Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
Sorin Gheorghe Mihali1*, Paul Cornel Freiman2 and Emanuel Adrian Bratu3
Received: July 27, 2018; Published: August 09, 2018
*Corresponding author: Sorin Mihali, 16 Memorandului Street, 300208, Timișoara, Romania
DOI: 10.26717/BJSTR.2018.07.001554
The aim of this study was to compare the conventional healing screw with custom healing screw in terms of maintenance of soft tissue architecture. Twenty-four patients who underwent single tooth extraction and single immediate implant placement were included in the study. Twelve patients were treated with conventional healing screw after immediate implant placement (control group) and 12 were treated with screwretained custom healing screw (test group). After minimally traumatic tooth extraction, a temporary abutment was fabricated utilizing flowable composite, which adapted to the socket architecture, to serve as a customized healing screw. In order to evaluate soft tissue remodeling in all cases, digital impressions were made before tooth extraction, at implant insertion, at 6 months after insertion, and after placement of the final restorations. After 6 months of the Osseo integrated period, the custom healing screw served successfully as a tooth profile for peri-implant tissue. In cases of implants with conventional healing screw, soft tissue remodeling around the implants is observed, in contrast to cases of custom healing abutments. Correct design of a healing abutment is important for maintaining the emergence contour in cases of immediate implant placement. In our study, a considerable difference was observed between the standard healing screw and customized healing screw. The selection between provisional restoration and customized healing abutment is only based on esthetic considerations.
Keywords: Custom healing screw; Soft tissue; Tooth extractions; Emergence profile; Immediate implant
Hard and soft tissue modifications occur after tooth extraction and immediate implant placement without provisional restorations. In addition to esthetic results are other reasons that the provisional implant is important in post-extraction crestal socket morphology. Fixed implant-supported provisional crowns are often used to customize the emergence profile and to individualize the surrounding peri-implant soft tissue. A factor for maintaining stable gingival contours is the reproduction of the shape of the root in the cervical third of the extracted tooth with soft tissue conditioning does improve the final esthetic result. It was described more technique way to replace missing teeth with dental implant which is designed to replicate the natural tooth root and crown of the natural tooth. This procedure preserves the gingival mucosa and bone with no damage to adjacent teeth. Other concepts of manufacturing the healing abutment were described to solve a lot of aesthetical and crestal socket morphology of what an immediate implant placement involve.
The anatomic harmony abutment ultimately allows for more predictable final restorations by providing the dental laboratory a restorative profile and blueprint for the definitive abutment, thus idealizing the final restoration. A lot of outcomes for the clinicians, patients, dental technician and prosthodontics dentist can be considered. This individualized, anatomical healing abutment copy and preserve the cervical tooth anatomy, is no need for suture after the surgical part (considering this, there will be a better healing for the soft tissue), preserve the soft and hard tissue after the extraction, may improve the restorations and raising the papillae. Thus, the predictability of final restorations is increase by reduce the treatment time, reduce the surgical operations and obtain the satisfaction for the patient. The adequately contoured implant restoration to the corresponding tooth anatomy may be a viable option for preserving the bone and the gingival architecture.
