Abstract
Background: Dermatological manifestations in diabetes mellitus include those due to disease itself, as well as complications and their respective treatments. Pruritus often presents with cutaneous manifestations, causing psychological distress and leading to scratching. Data showing an association between pruritus and health-related quality of life in Thai type-2 DM (T2DM) patients are still lacking. Our study concerns itself with effects of type-2 DM in an urban area, and ways to improve the physical and psychological quality of life of patients.
Objectives: The purpose of the present study was to evaluate the dermatologic quality of life among Thai T2DM patients with pruritus, and the association between plasma glucose level and degree of itching.
Materials and Methods: The study included Thai T2DM patients with pruritus, aged 18 years or above, and who attended the outpatient DM Clinic at Vajira Hospital. Their previous plasma glucose, HbA1C level and personal histories were recorded. They were also asked to complete the questionnaire regarding Dermatologic Life Quality Index and Itching Numeric Sating Scale.
Results: 300 T2DM patients with pruritus were enrolled in this study. The average plasma glucose level was 160 mg/ dL, and HbA1C level was 7.9%. We found no specific area of pruritus and most of the people have pruritus in more than one area. Most of our subjects have a mild to moderate degree of pruritus. Our study found that serum HbA1C levels above 6.5%, and previous topical steroid and topical moisturizer no usage were significantly associated with pruritus. We found that dry skin and sweating were statistically aggravating factors after multivariate analysis. There is a strong association between education, marital status and DLQI score.
Conclusion: Our study found that the control of HbA1C level, and no usage of topical steroids and moisturizers were statistically associated with clinical pruritus. Although our study showed that pruritus had small effects on quality of life, we also found that moisturizer usage significantly helps to improve clinical pruritus. Thus, giving moisturizer to all T2DM patients may help to improve and prevent their pruritus symptoms.
Keywords: DM; DLQI; Pruritus
Abbreviations: T2DM: Type 2 Diabetes Mellitus; DLQI: Dermatology Life Quality Index; NRS: Numeric Rating Scale
Short Communication
Type 2 diabetes mellitus (T2DM) is a major health problem in Thailand. Nowadays, up to 800 patients per month register in Thai DM clinics to follow up their illness. T2DM systematically affects the body in both long-term and short-term outcomes [1,2]. Longterm effects of T2DM cause serious common consequences such as diabetic retinopathy, peripheral neuropathy, diabetic nephropathy,and diabetic dermopathy, while short-term effects cause troublesome symptoms such as fatigue, abnormal weight change, and insomnia. These symptoms are known to adversely affect patients’ quality of life and mental health [1-3]. Dermatological manifestations in diabetes mellitus are due to disease itself, complications and their treatments. Dermatologic lesions associated with diabetes mellitus are classified into disease specific and non-specific symptoms. Consequences of neurovascular complications such as macroangiopathy, microangiopathy, and diabetic neuropathy are also formed [4-6].
Diabetic treatments can cause various dermatologic lesions.
Treatment with insulin can cause allergic reactions, lipoatrophy,
and insulin edema [5,6]. It has also been found that some
conditions are associated with diabetics than nondiabetics such as
lichen planus, eruptive xanthomas, perforating dermatosis, vitiligo,
and yellow nails [5,6]. Pruritus, or itching, involves cutaneous
manifestations over extended periods and often causes patients
psychological distress, and causes which leads to skin infection
[7,8]. Common causes of pruritus in dermatological conditions are
atopic dermatitis, urticaria, psoriasis, and insect bite. However,
systemic medical conditions include chronic renal failure, jaundice,
chronic hepatitis, diabetes mellitus, and thyrotoxicosis [9-12].
To our knowledge, there are some studies about the association
between plasma glucose level and pruritus. They found that higher
plasma glucose levels are significantly associated with a greater
prevalence of pruritus in T2DM patients [9].
