Abstract
Endometrial polyp, being one of the most common causes of abnormal uterine bleeding, is formed from localized overgrowths of endometrial tissue brought about by increased estrogen levels. Sizes of polyps usually are less than 2cm, while those >4 cm are labeled as giant polyps. Such polyps can even occupy the entire endometrial cavity, making complete hysteroscopic removal difficult and prone to failure and morbidity. Limited literature regarding use of GnRH agonist in endometrial polyps are published but given the idea that it induces a state of hypoestrogenism, it could be a promising approach for neoadjuvant treatment in such cases. In this paper, 3 cases of giant endometrial polyps with fertility problems were given GnRH agonists prior to resection. All cases have shown significant decrease in size of their polyps, making complete and successful hysteroscopic removal feasible.
Keywords: Giant Endometrial Polyp; GnRH Agonist; Hysteroscopic Removal
Introduction
Endometrial polyp is one of the most common structural causes of abnormal uterine bleeding in the reproductive age group. It arises from endometrial overgrowth brought about by a hyper-estrogenic state. Polyps are usually around 2cm in size, and those greater than 4cm are labeled as giant polyps. The cases presented are women in the reproductive age group with fertility problems, having endometrial polyps as large as 10cm occupying the whole uterine cavity, even prolapsing out of the endocervical canal. Conservative management was recommended but due to their size, immediate hysteroscopic removal may not be attainable due to expected difficulty in distending the uterine cavity and possible morbidities like fluid overload and uterine perforation. Although with limited studies, GnRH agonists have been proposed as a neoadjuvant treatment prior to hysteroscopic removal of giant polyps. Given the same mechanism applied with GnRH agonist’s use with myomas, it induces a hypoestrogenic environment at the same time decreasing the vascularity of the endometrial lining that will help significantly decrease the size of the giant polyps, making hysteroscopic removal feasible
Case Report
Case 1
This is a case of Abnormal Uterine Bleeding (AUB) in a 29-yearold,
single, nulligravid from Laguna. The patient has unremarkable
past medical and family history. She is living in with her 3-year
partner and is desirous of pregnancy. Ever since menarche, patient
has been experiencing heavy menstrual bleeding soaking 2-3 baby
diapers per day, lasting 7-14 days, with no associated symptoms. She was hospitalized at the age of 16 for blood transfusion due to
chronic blood loss brought about by heavy menstrual bleeding.
Blood dyscrasia was ruled out. At the age of 20, she consulted a
government hospital still for persistent heavy menstrual bleeding
now associated with dyspareunia and post-coital vaginal bleeding.
She was assessed with a cervical mass probably polyp and
underwent fractional curettage and polypectomy, which on biopsy
revealed polyp. Patient continue to have occasional heavy menstrual
bleeding however few months prior to consult in our institution,
she had continuous profuse vaginal bleeding, this time associated
with an enlarging abdomino-pelvic mass. She was assessed with
cervical cancer due to a finding of irregularly shaped cervical mass.
A cervical punch biopsy was done which only revealed granulation
tissue. She was then referred to our institution for further work up
and management.
When we first saw the patient, she was pale but with stable
vital signs. Speculum examination revealed a polypoid fleshy
mass occupying the upper half of the vaginal canal. On internal
examination, patient had a polypoid fleshy mass measuring 8cm x
10cm x 10cm occupying the upper vaginal canal and the cervix was
difficult to palpate. The corpus was enlarged to 18-20 weeks size.
She was initially diagnosed as a case of to consider cervical cancer
and was admitted for blood transfusion and work up. Cervical punch
biopsy was repeated and it revealed necrotic and hemorrhagic
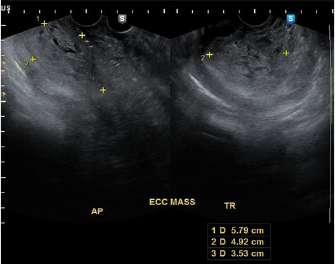
polypoid lesion. Transvaginal ultrasound done noted an aggregate
of polyps at the cervix that arise from the endometrial cavity with
attachment at the fundus. Impression was endometrial mass, to
consider endometrial pathology with extension to less than 50% of
the myometrium, endocervical canal, and lower third of vagina (See
Appendix 1, Figure 1). Current working diagnosis was changed to
AUB secondary to endometrial mass probably endometrial polyp.
