ABSTRACT
The anterior access route for surgical treatment of pathologies of the lumbar spine is indicated, given its advantages over the classic posterior approach. We also see the improvement in surgery access and better technology in implants. This study assesses a restraint device placed on the vertebral body to prevent migration of arthroplasty and lumbar inter somatic devices. The instrument has a low cost and promotes additional support as the last lock. We selected 89 patients with low back pain due to degenerative disc disease refractory to clinical treatment who required surgery, arthroplasty, and anterior arthrodesis. The use of cancellous screw with large fragments – 6.5 mm, with washer does not affect bleeding and surgical time. With more than ten years of executing this procedure, Marcondes and Dias advise its use for ALIF Stand Alone in two levels or more and all arthroplasty cases in one or two levels.
Keywords: Lumbar Spine; Arthrodesis; Arthroplasty
Introduction
The anterior approach technique to treat lumbar spine pathologies had a high rate of complications in the past, such as bleeding, retroperitoneal injury, retrograde ejaculation, and implant migration. [1-3] With the new implants, retractors, and trained access surgeons, we observed an increase in the number of surgeries by anterior approach associated with a lower rate of complications [4,5]. The anterior access technique allows wide exposure of the intervertebral disc with a larger area of the arthrodesis. Besides, it increases intradiscal height, causing an indirect decompression of the nerve roots and lordosis gain, improving the biomechanics of the lumbar spine and providing a faster recovery in the patient’s postoperative period. [4-6] The anterior access route for the surgical treatment of lumbar spine pathologies has been increasing its indication, given its numerous advantages over the classic posterior approach, the improvement of the access surgeon, and the better evolution of implants [4]. Following this evolution, we observed a small incidence of anterior migration of the implants used. However, despite being a small number, they can lead to devastating complications for the patient due to the specific characteristics of the local anatomy [7]. For more than ten years, the same surgeon team of a spine clinic in Sao Paulo state, Brazil, has been working hard to improve the approach technique and minimize post-surgical complications in the patient. They have used a cancellous screw with a meager cost and provides additional stability as an anterior lock [1,5-7]. Thus, this study describes using a 6.5 mm simple cancellous screw placed on the lower vertebral plateau in the surgery spine segment to avoid anterior migration of arthroplasty and lumbar interbody implants.
Methods
We documented the clinical outcomes of 89 patients who underwent arthrodesis and arthroplasty performed by the same team of surgeons from a medical center in Sao Paulo, Brazil. The FMABC Ethics committee approved the study with the number 37120920.1.0000.0082. The data presented maintain the confidentiality of the patient’s identity.
Eligibility criteria
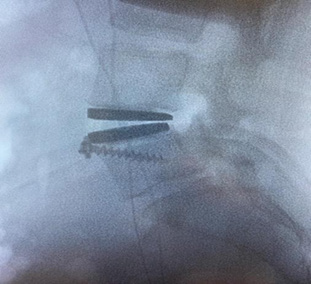
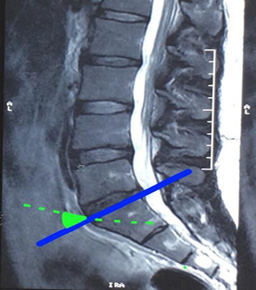
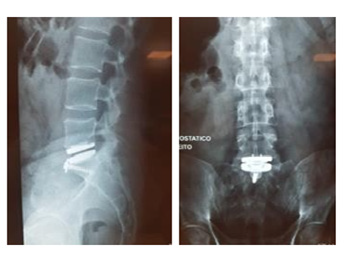
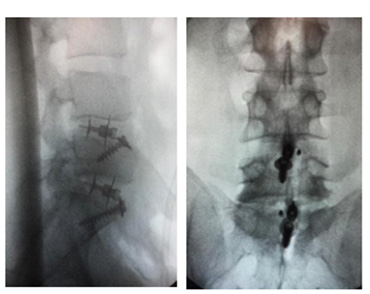
We selected patients who had pain in the lumbar region associated or not with irradiation to the lower limbs, with good bone quality confirmed by bone densitometry, calcium, and vitamin D metabolism. The diagnosis was also confirmed by traditional tests such as magnetic resonance imaging for specific etiologic diagnosis, dynamic radiography to assess the flexibility of the lumbar region, and the presence or absence of segmental instability. Electroneuromyography to document the presence of preoperative radiculopathy and possible pre-existing neurological deficits. In both techniques, arthrodesis, and arthroplasty, patients with indications for surgical