Abstract
The Peutz-Jeghers Syndrome (PJS) is a rare autosomal dominant disease characterized by macules of mucocutaneous pigmentation and hamartomatous intestinal polyps. Some signs of the PJS appear in childhood, usually with abdominal pain. In some cases, patients can develop complications. In this article, we report a case of a patient with PJS that reached the emergency room after presenting a concomitant gastric outlet obstruction (GOO). The patient underwent through an endoscopic polypectomy, followed by a laparotomy and an intraoperative enteroscopy. The symptoms were controlled and the extraction of hamartomatous intestinal polyps were achieved, culminating with an intestinal segment resection with muscle atrophy and posterior gastrojejunostomy. There is evidence of PJS cases related to other conditions that developed abnormal scenarios such as biliary obstruction or cecal appendix polyps. However, the association between PJS and GOO and a concomitant delimited intestinal aperistalsis has not been reported. Thus, this case report shows the possible association between the PJS and GOO, whose cause is the intraluminal occupation of the duodenum by polyps and the synergy of the symptoms given by the atrophy of the jejunum muscle.
Keywords: Peutz-Jeghers Syndrome; Peutz- Jeghers Aggravations; Gastric Outlet Obstruction
Abbreviations: PJS: Peutz-Jeghers Syndrome; GOO: Gastric Outlet Obstruction; CT: Computed Tomography; VAS: Visual Analog Scale
Background
The proliferation of polyps or polyposis is mostly associated
with the elderly. However, a small proportion of cases is related to
hereditary disorders, including the Peutz Jeghers Syndrome (PJS), a
rare disease with an estimated incidence of 1 in 25,000 to 300,000
live births [1]. PJS is based on three clinical pillars:
a. The appearance of melanic mucocutaneous pigmentation, in
the form of small macules of 1 to 5 mm around the mouth, eyes,
anus, fingers, and toes [2].
b. The appearance of 1 to 20 hamartomatous polyps per intestinal
segment generally found in the small intestine, most frequently
in the jejunum and followed by the ileum and duodenum [3].
These polyps are formed by glandular epithelium supported
by an arboriform proliferation of smooth muscle. The smooth
muscle bands fan out into the polyp head and thin as they
advance to the surface [3].
c. The autosomal dominant hereditary character. Nevertheless,
it should be noted that cases of PJS without a hereditary association have also been reported, the so-called “sporadic
PJS”.
d. The polyps found in PJS are commonly present in early
adulthood. One-third of affected people experience symptoms
during the first ten years of life, with intermittent abdominal
pain being the most common of them [4]. This pathology is
believed to originate from the germline mutation of the serine/
threonine kinase 11 (SKT11) gene. It has been reported that
patients who suffer from this mutation have a risk between 9
to 15 times greater than the general population of suffering
intestinal cancer [5,6], and to a lesser extent, extraintestinal
cancer, specifically the lung, breast, uterus, testicle, and ovary
cancer [7]. Moreover, several studies have confirmed a high
association between the genetic alteration in STK11 and the
oncological pathology.
The management of PJS begins with active endoscopic
surveillance such as upper gastrointestinal endoscopy, video
capsule endoscopy, and colonoscopy, searching for polyps. Other
study alternatives are magnetic resonance enterography or
computed tomography and barium follow-up that could be more
precise. Nevertheless, the latter is limited by radiation exposure
and should be avoided in children [8-10]. The main complications
of this syndrome are anemia, intussusception, and intestinal
obstruction; however, despite the intestinal obstruction being
a prevalent complication, the presentation of a PJS with gastric
retention syndrome is infrequent. From this premise, the objective
of this study was to present the case of a patient with a diagnosis
of PJS, who presented a duodenal polyp that obstructed the lumen.
This obstruction was manifested by a gastric outlet obstruction
(GOO) and simultaneously with the investigation of a hypotonic
and a peristaltic segment of the proximal jejunum. In this study, we
report the possible association between the PJS and GOO, which so
far, there are no reports of an SPJ case with a similar presentation.