Patient was referred to our section for possible hysteroscopic
polypectomy. But due to the size of the mass and expected technical
difficulty for hysteroscopic removal, we advised pre-treatment with
Gonadotropin-Releasing Hormone (GnRH) agonist to be given for 3
to 6 doses every 28 days prior to surgery.
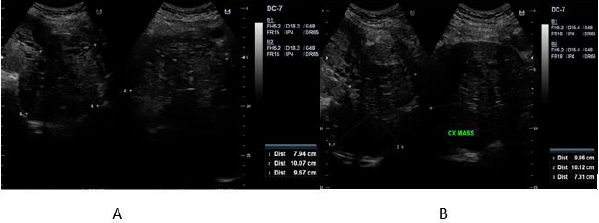
Apendix 1 Figure 1: Endometrial mass and prolapsing cervical mass arising from the endometrium prior to GnRH agonist.
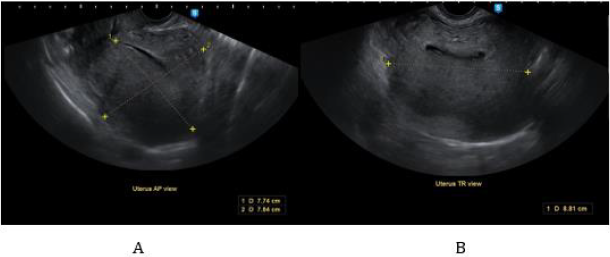
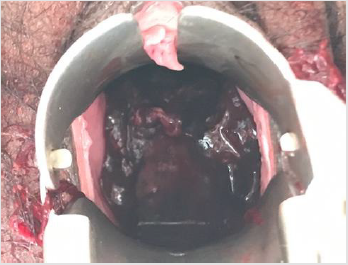
After three doses of GnRH, repeat internal examination showed that the polypoid mass within the vaginal canal disintegrated and was easily removed from its attachment. Patient noted minimal vaginal bleeding with passage of meat like material, probably fragments of the polyp. The corpus size also decreased to 14 to 16 weeks size, from the initial 18-20 weeks size. Additional 3 doses of GnRH agonist were suggested to further decrease the size of the mass and make the hysteroscopy easier. After 6 doses of GnRH agonists with a corpus size of 10-12 weeks, the patient then underwent hysteroscopic polypectomy. Intraoperatively, the polypoid mass was soft and hemorrhagic, but was not friable and non-necrotic, with an aggregate diameter of 17 cm (See Appendix 1, Figures 2 & 3). Cut section revealed multiple cystic spaces all throughout the mass. Final biopsy report showed mixed endocervical-endometrial polyp. Three months post-surgery, there was no recurrence of heavy menstrual bleeding and repeat ultrasound revealed normal uterus with thin endometrium (See Appendix 1, Figure 4). Currently, the patient is already 1 year post op with no recurrence of the heavy menstrual bleeding and is currently for infertility management.
Apendix 1 Figure 2: Endometrial mass and prolapsing cervical mass arising from the endometrium prior to GnRH agonist.
Apendix 1 Figure 3: Endometrial mass and prolapsing cervical mass arising from the endometrium prior to GnRH agonist.
Case 2
This is another case of AUB in a 30-year-old, Gravida 2 Para
0 (0020), married, from Mindoro. She has no co-morbids and
had 2 previous spontaneous abortions at 12 weeks AOG. She is
currently living with her husband of 10 years and is desirous of a
successful pregnancy. Four years prior to consult in our institution,
patient experienced heavy menstrual bleeding for 7 days, soaking
3 baby diapers per day with blood clots. She was assessed with
AUB secondary to thickened endometrium and was admitted for
blood transfusion. After 2 years, patient again had recurrence of
heavy menstrual bleeding, this time associated with abdominal
enlargement. Ultrasound was done and showed myoma uteri. She
was again transfused with blood products and advised hysterectomy
but patient refused due to financial constraints and desire of future
fertility. 3 months prior to consult in our institution, patient again
experienced continuous vaginal bleeding and pain with pallor
and fatigue. She was rushed again to the local hospital and on
assessment, there was a polypoid mass occupying the vaginal canal
and was sampled for biopsy. The histopathology result revealed
atypical polypoid adenomyoma so the patient was referred to our
institution.