Conventional procedure for implant placement involves extraction of offending tooth, waiting 2-4 months for extraction socket to heal, insertion of implant, and again waiting for 3-6 months for integration of implant with surrounding bone; after this procedure, another surgery is necessary to expose the implant and to place a prosthetic abutment. Taking this consideration using anatomic healing screw abutment we eliminate the need for a second stage surgery and may provide a platform to promote periimplant soft tissue healing and minimize remodeling. Aim of this study was to compare the conventional healing screw with custom healing screw to solve problems were the immediate implant placement doesn’t reach the primary stability for immediate loading. In this way was approach an immediate customized healing screw fabrication. This concept can be used in all regions in oral cavity, for fabrication of a customized healing anatomic screw to maintain the crestal socket morphology
The study clinic was conducted at the Dental Implantology Clinic in Timisoara, Romania and included a group of 24 adult patients aged between 25 and 56 years. The medical and scientific staff that participated in this research were empowered, certified and approved in the field of interest (competence in implantology) to minimize possible negative effects. All patients accepted to participate in the study, signing a written informed consent. Patients who presented non-restorable tooth with good apical bone volume and keratinized soft tissue were eligible for this study. Twenty-four patients who underwent single tooth extraction and single immediate implant placement were included in the study (Figure 1a). The tooth was removable by sectioning and elevation with minimal traumatic technique using piezo surgery kit without disturbing the papillary tissue (Figure 1b). After removal, the alveolar socket was inspected to determine the quantity of furcation bone and was determining maximum drill depth. To remove any periodontal ligament remnants and granulation tissue a raspatory was used also to stimulate socket bleeding. Implant site preparation procedures for the osteotomy were performed using standard implant system protocol and respect the position in central fossa for ideal restorative design (Figure 1c).
Figure 1: Surgical step of extraction and positioning the implant: a – clinical view of tooth on day of removal; b - the alveolar socket and quantity of furcation bone; c – correct positioning the future implant.
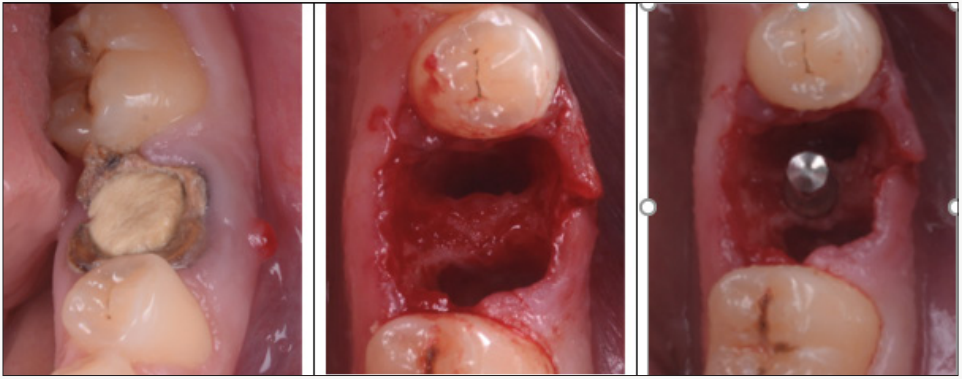
Figure 4: Technique to obtain custom healing screw: a - abutment fixed to implant; b - composite is injected around implant abutment; c – mark the buccal site.
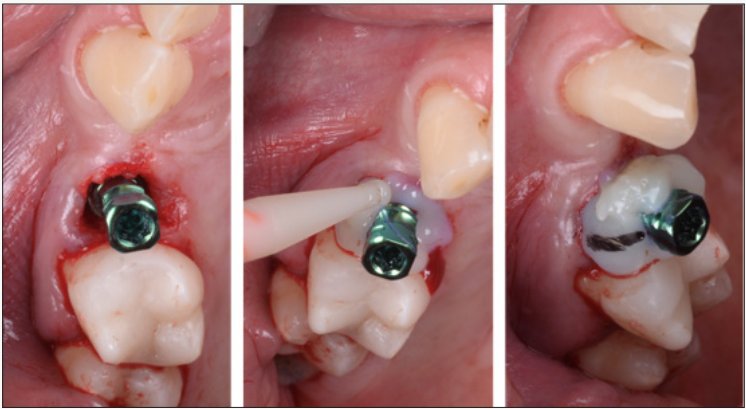
The dental implants used were internal hexagonal connection (TSV, Zimmer Biomet, US) with the 4.1 and 4.7 mm diameter and 10, 11.5, 13 mm length. In all cases the implants were inserted without any gingival flap elevation for insertion of the implants (Figure 2). Twelve patients were treated with conventional healing screw after immediate implant placement (control group) and 12 were treated with screw-retained custom healing abutment (test group) (Figure 3). The last one on the test group has also the temporary abutment attached that supply as insertion abutment. After grafting the alveolar socket around inserted implant with allograft (Bio-oss, Geistlich, Switzerland) material, a dual curing composite resin material (Protemp 4, 3MEspe, US) was injected into adapted to the abutment (Figure 4). This material takes the gingival shape of the socket until marginal position. After polymerization a buccal orientation mark was created into the composite to assist the restorative dentist with replacement after removal. The abutment was removed, and the final contouring was performed with lightcured composite (Flow, 3MEspe, US) and finishing with laboratory burs (Figure 5). Until fixation the custom healing screw the implant cover screw is temporarily placed. After finishing, the custom healing is screwed in oral cavity with a torque of 25Ncm.