treatment are refractory to clinical therapy for more than one year. For anterior arthrodesis, we included patients with degenerative lumbar disc disease between the L3- L4 levels; L4-L5; L5-S1 in patients over 60 years old, patients who have moderate to severe facet arthrosis, gross instability, previous surgery approached via a posterior approach and as a complement to 360° arthrodesis. We excluded patients with minimal or no degree of arthrosis of the facet joint without evidence of spondylolisthesis or pars defect. In the case of arthroplasty, we included patients aged between 20 and 55 with low back pain with or without irradiation to the leg who had failed conservative treatment for more than one year. They confirmed the diagnosis of degenerative disc disease by magnetic resonance imaging [8]. We excluded patients with significant or symptomatic facet disease, degenerative spondylolisthesis > 3 mm or pars defect, osteoporotic disease, and previous anterior or posterior lumbar fusion. Individuals with bone involvement such as infection or tumor and conditions that would be against indication for surgery were also excluded [8]. The primary implants used in the surgical interventions described in this analysis are Intersomatic CAGE (Double Locking Cage ALIF (Figure 1); Thoracolumbar Interbody Fusion Kili (Figure 2); M6-L Artificial Lumbar Disc (Figure 3), and the Cannulated Screw (Figure 4).
Surgical Procedure
After placing the lumbar disc prosthesis or inter somatic CAGE, it is necessary to minimize the migration risk of these implants, using a screw to reinforce anterior stability. [9] To place the screw, we performed a bone tunnel with a 3.2 mm drill or a Stillman wire (bone tunnel performed manually with an orthopedic hammer without using a drilling machine) centered on the body’s midline and the apex of the lower vertebral plateau of the instrumented level. We followed the anterosuperior direction from the vertebral plateau to the posteroinferior monocortical region, as shown in Figure 5. At the time of bone drilling, we used the ‘’C’’ arm of the radioscopy directed in anteroposterior to identify the vertebral body midline and handled to aid in the depth of the drill or Stillman wire insertion not to invade the opposite cortex and the endplate. [9,10] We considered slight variations of 10° to 15° of angulation acceptable and minor changes in the entry point in the anterolateral direction. Some access surgeons prefer to place the screw 5 to 10 mm lateral to the midline at the levels of l3-l4 and l4-l5 to avoid possible protrusions under the inferior vena cava. To introduce the cancellous screw with washer into the body of the first sacral vertebra (S1), we used the 70° angle concerning the upper plateau of the body of S1 due to its trapezoidal anatomy (Figure 6). [9,10] After the bone tunnel, we measured the screw with the conventional gauge of the large fragment box that varies between 25 mm to 40 mm, followed by the tapping of 6.5 mm and then the insertion of the cancellous screw total thread of 6.5 mm with washer under fluoroscopy control as seen in Figure 7. The screw works as a locking tool to prevent the anterior migration of the instrumented material performed by locking the washer (Figure 8).
Results
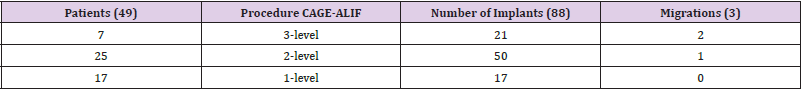
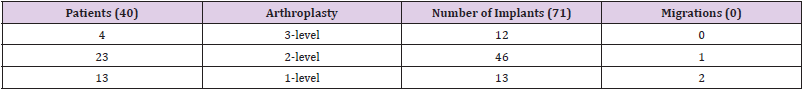
Of the total patients (89) who underwent surgery, 49 were treated by the Anterior Lumbar Interbody Fusion (ALIF) technique, and the other 40 by arthroplasty. Table 1 shows the frequency of patients who underwent ALIF. Three of them suffered migration of the implants, one case in a Stand-Alone approach to 2 levels of instrumentation and two migrations of Stand Alone in 3 levels instrumented. The patients who underwent arthroplasty (40 patients and 71 implants) were performed with stabilization of the ‘’Cancellous Screw with Washer’’. Three patients presented complications related to implant migration, as illustrated in Table 2.