On our initial examination, the patient was pale but with stable
vital signs. Pelvic examination revealed a hemorrhagic polypoid
fleshy mass occupying the whole vaginal canal that easily bleeds
in manipulation measuring 6cm x 6cm (See Appendix 2, Figure 1).
The cervix was difficult to assess and the corpus was enlarged to
20-22 weeks size. Rectovaginal examination was unremarkable.
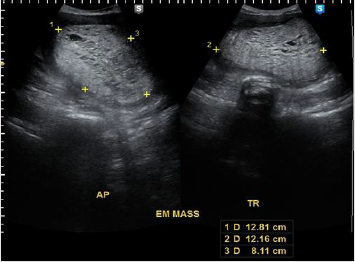
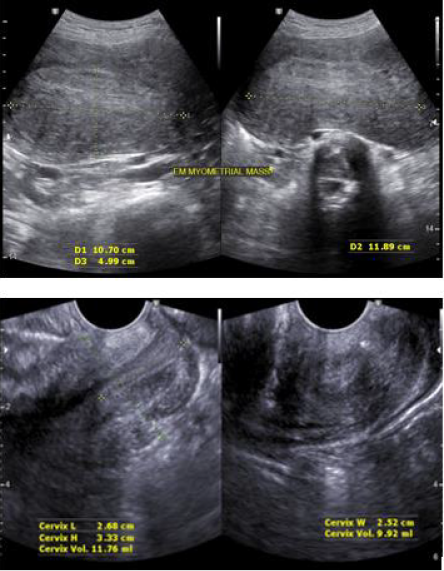
Transvaginal ultrasound was done which showed an echogenic
mass within the endometrial, endocervical and vaginal canal
measuring 12.8 x 12.2 x 8.1 cm with multiple irregular cystic
spaces, invading >50% of the posterior myometrium (See Appendix
2, Figure 2). The impression was endocervical and endometrial
masses consider atypical polyp with >50% myometrial invasion.
Repeat biopsy of the prolapsed endometrial mass was done which
revealed endometrial polyp. Patient was also referred to our section
for possible hysteroscopic polypectomy. But again, due to the size
of the mass and expected technical difficulty for hysteroscopic
removal, pre-treatment with GnRH agonist prior to surgery was advised. After 2 doses of GnRH, there was significant improvement
of patient’s symptoms, but with minimal vaginal bleeding, and
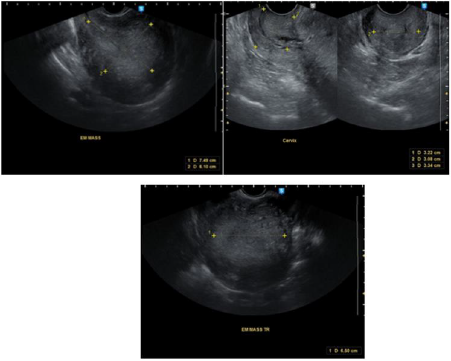
passage of meat-like materials. On internal examination, the
prolapsing endometrial mass decreased to 2x2cm (See Appendix
2, Figure 3) and the corpus size decreased to 16-18 weeks from the
initial 20-22 weeks size. Repeat ultrasound also noted a decrease
in the size of the endometrial mass to 10.7 x 11.8 x 5.0 cm (See
Appendix 2, Figure 4). After the 3rd dose of the GnRH, the patient
will be re-assessed if additional GnRH is needed or if already
amenable to hysteroscopic polypectomy.
Case 3
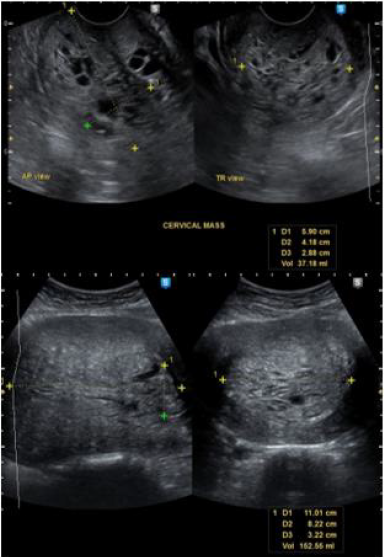
The last case is a 36-year-old, nulligravid who came in due to abdominal enlargement and inter-menstrual bleeding. Patient has no comorbid but is unable to conceive for 9 years with her husband. 1 year prior to consult, she began to develop intermenstrual bleeding, soaking 3 pads per day lasting 1-2 days associated with abdominal enlargement. On pelvic examination, there is a 3x3cm polypoid mass protruding out the endocervical canal, which seems to be coming from the endometrial cavity and the corpus is enlarged to 18-20 weeks size. Ultrasound showed an endometrial mass measuring 11.0 x 8.2 x 3.2cm with irregular cystic spaces and seems to be contiguous with the endocervical mass (See Appendix 3, Figure 1). Endometrial biopsy was done to rule out malignancy, and the result was endometrial polyp, hyperplastic type. Management was again GnRH for 3 doses and reasses if amenable for hysteroscopy. After her 1st dose of GnRH, the size of the corpus significantly decreased to 14 to 16 weeks size. Patient also reported fragments passage of meat-like material with minimal vaginal bleeding. Repeat ultrasound was done and the size also significantly decreased to 7.5 x 6.5 x 6.1cm (See Appendix 3, Figure 2). Patient is still for completion of 2 more doses of GnRH prior to re-assessment.