T2DM is associated with quality of life in many areas such as
family, daily life, and self-esteem [13]. Histamine level is associated
with pruritus; hence, antihistamines are considered to play a role
in the reduction of itching. However, there is no standard treatment
guideline for regularly using antihistamine in T2DM patients [14-
16]. Nevertheless, the data for an association between pruritus
and health-related quality of life in Thai T2 DM patients are still
lacking. Therefore, the purpose of our study was to evaluate the
dermatology quality of life among Thai T2DM patients with pruritus
and the association between plasma glucose level and degree of
itching using Dermatology Life Quality Index (DLQI) questionnaires
and the Itching Numeric Rating Scale (NRS) [17,18]. The factors
considered included age, gender, educational degree, and duration
of type 2 DM [1].
Materials and Methods
This study was approved by Vajira Hospital Institutional Review Board. The study design was a prospective descriptive study. Thai T2DM patients with pruritus, aged 18 years over, and who attended the out-patient DM Clinic at Vajira were included in the study. All of the other causes of pruritus (atopic dermatitis, urticaria, psoriasis, cutaneous fungal infection, contact dermatitis) and the other systemic conditions associated with pruritus such as chronic renal failure, jaundice, chronic hepatitis, thyrotoxicosis, and hematologic malignancy were excluded from the study.
Statistical Analysis
All analyses were performed by using SPSS software version 22.0. Continuous data were described as mean and standard deviation. The statistical comparisons of the DLQI results between subpopulations were performed by using Fisher’s exact test and Mann-Whitney U Test. A p-value < 0.05 was considered statistically significant. Correlation analysis was made by using Spearman’s Correlation Test [19-21].
Results
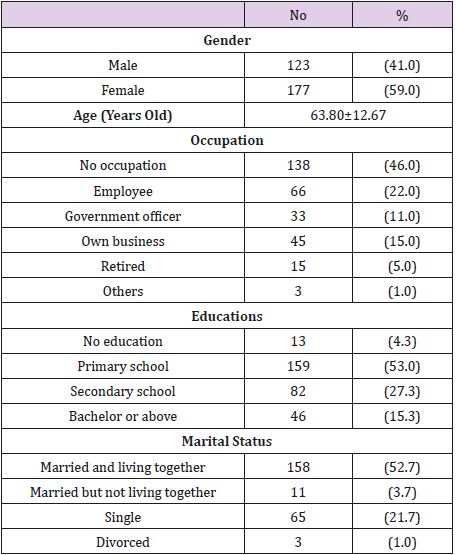
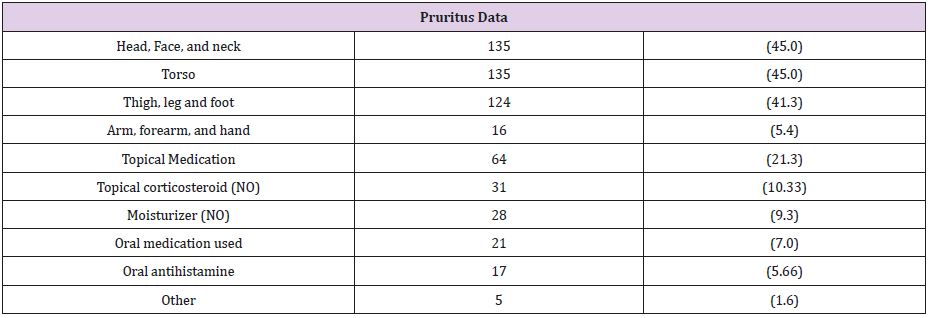