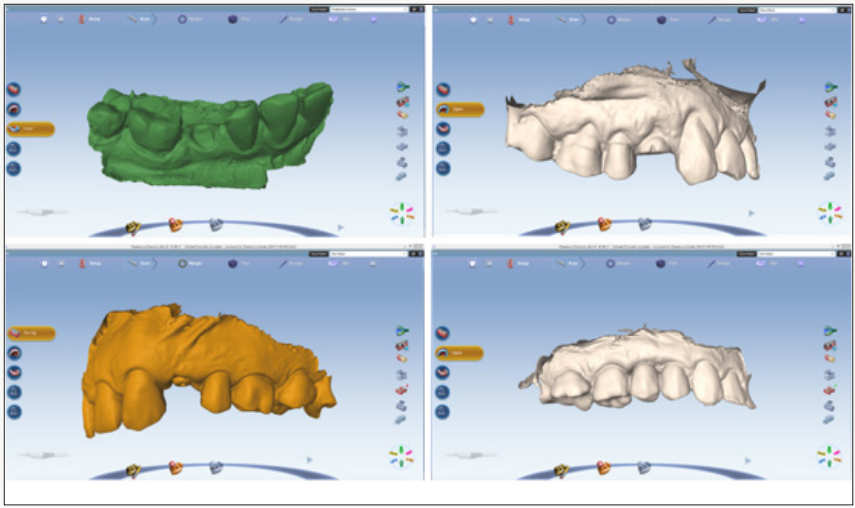
By using this type of abutment, we can obtain a short-term barrier by circumferential seal. The abutment access hole can be close by using flowable composite or interim light polymerizing restorative material such as Telio CS Inlay/Onaly (Telio, Ivoclar Vivadent AG, Liechtenstein). Six months after the implant insertion phase, impressions were taken utilizing an implant transfer technique. Prosthetic restorations were delivered 2-3 weeks after impression. All patients received screw-retained, implantsupported, monolithic lithium disilicate (e.max Press, Ivoclar Vivadent) single crowns. In all cases, the screw access holes were closed with ceramic inlays. Evaluating of the peri-implant soft tissue remodeling was performed by intra oral digital impressions (PlanScan, Planmeca, Finland). A set of 3D intraoral scanning digital system was obtained during: before tooth extraction, at implant placement, at 6 months after insertion and with final restorations (Figure 6). Analysis of the soft tissue level was measuring the comparing situations from placements until final using MeshLab software. The results were determining by using three reference points for accurate comparison. Remodeling amounts (μm) was to measure the max loss in vertical and horizontal of soft tissue.
Figure 6: Evaluation of soft tissue remodeling using digital impressions: a - before tooth extraction; b - at implant placement; c - at 6 months after insertion; d - with final restorations.
Statistical analyses were performed using OS X El Capitan, version 10.13.6 software (Apple Inc., California, U.S.A.). The significance of the differences observed was evaluated using oneway analysis of variance (ANOVA). P-value ≤0.05 was regarded as statistically significant. All statistical calculations are described in the tables and the results are presented as the mean, standard deviation (SD), and minimum and maximum values of the measured data. Differences in the proportion of patients with prostheses failures implant failures, and any complications were compared between groups using Fisher’s exact test. Comparisons between the measurements taken at each follow-up one of this is the osseointegration period: first time at implant placement with 6 months after placement and second time on the prosthetic phase - after 6 months of placement with final restorations.