Discussion
Out of the 89 patients who underwent surgery, six (6,7%) experienced implant migration. The complications with anterior arthroplasty occurred among the first patients who underwent the surgical intervention. The clinical team has discussed it profoundly and thinks that perhaps its short experience with those implants could affect the outcome. We also have managed the hypothesis that the complications of anterior arthroplasty migration were even more related to problems inherent to the patient and the medical indication than to the surgical technique and the implant used. Furthermore, we believe the complications were caused by: a) A significant fracture of the upper vertebral plateau of the instrumented lower vertebra, possibly due to inadequate indication of the procedure, as the patient was over 55 years old. Late plateau fracture (35 days postoperatively) evolved with instability and anterior expulsion of the implant.
b) An anterior migration due to segmental instability was only identified intraoperatively in a patient with a large extruded herniated disc, treated anteriorly for decompression and arthroplasty, followed by a posterior microsurgical approach to review the spinal canal. Segmental instability was diagnosed in the posterior approach, and it was no longer possible to change the technique for arthrodesis of this segment. We waited for the postoperative evolution, with implant migration after falling from its height on the 21st postoperative day.
c) A prior migration was due to the patient’s previous obesity, her initial refusal to perform lumbar arthrodesis, and her inability to lose weight during the first 60 postoperative days. She evolved with anterior migration of the implant 61 days after surgery, after a minor fall from its height.
It is worth noting that anterior migration, both the ALIF and the arthroplasty, can cause arterial compression, venous compression, or compression of the right or left ureters. Depending on the level accessed during surgery, arteriovenous compression can compress the aorta, the vena cava, or the iliac arteries and veins. Arterial compression can progress to acute arterial occlusion accompanied by tissue ischemia, or subacute partial arterial compression, with consequent vascular claudication. Venous compression can cause total venous occlusion with deep vein thrombosis. It can trigger pulmonary embolism and death, where a partial venous compression with hemodynamic involvement of more than 70% of the vessel lumen will start venous stasis and chronic venous insufficiency. Concerning extrinsic compression of the ureters by the migrated implant, post-renal acute failure could lead to renal failure. It occurred in cases of total obstruction; or dilation of the ureter and pyelocaliceal system due to a ureter partial block, with consequent chronic renal failure. Resolute treatment for chronic low back pain due to degenerative disc disease (DDD) is challenging and controversial. According to the Visual Analogue Scale and Oswestry Scale [The Oswestry Disability Index (ODI)] there has been a significant improvement in performing surgical treatment with anterior arthrodesis at 1 to 2 levels for patients with more than six months of clinical therapy due to DDD [8].
After the complications of the initial learning curve of the use of the lumbar arthroplasty technique, it was decided to combine the ‘’Cancellous Screw with Washer’’ with the arthroplasty technique in all other subsequent patients, totaling 30 more patients with implantation of M6-L arthroplasty, without any case of subsequent migration. From a historical point of view, there is evidence that the cancellous screw was used as a retaining device for the iliac crest or femoral diaphysis graft in inter somatic arthrodesis performed via the anterior approach. We observed that it did not follow a pattern of insertion, positioning, size, or angulation for its purpose. There was not a protocol for its usage [9]. Because of these circumstances, and in the absence of a clinical protocol, surgeons Marcondes and Dias have implemented and mastered the screw reinforcement technique to avoid the risk of displacement of the implants in spinal surgeries. With an experience of more than ten years of performing this procedure, these doctors have accumulated evidence of the patients benefiting from this technique. This particular surgical approach of doctors Marcondes and Dias is known and recognized by the clinical community.