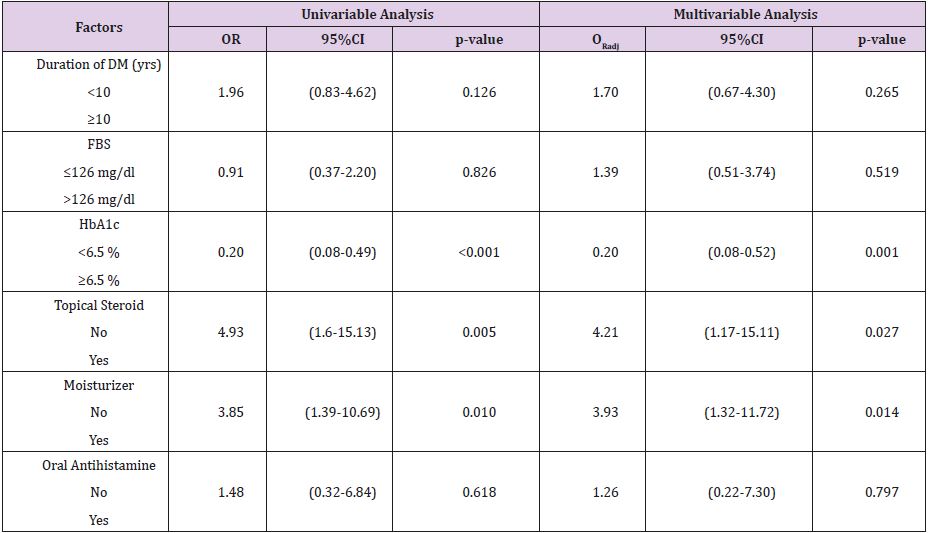
Of the 300 patients enrolled, 177 patients were female, and the rest were male. Table 1 shows demographic data in patients studied. Almost half of them were unemployed. More than fifty percent of them were married and living with their spouse. One hundred and fifty-nine patients graduated from primary school. The average duration for having DM was nine years, and the average plasma glucose level was 160 mg/dL while average HbA1C level is 7.9%. Table 2 shows the characteristics of pruritus in our patients studied. We found no specific area of pruritus and most of the people have pruritus in more than one area. Approximately forty percent of the patients mentioned that head, neck, body, and lower extremities are the most itch areas, while upper extremities are less affected. After univariate and multivariate analysis, our study found that serum HbA1C level above 6.5%, no usage of topical steroids and topical moisturizer were significantly associated with pruritus, while anti-histamine usage, serum fasting plasma glucose >126 mg/dL, and having diabetes for over 10 years were not relevant factors in pruritus (Data shown in Table 3).
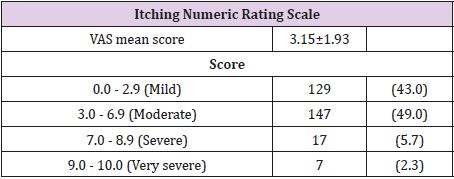
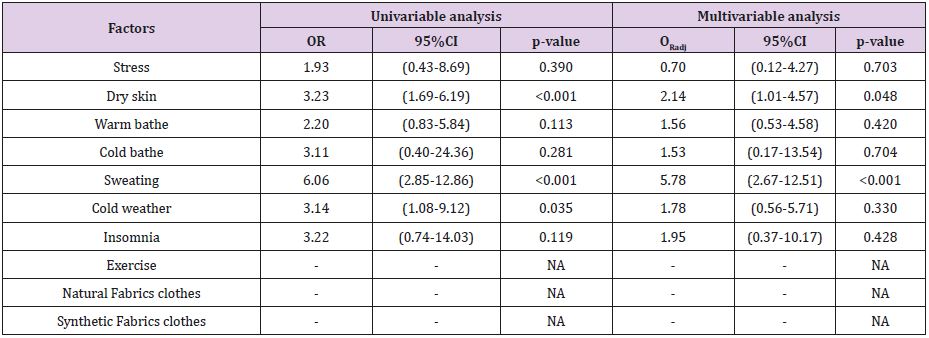
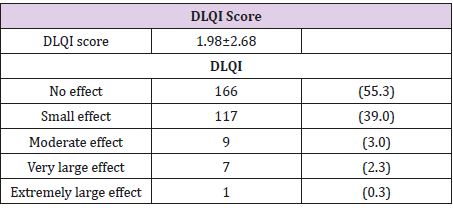
Table 4 shows the numeric rating scale in each range and average score. Our study shows VAS mean score were3.15±1.93. of our subjects had a mild to moderate degree of pruritus. Table 5 shows associated factors that affect pruritus. We found that dry skin, sweating, and cold weather were statistically aggravating factors (when using univariate analysis; p-value < 0.05). However, cold weather is not statistically significant after multivariable analysis. Table 6 shows DLQI score in our patients studied. Our study found that the mean DLQI score is 1.98. More than half of our subject responded that their quality of life was not affected by pruritus [22].