A total of 24 patients that were in this study all of implants remained osseointegrated. All the patients were followed-up for at least 1 year. Implants and prosthesis survival rates at 1 year were 100%. A minimal marginal soft tissue loss was observed over time in cases of implants with customized healing screw. With conventional healing screw, soft tissue remodeling around the implants is observed. One-way ANOVA showed significant differences among the vertical and horizontal loss between these two groups (Table 1). The custom healing abutments maintained 360-degree soft-tissue shape over this follow-up period.
Immediate implant placement after extraction of tooth with early loading has become more common. The advantages of this procedure include fewer surgical interventions, reduction in overall treatment time, reduced soft and hard tissue loss, and psychological satisfaction to the patient. Customizing the healing abutment on the immediate implant placement after tooth extraction is more predictable for the future restoration, for the soft tissue and for all local architecture (this procedure preserves the gingival mucosa and bone). For adopting the conventional technique are imperious necessaries to do a buccal rotational flap to improve the implant site in the esthetic zone and increase gingival tissue thickness. The implant site is improved; the gingival thickness increased, the gingival level enhanced and the emergence profile developed. Customized immediate posterior healing abutments not only support local anatomy during the osseointegration phase, but also allow for straightforward access to the implant during the restorative phase. After osseointegration, the result is an anatomic representation that mimics the emergence profile of the natural dentition.
The success of early loading implants may not be compromised by placement in fresh extraction sockets as long as history of marginal periodontitis is avoided. The emergence profile of the implant-supported restoration derives a critical effect on peri-implant tissue health hygiene and esthetics. Immediate provisionalization allows for healing and maturization of tissue. It is known that once the restoration in removed from the implant platform, the soft tissue collapses vertically and horizontally. With the temporary restoration we guide and keep the contour of the soft and hard tissue. The immediate implant placement saves time, involve less invasive surgical procedures, the minimal soft tissue and crestal bone loss, and considerably very good esthetic outcome and excellent success rates. The immediate loading implant placement preserves the vertical existing osseous and maintains the gingival architecture. The greatest horizontal facial bone thickness change was noted at the implant platform level, in part because horizontal facial bone thickness change is correlated to the initial vertical facial bone level and the change in vertical facial bone level at that level.
Using an immediately placed provisional restoration with cervical contours of the extracted tooth at the time of implant placement may provide a platform to promote peri-implant soft tissue healing. The use of anatomically contoured provisional restorations may minimize remodeling of the buccolingual ridge dimension. Another technique describes the use of the patient’s natural teeth extracted and used as provisional immediately after the implants had been placed. The possibility of using the patient’s extracted teeth as provisional teeth during the period of osseointegration, preserving aesthetics and favoring gingival tissue healing with a correct emergence profile and maintenance of the gingival papillae. The contraindications of immediate loading implant placement involve the presence of purulent exudates at the time of extraction, adjacent soft tissue cellulites and granulation tissue, the lack of an adequate bone apical to the socket, the adverse location of the mandibular neurovascular bundle, maxillary sinus and nasal cavity.
Another factors that leads to the decision of not doing an immediate loading implant placement are poor anatomical configuration of remaining bone and primary stability less than 35Ncm. In this way is very important to use a custom anatomic healing screw. It is the author’s opinion that custom healing abutments and provisional implants ideally should be placed by the surgeon to capture the anatomy present at the time of extraction and should be viewed as the final step in the implant surgery.
Based on the outcomes of the present study, the correct design of a healing abutment is important for maintaining the emergence contour immediately after extraction and implant placement. A significant difference was observed between the standard and customized healing screw. When an immediate placement of end osseous implants into the extraction sockets with this method we can obtain a custom seal to retain the graft particles. Selection between provisional restoration and customized healing abutment is only based on esthetic considerations.
This work was supported in part by a project grant, number: P III-C5-TC-2017-03-ERPOCSI.