Intersomatic arthrodesis performed via the anterior approach has biomechanical advantages compared to posterior, oblique, or lateral approaches [1]. It is a considerably young procedure and has been increasingly adopted since 1960 [11]. Due to the direct access to the anterior spine, the intervertebral disc space is visualized, a complete discectomy is performed, and intervertebral spacers are implanted. It has resulted in an exponential growth in the number and variety of devices for the anterior lumbar approach over the last five years. [12,13] We know that 80% of the load is absorbed in the anterior portion of the spine, making instrumentation in this region essential when performing segmental arthrodesis. A literature review comparing the biomechanics of different approaches for inter somatic fusion (MIS TLIF expandable with conventional TLIF and ALIF) reported that the most rigid fixation in flexion-extension and axial rotation was ALIF associated with bilateral pedicle screw fixation. However, other studies tended to perform arthrodesis using an isolated anterior approach. Its advantage is shorter surgical time, less intraoperative bleeding, hospital stay reduction, and decreased complication, for example, pseudarthrosis rate varying around 6.5% and reoperation around 2.4% [10].
After arthrodesis surgery, we highlight the disc disease of the adjacent level as a late complication; its prevalence is still not well documented, making it one of the main criticisms in opposition to performing a movement-preserving surgery (total disc arthroplasty). Studies show increased stress on the facet joint and disc, causing high mobility at levels adjacent to the fused segments. In recent studies, we have observed a prevalence of symptomatic patients with degenerative disease of the adjacent level ranging from 5.2% to 18.5%, with instrumentation for arthrodesis, an extension of the fusion, iatrogenic sagittal balance, previous degenerative disc disease adjacent to arthrodesis and young patients with high functional demand [10]. Despite a limited sample of 89 patients analyzed in this study, there was a significant decrease in complications related to the migration of the Stand- Alone implant, both CAGE ALIF and total disc prosthesis, when supplementation of the anterior fixation with ‘’Cancellous Screw with Washer’’.
Studies report that the anterior approach has higher implant migration rates. With the removal of stabilizing structures of the anterior column associated with the lordotic anatomy of the lumbar spine, there is a greater probability of anterior migration of the implant in the postoperative period [10]. In the late patient’s follow-up, we observed that the screw does not change the mobility of the implant in the case of arthroplasties and does not result in a significant increase in the cost of the procedure. In addition, the anterior approach has been advocated due to the minimal formation of fibro-scar tissue, absence of trauma to the paravertebral musculature, and posterior ligament structures, with the main advantage being the gain of lumbar segmental lordosis and the recovery of sagittal alignment. [3,14-20] The current study showed the use of the ‘’ Cancellous Screw with Washer’’ in cases of double ALIF Stand Alone locks at two or more levels. In cases of Lumbar Arthroplasty, it can contain the need for a posterior approach and prevent complications from anterior implant migration.
Conclusion
The cancellous screw with large fragments - 6.5 mm, with washer is a low-cost fixation instrument, and its implantation does not affect bleeding and surgical time. With more than ten years of executing this procedure, Marcondes and Dias advise its use for ALIF Stand Alone in two levels or more, and all arthroplasty cases in one or two levels, considering the low cost and the prevention of anterior migration of the implant, decreasing the reoperation rate. The clinical team of Marcondes and Dias are currently carrying out a biomechanical study to deeply understand other aspects of the screw stabilizing effect.
References
- Choy Jie Wen, Hanna David Abi, Cassar Lachlan P, Philip Hardcastle, Kevin Phan, et al. (2019) Histoy of Integral Fixation for Anterior Lumbar Interbody Fusion (ALIF): The hastshill horseshoe. World Neurosurgery 129: 394-400.
- Bassani Roberto, Gregori Fabrízio, Peretti Giuseppe (2019) Evoluiton of The Anterior Approach im Lumbar Spine Fusion. World Neurosurgery 131: 391-398.
- Kerolus Mena, Turel Mazda K, Tan Lee, Deutsch Harel (2016) Stand- Alone Anterior Lumbar Interbody Fusion: Indications, techniques, surhical, outcomes and complications. Expert Review of Medical Devices 13(12): 1127-1136.