Discussion
Type-2 diabetes mellitus (T2DM) is a systematic disease, in
which multiple organs are involved including the dermatological
system. The effects of T2DM to dermatological problems come from
the disease, complications, and the consequences of treatment [1-
3]. Pruritus (itching) is one of the most common clinical symptoms.
It often presents in T2DM patients with adverse effects on their
quality of life and mental status [7]. Of all the systemic diseases
associated with pruritus, renal failure is probably the most common
underlying disease. In diabetes mellitus, generalized pruritus is rare
but localized pruritus is more frequent, especially in the perianal/
genital region, and caused by fungal infection [23]. To date, there
have been many studies about the association between plasma
glucose level and pruritus [9,13]. They found that an elevated
plasma glucose level is significantly associated with a greater
prevalence of pruritus in T2DM patients [9,13]. Nevertheless, data
for the association between pruritus and health-related quality of
life in Asian T2DM patients are still lacking.
Our study showed that eighty percent of T2DM patients had
mild to moderate pruritus (NRS 0.0 - 6.9). We found that most of
them had clinical pruritus more to than one part of the body. The
most affected areas were the face, torso, and lower extremities,
while upper extremities were less affected. The diabetic profiles
in our subjects were not well controlled. The average duration
of having DM was nine years, average plasma glucose level was
160. Moreover, our study found that dry skin and sweating were
statistically significant aggravating factors (p-value<0.05). After
multivariable analysis, it seems that serum HbA1C level, topical
steroid no usage, and topical moisturizer no usage were associated
with pruritus in our study (p-value<0.05). In poorly controlled
T2DM. Dry skin is a well-known factor which aggravates itching,
so topical moisturizer is commonly effective, thus explaining its
association with pruritus. There were strong associations between
education, marital status and DLQI score (p-value < 0.05).
T2DM patients who have pruritus were affecting their quality
of life. We found that mean DLQI score was 1.98, which means that
pruritus has no, or a small, effect on their quality of life. Compared
to other systemic diseases, our study had lower DLQI scores than
others. Batalla et al. showed the DLQI in CLE had an extremely
large effect on quality of life in more than half of the patients [24].
A study of DLQI in Thai patients with systemic sclerosis showed
moderate impact on patients’ dermatology-specific health-related
quality of life, which is predominantly in pain and pruritus (mean
DLQI score = 6.3) [21]. Boonsiri et al. reported DLQI in Thai dialysis
patients showing the large impact on their quality of life, in which
xerosis and pruritus were the most significant problems (mean
DLQI score = 4.74) [12]. However, our study was done only in a
government hospital. More than 40% of all patients had no job,
and their education was below bachelor’s degree level. The degree
and frequency of dermatological involvement in T2DM disease,
compared to other diseases such as ESRD, systemic sclerosis, and
CLE seem to be less frequent. It means that dermatologic quality
of life of individuals might vary due to socioeconomic, educational
status, and specific systemic disease.
Conclusion
Our study found that the control of HbA1C level, usage of topical steroids and moisturizers are statistically associated with clinical pruritus. Dry skin and sweating were statistically aggravating factors. Although our study found that pruritus had small effects on quality of life, we also found that use of topical steroids and moisturizers is significantly helps improve clinical pruritus. Thus, giving moisturizer to T2DM patients may help to improve and prevent their pruritus symptoms.
References
- Trikkalinou A, Papazafiropoulou AK, Melidonis A (2017) Type 2 diabetes and quality of life. World J Diabetes 8(4): 120-129.
- Papadopoulos AA, Kontodimopoulos N, Frydas A, Ikonomakis E, Niakas D (2007) Predictors of health-related quality of life in type II diabetic patients in Greece. BMC Public Health 7: 186.
- Polonsky WH (2000) Understanding and Assessing Diabetes-Specific Quality of Life. Diabetes Spectrum 13(1): 36.