Case Report
A 25-year-old female patient with a morbid history of Peutz- Jeghers Syndrome, without previous complications and without follow-up, goes to the emergency department due to symptoms of one month of evolution and intensified during the last two days. The patient consults for pain in the epigastrium, periumbilical irradiation of progressive intensity reaching a visual analog scale (VAS) of 10/10, colic type and associated with explosive vomiting and a loss of 7 kg of weight in the last month. A physical examination highlighted: allergic facial, dehydrated mucous membranes and decreased turgor. The patient exhibited faint macules on the oral mucosa, for which she underwent dermatological laser treatment (Figures 1A & 1B). In addition, she presented a soft, depressible, and painless abdomen, without the presence of masses or visceromegaly. A computed tomography (CT) scan of the chest, abdomen, and pelvis was performed, which revealed images suggestive of multiple polyps at the level of the duodenum-jejunal transition and proximal jejunum.
Figure 1:
A. Patient with multiple peri-oral pigmented macules at the time of diagnosis.
B. After laser treatment, the patient shows the disappearance of the macules almost entirely at the time of the physical
examination in the Emergency Department.
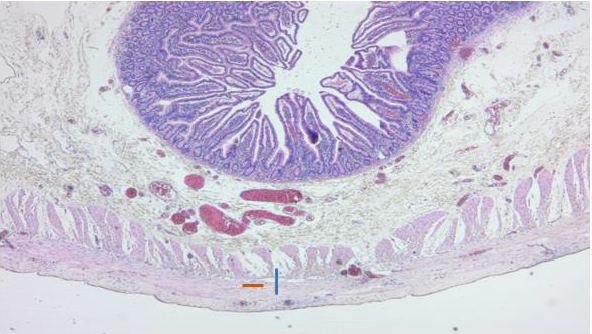
Also, retention distended stomach was revealed. Considering the symptomatology and the pathological findings in the tomography, it was decided to perform an endoscopic polypectomy in the pavilion. In this procedure, a pedunculated polyp obstructing the intestinal lumen at the level of the third to fourth duodenal portion was found and resected. A rapid biopsy obtained was negative for dysplasia and malignancy (Figure 2). Subsequently, a colonoscopy was performed, which allowed identifying a 10 mm diameter pedunculated lesion located in the distal sigmoid colon. This lesion exhibited a polypoid appearance with an erythematous head, and fibrin remains on its surface. The patient evolved with persistent abdominal pain, intermittent vomiting of lesser quantity, and periodicity. Control computed tomography with oral contrast reported a slowdown in the passage of contrast medium at the level of the proximal jejunum with the presence of polyps that did not completely obstruct the lumen. Based on the results obtained in the follow-up studies, it was decided the re-intervention of the patient employing an exploratory laparotomy and intraoperative enteroscopy.
Figure 2: Peutz-Jegher pedunculated hamartomatous polyp, located in the duodenum, completely obstructing the intestinal
lumen. This polyp was resected by endoscopic polypectomy.
Results
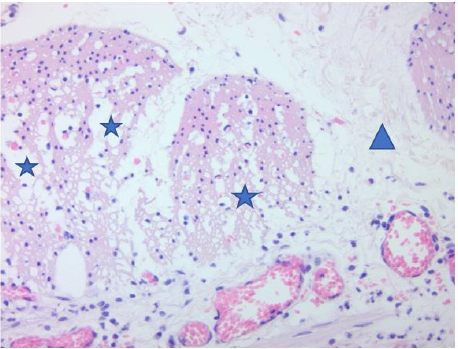
During the procedure, a polyp was found at the fourth portion of the duodenum level, and multiple polyps in the distal ileum from 5 to 40 cm from the ileocecal valve that was extracted with a biopsy forceps. Moreover, the last polyp located 120 cm from the ileocecal valve was resected endoscopically. None of the polyps found obstructed the entire intestinal lumen. Also, a proximal jejunum area of approximately 15cm with aperistalsis was detected. A neostigmine test was performed with local infiltration, confirming abolished peristalsis in the proximal jejunum area. The rest of the small intestine maintained good contractibility. The jejunal segment (15 cm) was resected with its mesentery (it was sent for a deferred histopathological study) (Figure 3), culminating the intervention with a gastro-jejunal-lateral anastomosis performed without complications. In the histopathological study, a muscle wall thinned was observed, especially at the expense of the internal circular. Even, a loss of muscle fiber density was observed, with connective tissue spaces between them (Figure 4). Also, a degenerative changes of the muscle tissue of the internal circular was visualized, along with loss of muscle fibers (Figure 5). After surgery, the patient showed a favorable evolution and remained hemodynamically stable and afebrile. She presented a progressive decrease in pain, gas elimination, and preserved stools, and she was discharged on the 8th postoperative day. At postoperative control up to 6 months, the patient remained asymptomatic.
