RR, Ismail YH (1992) Reconstruction of maxillary alveolar defects with mandibular symphysis grafts for dental implants: a preliminary procedural report. Int J Oral Maxillofac Implants 7(3): 360-366.
- Turkyilmaz I, McGlumphy EA (2008) Influence of bone density on implant stability parameters and implant success: a retrospective clinical study. BMC Oral Health 8: 32.
- Clavero J, Lundgren S (2003) Ramus or chin grafts for maxillary sinus inlay and local onlay augmentation: comparison of donor site morbidity and complications. Clin Implant Dent Relat Res 5: 154-160.
- Hunt DR, Jovanovic SA (1999) Autogenous bone harvesting: a chin graft technique for particulate and monocortical bone blochs. Int J Periodontics Restorative Dent 19(2): 165-173.
- Gobbato L, Avila Ortiz G, Sohrabi K, Wang CW, Karimbux N (2013) The effect of keratinized mucosa width on peri-implant health: a systematic review. Int J Oral Maxillofac Implants 28(6): 1536-1545.
- Ladwein C, Schmelzeisen R, Nelson K, Fluegge TV, Fretwurst T (2015) Is the presence of keratinized mucosa associated with periimplant tissue health? A clinical cross-sectional analysis. Int J Implant Dent 1(1): 11.
- Padhye NM, Mehta LK, Yadav N (2020) Buccally displaced flap versus sub-epithelial connective tissue graft for peri-implant soft tissue augmentation: a pilot double-blind randomized controlled trial. Int J Implant Dent 6(1): 48.
- Tavelli L, Barootchi S, Ravidà A, Oh TJ, Wang HL (2019) What Is the Safety Zone for Palatal Soft Tissue Graft Harvesting Based on the Locations of the Greater Palatine Artery and Foramen? A Systematic Review. J Oral Maxillofac Surg 77: 271.
- Xu C, Wang QT, Chen J, Wu Y, Zhao L (2019) Collagen matrix for periodontal plastic surgery procedures: a meta-analysis update. Int J Periodontics Restorative Dent 39(4): e129-e155.
- Baltacıoğlu E, Bağış B, Korkmaz FM, Aydın G, Yuva P, et al. (2015) Peri-implant plastic surgical approaches to increasing keratinized mucosa width. J Oral Implantol 41(3): e73-e81.

 Case Report
Case Report