- Chan JC, Malik V, Jia W, Kadowaki T, Yajnik CS, et al. (2009) Diabetes in Asia: epidemiology, risk factors, and pathophysiology. JAMA 301(20): 2129-2140.
- Chilukuri S, Nikica C, Ivana PR (2002) Dermatologic lesions in diabetes mellitus. Dibetologia Croatica p. 31-33.
- Tarikci N, Kocatürk E, Güngör Ş, Topal IO, Can PÜ, et al. (2015) Pruritus in Systemic Diseases: A Review of Etiological Factors and New Treatment Modalities. The Scientific World Journal 2015: 803752.
- Yosipovitch G, David M (1999) The diagnostic and therapeutic approach to idiopathic generalized pruritus. Int J Dermatol 38(12): 881-887.
- Zirwas MJ, Seraly MP (2001) Pruritus of unknown origin: A retrospective study. J Am Acad Dermatol 45(6): 892-896.
- Etter L, Myers SA (2002) Pruritus in systemic disease: mechanisms and management Dermatol Clin 20(3): 459-472.
- Ponticelli C, Bencini PL (1995) Pruritus in dialysis patients: a neglected problem. Nephrol Dial Transplant 10(12): 2174-2176.
- Jones EA, Bergasa NV (1992) The pruritus of cholestasis and the opioid system. JAMA 268(23): 3359-3362.
- Boonsiri M, Prompongsa S, Bunyaatavej S (2015) Dermatologic Life Quality Index in Thai Dialysis Patients with Cutaneous Manifestations: A Cross-Sectional Study and Review. Vajira Medical Journal 59(1): 11-20.
- Puavilai A, Stuifbergen AK (2000) Quality of life for Thai women with diabetes. Health Care Women Int 21(6): 471-483.
- Bhate V, Abhayankar S (2014) Health related quality of life in type 2 diabetic patients with special emphasis on gender and mode of treatment. Indian Journal of Health and Wellbeing 5(3): 350-353.
- Rajagopalan M, Saraswat A, Godse K, Krupa Shankar DS, Sanjiv K, et al. (2017) Diagnosis and Management of Chronic Pruritus: An Expert Consensus Review. Indian J Dermatol 62(1): 7-17.
- Longley J, Duffy TP, Kohn S (1994) The mast cell and mast cell disease. J Am Acad Dermatol 32(4): 545-561.
- Finley AY, Khan G K (1994) Dermatology Life Quality Index (DLQI)--A simple practical measure for routine clinical use. Clin Exp Dermatol 19(3): 210-216.
- Finlay AY (2004) Quality of life indices. Indian J Dermatol Venereol Leprol 70(3): 143-148.
- Kulthana K, Jiumton S, Wanitphakdeedecha R (2004) The Validity and Reliability of the Dermatology Life Quality Index (DLQI) in Thais. Thai J Dermatol 20: 113-123.
- Ko MJ, Chiu HC, Jee SH, Hu FC, Tseng CH (2013) Postprandial blood glucose is associated with generalized pruritus in patients with type 2 diabetes. Eur J Dermatol 23(5): 688-693.
- Chularojanamontri L, Sethabutra P, Kulthanan K, Manapajon A (2011) Dermatology life quality index in Thai patients with systemic sclerosis: A cross-sectional study. Indian J Dermatol Venereol Leprol 77(6): 683-637.
- Lemeshow S, Hosmer DW, Klar J, Lwanga SK, Organization WH (1990) Adequacy of sample size in health studies. WHO?
- Ständer S, Augustin M, Reich A, Blome C, Ebata T, et al. (2013) Pruritus assessment in clinical trials: consensus recommendations from the International Forum for the Study of Itch (IFSI) Special Interest Group Scoring Itch in Clinical Trials. Acta Derm Venereol 93(5): 509-514.
- Batalla A, García Doval I, Peón G, de la Torre C (2013) A Quality-of-Life Study of Cutaneous Lupus Erythematosus. Actas Dermosifiliogr 104(9): 800-806.

 Short Communication
Short Communication