Figure 3: Peutz-Jeghers type hamartomatous polyp resected from the ascending colon and histologically described with a
complex polypoid arrangement. This polyp is composed of bands of smooth muscle tissue surrounded by glands without
epithelial atypia but with focal cystic hyperplasia and dilatation.
Figure 4: Muscle wall thinned, especially at the expense of the internal circular (blue line). Loss of muscle fiber density is
observed, with connective tissue spaces between them (orange line).
Figure 5: Degenerative changes of the muscle tissue of the internal circular (blue stars), loss of muscle fibers (blue triangle).
Discussion
Peutz-Jeghers syndrome is an autosomal dominant disease
characterized by the finding of multiple hamartomatous polyps
in the gastrointestinal tract, mucocutaneous pigmentation, and an
increased risk of both gastrointestinal and non-gastrointestinal
cancer [11]. Concerning mucocutaneous pigmentation, it is present
in more than 95% of individuals with PJS and is caused by pigmentladen
macrophages in the dermis. This pigmentation is usually
flat, bluish-gray to brown spots 1 to 5 mm in size, and generally
manifests during the first or second year of life. The size and
number of pigmentations increase continuously in the following
years and finally clear up after puberty, except for those located in
the buccal mucosa [7]. Unfortunately, not all patients may exhibit
mucocutaneous pigmentation due to the time of the disease or because the patient underwent dermatological laser treatment
on the macules. In this treatment, the laser vibration can alter the
pigmentary system, and the beams may absorb the dark color of the
melanocytes in the pigmented areas, masking this symptom.
On the other hand, polyps appear mainly in the small intestine
(in order of prevalence: jejunum, ileum, and duodenum), but they
can also be located in the colon or stomach. Histologically, they
are defined by a normal epithelium surrounding smooth muscle
bundles arranged in a branched or leafy pattern [8]. As far as we
know, no other cases were found related to aperistalsis of the small
intestine. It seems a feasible theory in the relationship with the
atrophy of the smooth muscle presented in the case, the same of the
formation of polyps: the thinning of the smooth muscle when they
advance to the surface. The mentioned clinical characteristics were
manifested in a typical way in our patient. The patient presented
numerous peri-oral pigmented macules at the beginning of the
disease. Also, multiple polyps appeared predominantly in the small
intestine, a common and known feature in this syndrome. The
diagnosis of PJS is made clinically in patients with hamartomatous
polyps, demonstrated by histology if two of the following three
conditions are present: positive family history with an autosomal
dominant inheritance pattern, mucocutaneous hyperpigmentation,
and/or polyposis of the small intestine [8].
Although our patient was previously diagnosed with PJS, we
confirmed 2 of the 3 criteria mentioned through physical examination
and the imaging study findings, confirming the diagnosis of Peutz-
Jeghers syndrome. Concerning the morphology, if polyps larger than
0.5 mm are detected, the recommended management is endoscopic
polypectomy or double-balloon endoscopy to reduce the risk of
complications [9,10,12,13]. The aforementioned is performed
considering the inherent morbidity of a surgical procedure and the
possibility of a residual short bowel syndrome due to resection of
intestinal segments. However, if a large load of polyps is detected,
the control by endoscopic approach is not achieved, or there is a
complication, the most accepted procedure is a laparotomy with
intraoperative enteroscopy since it offers direct vision to identify
and resect the polyps [14]. In our case report, both approaches
were performed. First, an endoscopic polypectomy was performed
to treat the obstruction of the lumen, with the consequent GOO
caused by a polyp located in the duodenum. Finally, a laparotomy
was carried out with intraoperative enteroscopy due to the finding
of multiple new polyps in monitoring exams and the slowing down
of the intestinal transit associated with the patient’s symptoms.
Patients with PJS may present complications such as
intussusception, anemia, obstruction, perforation, and cancer,
the latter being the most significant and studied given its
relationship with PJS. However, given that biopsies did not show
the presence of cancerous cells, this issue was not addressed.