Discussion
Endometrial polyp is one of the most common structural
causes of AUB among the reproductive age group. It could present
as intermenstrual or heavy menstrual bleeding and the amount
of bleeding is usually proportional to the size of the endometrial
polyp: the larger the size, the more debilitating the symptoms.
Aside from bleeding, it is also associated with infertility just as the
cases presented. Endometrial polyps are formed from localized
overgrowths of endometrial tissue composed of variable amount
of glands, stroma, and blood vessels covered by epithelium. The
stroma of a polyp is composed of fibroblast like spindle cells and
large blood vessels with thick walls. Commonly, the size of a polyp
is less than 2cm, however, polyps greater than 4 cm are called giant
polyps, as shown in the cases above, whose sizes range from 10 to
12 cm. The development of endometrial polyps has been explained
by a number of molecular mechanisms such as monoclonal
endometrial hyperplasia, over-expression of endometrial
aromatase and gene mutations [1]. It usually arises because of
estrogen hypersensitivity in some areas of the endometrium,
probably caused by hyperactivation of the beta or the alpha
estrogen receptor during the first phase of the cycle. Furthermore,
they do not shed with menstruation because the estrogen related
inflammation block the apoptosis via bcl-2 gene expression. Giant
polyps, on the other hand are known to occur due to unbalanced
estrogen levels. This estrogen related polyp growth occurs due to
angiogenic growth factors’ deregulation, produced under hormone
control inside the polyp, within a short time and few cycles [2].
Histopathological examination must be performed on all
resected polyps to rule out endometrial polyps (0.5%–3%) with
malignant foci. Lasmar BP reported that endometrial polyps larger
than 15 mm are associated with hyperplasia and Wang J et al.
identified that polyps measuring more than 10 mm are associated
with malignancy [3]. The 3 cases of giant polyps presented all
underwent endometrial biopsy to rule out the possibility of
malignancy prior to choosing conservative treatment, which was
advocated since all 3 cases have issues with infertility. For the
management of endometrial polyps, hysteroscopic resection is
the preferred method [4]. However, in some instances like in giant
polyps, immediate hysteroscopic removal may not be feasible. This
could be due that giant polyps occupy the entire uterine cavity that
distending the cavity during hysteroscopy for visualization of the
polyp’s attachment may not be done. Aside from failed removal of
the polyp, morbidities like fluid overload and uterine perforation
can be encountered. Although there is limited evidence with the
use of GnRH agonist in endometrial polyps, it’s use was suggested
as it may significantly decrease the size of the polyps to make the
hysteroscopic resection achievable.
GnRH agonists has revolutionized the management of many
conditions in gynecology based on the discovery that when
administered in a non-pulsatile fashion, they down regulate
pituitary GnRH receptors, and therefore decrease the production
of FSH and LH. It has been widely used for submucus myomas to
decrease its size and make its hysteroscopic removal manageable
with less morbidity. It used as a neo-adjuvant therapy prior to
hysteroscopy to decrease bulk of the myoma and induce a state of
hypoestrogenism. Pretreatment with GnRH agonists improves the
hemoglobin level, reduces blood loss during surgery, and reduces
uterine and leiomyoma volumes in as much as 40-50%, with most
of the reduction occurs in the first 12 weeks [5]. This is especially
helpful in infertile patients because this prevents destruction of the
surrounding endometrial tissue [6]. Given the same concept for
myomas, GnRH can then be used as pre-treatment for giant polyps
since they have characteristic cytogenetic rearrangements similar to
uterine leiomyoma [2]. As said previously, polyps contain estrogen
as well as progesterone receptors, and the concentrations of these
receptors are significantly higher in the glandular epithelium of
endometrial polyps than those in the normal endometrium [7].