- Mobbs J Ralph, Phan Kevin, Malham Greg, Kevin Seex, Prashanth J Rao, et al. (2015) Lumbar Interbody Fusion: techniques, indications and comparison of intebody fusion option including PLIF, TLIF, MI-TLIF, OLIF/ATP, LLIF and ALIF. NeuroSpine Surgery Research Group 1(1):1-17.
- Moura Diogo Lino, Lawrence David, Gabriel Josué Pereira Artrodese Lombar Intersomática Anterior Multiníeis Combinada com Estabilização Posterior em Discopatia: Análise clínico-funcional prospective.
- Kapustka Bartosz, Kiwic Grzegorz, Paweł Chodakowski, Jan P Miodoński, Tomasz Wysokiński, et al. (2019) Anterior Lumbar Interbody Fusion (ALIF): Biometrical results and own experiences, Neurosurgical Review 43(2): 687-693.
- Rajaraman V, Vingan R, Roth P, Heary RF, Conklin L, et al. (1999) Visceral and vascular complications resulting from anterior lumbar interbody fusion. Journal of Neurosurgery: Spine 91(1): 60-64.
- Kleimer Jonh P, Cheng Ivan, et al. (2018) Fusão Intersomática lombar anterior seletiva para dor lombar associada à doença degenerative do disco versus tratamento não cirurgico. SPINE: 01 de outubro de 43(19): 1372-1380.
- Keith H Bridwell, Ronald L DeWald (1997) The Textbook of Spinal Surgery (2nd )., 12(94): 1995-1997.
- Cannestra Andrew F, Peterson Mark D, et. al. (2016) A Literature Review and Biomechanical Comparison of an Expandable MIS TLIF With Conventional TLIF and ALIF. SPINE 41: S44-S49.
- Li Y, Hao D, He B, Wang X, Yan L (2015) The Efficiency of Zero-profile Implant in Anterior Cervical Discectomy Fusion. Journal of Spinal Disorders and Techniques 28(10): 398-403.
- Phan K, Pelletier MH, Rao Pj, Choy Wj, Walsh Wr, et al. (2019) Integral fixation titanium/polyetheretherketone cages for cervical arthrodesis: Evolution of cage design and early radiological outcomes and fusion rates. Orthopaedic surgery 11(1): 52-59.
- Giang G, Mobbs R, Phan S, Tran TM, Phan K (2017) Evaluating outcomes of stand- alone anterior lumbar interbody fusion: a systematic review. World Neurosurgery 104: 259-271.
- Jaeger Antoine, Gilber David, Bastard Claire, Benjamin Thiebaut, François Roubineau, et al. (2019) Risk Factors of Instrumentation Failure and Pseudarthrosis After Stand-Alone L5-S1 Anterior Lumbar Interbody Fusion: A retrospective cohort. Neurosurg Spine 31(3): 388-346.
- Salvador A Brau FACS: Anterior Access to The Lumber Spine: Mini- open, retropertironeal approach.
- Choy W, Barrington N, Garcia RM, Kim RB, Rodriguez H, et al. (2017) Risk factors for medical and surgical complications following single-level ALIF. Global Spine Journal 7(2): 141-147.
- Goz V, Weinreb JH, Schwab F, Lafage V, Errico TJ (2014) Comparison of complications, costs, and length of stay of three different lumbar interbody fusion techniques: an analysis of the Nationwide Inpatient Sample database. The Spine Journal 14(9): 2019-2027.
- Rao PJ, Loganathan A, Yeung V, Mobbs RJ (2015) Outcomes of anterior lumbar interbody fusion surgery based on indication: a prospective study. Neurosurgery 76(1): 7-24.
- Teng I, Han J, Phan K, Mobbs R (2017) A meta-analysis comparing alif, plif, tlif and llif. Journal of Clinical Neuroscience 44: 11-17.
- Oxland TR, Hoffer Z, Nydegger T, Rathonyi GC, Nolte L P (2000) A comparative biomechanical investigation of anterior lumbar interbody cages: central and bilateral approaches. JBJS 82(3): 383-393.

 Case Report
Case Report