In the literature, there is a lack of official epidemiological data
on PJS complications. Nonetheless, according to the published
case reports, intussusception is the most frequent complication
(excluding cancer), which can cause intestinal obstruction when it
is generated by large polyps (> 15 mm), being the small intestine
the most affected site, specifically the jejunum [15]. On the other
hand, intestinal obstruction, together with anemia, is the second
most reported complication and is produced by the appearance
of a large polyp that covers the entire intestinal lumen. Also, these
complications may result from an associated intussusception (in
the case of obstruction) and injury/bleeding of the polyp or cancer
(in the case of anemia). There is evidence of PJS cases associated
with other diseases and, therefore, presented in an atypical way
such as i) an extra ampullary PJ polyp, which causes duodenal
intussusception and presents with biliary obstruction and ii) a
PJ polyp located in the appendix, presented with concomitant
appendicitis or with melena as the only symptom.
Nevertheless, no cases of PJS have been reported associated
with a concomitant GOO or intestinal aperistalsis. In this case
report, the patient’s clinical picture coincided with the GOO, where
the polyps in the duodenum may act as a mechanical factor causing
food retention and its related symptoms. In addition, it is important
to highlight that the jejunal smooth muscle atrophy that the patient
presented could play a role in a possible synergistic factor in the
GOO. However, more studies are necessary to establish concrete
and detailed causal relationships between both syndromes.
Conclusion
Peutz-Jeghers syndrome is a rare disease that has not been deeply studied. As far as we know, there are few reported cases of PJS concomitant with other syndromes, specifically gastric outlet obstruction. There is an undiscovered and/or studied relationship between these pathologies, especially considering the high probability that there are more cases globally, with these characteristics, without reporting. We speculate that the association of gastric outlet obstruction could be based on a mechanical effect generated by the polyps of the small intestine, which could alter the function of the stomach. This alteration could contribute to the aperistalsis of the jejunum, causing the symptomatology. Despite the above, more evidence is needed to demonstrate this association, mainly if muscular atrophy is part of the PJS.
Conflict of Interest
The authors declare that they have no conflict of interest.
References
- Wu M, Krishnamurthy K (2020) Peutz-Jeghers Syndrome.
- Idrogo Regalado B, Frisancho Velarde O (2016) Síndrome de Peutz- Jeghers. Presentación de cinco casos. Rev Gastroenterol Peru 36(2): 165-168
- McGarrity T, Amos C (2006) Peutz-Jeghers syndrome: clinicopathology and molecular alterations. Cellular and Molecular Life Sciences 63(18): 2135-2144.
- Choudhury S, Das A, Misra P, Ray U, Sarangi S (2018) Peutz-Jeghers Syndrome: A Circumventable Emergency. Indian Journal of Dermatology 63(2): 168-171.
- Calva D, Howe J (2008) Hamartomatous Polyposis Syndromes. Surgical Clinics of North America. 88(4): 779-817.
- Tsao H (2000) Update on familial cancer syndromes and the skin. Journal of the American Academy of Dermatology 42(6): 939-969.
- Peutz-Jeghers syndrome: Clinical manifestations, diagnosis, and management.
- Kliegman R Nelson (2020) Tratado de Pediatrí pag 2061-2064, cap 372. Barcelona: Elsevier.
- Gupta A, Postgate A, Burling D, Ilangovan R, Marshall M, et al. (2010) A Prospective Study of MR Enterography Versus Capsule Endoscopy for the Surveillance of Adult Patients With Peutz-Jeghers Syndrome. American Journal of Roentgenology 195(1): 108-116.
- Tomas C (2014) Update on imaging of Peutz-Jeghers syndrome. World Journal of Gastroenterology 20(31): 10864.
- Gastroparesis: Etiology, clinical manifestations, and diagnosis.
- Beggs A, Latchford A, Vasen H, Moslein G, Alonso A, et al. (2010) Peutz-Jeghers syndrome: a systematic review and recommendations for management. Gut 59(7): 975-986.
- Syngal S, Brand R, Church J, Giardiello F, Hampel H, et al. (2015) ACG Clinical Guideline: Genetic Testing and Management of Hereditary Gastrointestinal Cancer Syndromes. American Journal of Gastroenterology. 110(2): 223-262
- Hinds R, Philp C, Hyer W, Fell J (2004) Complications of Childhood Peutz-Jeghers Syndrome: Implications for Pediatric Screening. Journal of Pediatric Gastroenterology and Nutrition 39(2): 219-220.
- Tavusbay C, Acar T, Kar H, Atahan K, Kamer E (2018) The patients with Peutz-Jeghers syndrome have a high risk of developing cancer. Turkish Journal of Surgery 34(2): 162-164.

 Case Report
Case Report