Hormonal inhibition of the endometrium can induce mucosal
thinning and decreased bleeding. The effect of GnRH agonist can
extend up to 1 month from the last dose and this could be due
to persistent hypoestrogenism and consequent inhibition of
regeneration of viable endometrial cells [5]. In the cases presented,
GnRH agonist has significantly decreased the size of giant polyps
even after 1 dose. All of the patients have reported vaginal bleeding
along with passage of meat-like materials, which were believed
to be fragments of the polyp spontaneously sloughing off from
its attachment due to devascularizing effect of the GnRH agonist.
None of the cases developed anemia or needed blood transfusion
despite the said vaginal bleeding. The 1st case even successfully
underwent hysteroscopic polypectomy after 6 doses of GnRH with
no morbidity encountered and no residuals after, given the initial
size of her polyp. With this in mind, there is room for GnRH agonists
in treating endometrial polyps, specifically the giant polyps, where
immediate hysteroscopic removal may tend to be difficult or may
lead to failure, more so, morbidity. The cases have shown the
effect of GnRh agonists in significantly decreasing the size of the
polyps probably by inducing a hypoestrogenic state and at the
same time deceasing the vascularization of the polyps causing
it to spontaneusly slough off from its base. This will facilitate
complete hysteroscopic removal of the giant polyp at the same
time decreasing chances of morbidity. Although further studies are
needed to strengthen its use in endometrial polyps, this may open
an area for more research work.
Conclusion
Endometrial polyps, specifically the giant polyps, can be an incapacitating cause of abnormal uterine bleeding, which are often associated with infertility. In such cases, conservative management in the form of hysteroscopic removal is encouraged. However, given the size of a giant polyp, there will be technical difficulty in doing its resection. Use of GnRH agonist as neoadjuvant treatment for giant polyps can be advised. Using the same concept of GnRH agonist in shrinking myomas, it can induce a hypoestrogenic state causing devascularization of the endometrial lining. This will help significantly decrease the size of polyp, allowing complete hysteroscopic removal. However, further research studies are still suggested to strengthen its neoadjuvant use with giant endometrial polyps.
References
- Nigel Pereira, Allison C Petrini, Jovana P Lekovich, Rony T Elias, Steven D Spandorfer (2015) Surgical Management of Endometrial Polyps in Infertile Women: A Comprehensive Review. Surgery Research and Practice 2015: 914390.
- Stuti Tyagi, Rahul Manchanda, Sudhir Kulkarni, Fardina Samadi (2017) Manchanda's Endoscopic Centre, PSRI Hospital, New Delhi. Giant Endometrial Polyps- A Case Series. International Journal Of Current Advanced Research 6(6): 4185-4189.
- Thomas Römer (1998) Benefit of GnRH Analogue Pretreatment for Hysteroscopic Surgery in Patients with Bleeding Disorders. Gynecol Obstet Invest 45(1): 12-21.
- Ugo Indraccolo , Maria Matteo, Romolo Di Iorio (2011) The Pathogenesis Of Endometrial Polyps: A Systematic Semi-Quantitative Review. International Journal of Clinical Medicine 2: 478-480.
- P Vercellini, L Trespidi, T Bramante, S Panazza, F Mauro (1994) Gonadotropin Releasing Hormone Agonist Treatment Before Hysteroscopic Endometrial Resection. International Federation of Gynecology and Obstetrics 45(3): 235-239.
- Vikram Sinai Talaulikar, Anna Maria Belli, Isaac Manyonda (2012) GnRH Agonists: Do They Have a Place in the Modern Management of Fibroid Disease? J Obstet Gynaecol India 62(5): 506-510.
- Yu Hung Lin, Yuh Yu Chou, Lee Wen Huang, Kok Min Seow, Jiann Loung Hwang (2013) An Adenomyomatous Polyp Presenting As A Large Hypervascular Tumor And Its Response To A Gonadotropin-Releasing Hormone Agonist. Taiwanese Journal of Obstetrics & Gynecology 52(1): 129-e130.

 Case Report
Case Report