Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
Mahaman Moussa*
Received: May 06, 2018; Published: May 15, 2018
*Corresponding author: Mahaman Moussa, Department of Adult Health Nursing Course, King Saud University, Saudi Arabia
DOI: 10.26717/BJSTR.2018.04.001074
Background: In 2013, approximately 25,029 liver transplants were conducted in 112 international states and countries, including Saudi Arabia. Post liver transplant patients may experience higher health related quality of life (HRQOL), compared to preoperative status, for up to 20 years. Multiple researchers have found that patient engagement in physical activity improves their HRQOL. However, post liver transplant patients often do not engage in physical activity. In addition, in Saudi Arabia, no intervention is in place to promote physical activity among this population.
Purpose:The purpose of this project was to determine if a walking program (physical activity) for post liver transplant patients improved HRQOL for this patient population.
Methods: This study was a prospective evaluation of the walking program. The target population was post liver transplant patients from one tertiary hospital in Riyadh. Patients included were between the ages of 18 and 69 years. Data on patients’ levels of physical activity were collected using the International Physical Activity Questionnaire (IPAQ) and data on patients’ HRQOL were collecting using the SF-12 Version 1.
Results: A total of 20 patients were invited to participate in the study. Of those 20 patients, 15 patients signed the consent. All the 15 patients who participated in this study were able to complete the 7 week walking program. SF-12 and IPAQ data were collected for all 15 patients at Week 1 and at Week7. At baseline, patients’ metabolic equivalent (MET) scores ranged from 99 to 628.5 and at Week 7, their scores ranged from 1402.5 to 3006.Patients showed improvement in all HRQOL domains except the emotional domain.
Keywords: Chronic Liver Disease, Liver Transplant, Post Liver Transplant, Liver Transplant and Physical Activity, Liver Transplant and Health-Related Quality of Life
Life-threatening, end-stage liver disease requiring transplantation is common across the globe. In 2013, approximately 25,029 liver transplants were conducted in 112 international states and countries including Saudi Arabia, the clinical site for this project [1]. The estimated number of annual liver transplants conducted in Saudi Arabia ranged between 700 and 1,200 [2]. According to Al-Sebayel, doctors at King Faisal Specialist Hospital and Research Center (KFSH) in Saudi Arabia perform between 2 and 3 transplants per week [4]. Between the year 2001 and 2012, approximately 480 patients underwent liver transplantation surgery at KFSH [3]. Successful liver transplantation may mend liver function, but improving post-transplant quality of life often requires physiotherapy, which can reduce weight gain, increase muscle strength, enhance sleep and decrease fatigue, and improve healthy aerobic activity [4]. Overweight or obese post-transplant patients may experience additional complications during the postoperative period, such as metabolic syndrome and cardiovascular events [5].
Evidence indicates that immediate postoperative and ongoing exercise rehabilitation is necessary to restore physiological functioning to healthy levels post transplantation [4]. Ongoing post-transplant physiotherapy or exercise therapy also can have positive psychological effects [4]. However, some post-transplant patients are unable to adhere to lifestyle interventions and rely on medications to manage their symptoms [5]. Nurses and nurse practitioners are in a unique position to use evidence based strategies to enrich post liver transplant care. Stated more specifically, nurses and nurse practitioners in liver transplant facilities can implement interventions to prompt physical activity in post-transplant patients as a means of improving health related quality of life (HRQOL)
Chronic liver disease is traditionally referred to as cirrhosis [6]. Etiologies for cirrhosis include alcohol abuse, infection, andgenetic and autoimmune diseases [6]. The two most common non-alcoholrelated causes of chronic liver disease are non-alcohol fatty liver disease and hepatitis [6]. Approximately 240 million people worldwide have chronic hepatitis B virus [7] and130-150 million people have chronichepatitis C [8]. People infected with HIV are at an increased risk of contracting hepatitis C [8]. According to WHO [9], approximately 36.7 million have HIV/Aids. Although exact percentages vary from country to country, rates of NAFLD in Eastern and Western Countries have been reported to range between 10 and 30% [10]. Between1982 and 1990, Al-Quirain et al. [11] found rates of NAFLD among patients at KFSH to be 7.2%; between 1985 and 1990, El-Hassan et al. [12] found rates of NAFLD to be 9.7%; and in 2009, Al-hamoudi et al. [13], found rates of NAFLD to be 16.6%. In 2002, among patients with Type 2 diabetes, Akbar and Kawther (2003) found rates of NAFLD to be 55%. This elevated rate may be due the fact that Type 2 diabetes significantly increases a patient’s risk of developing NAFLD Akbar & Kawther.
According to Mohammed Al-Sebayel, the chairman of Liver Transplantation and Hepatobiliary-Pancreatic Surgery Department at KFSH, the high rates of chronic liver disease in Saudi Arabia are in part the result of increasing rates of NAFLD Ahmad, [2]. Al-Sebayel explained that NAFLD disease has become common place in Saudi Arabia as the result of people’s lack of exercise and engagement in unhealthy lifestyles over the last 2 decades Ahmad, [2]. Although NAFLD is responsible for the increase in rates of liver disease in Saudi Arabia in recent years, hepatitis B and C as well as inherited and metabolic diseases also contribute to the overall rate of liver disease in Saudi Arabia [2]. Since 2008, rates of hepatitis in Saudi Arabia have decreased Ministry of Health, Saudi Arabia [14]. The MOHSA [7] credits the decline to a multitude of environmental, health awareness, and health regulation initiatives throughout Saudi Arabia. Childhood immunization against the disease has been notably effective [15,16]. The release of a new hepatitis C treatment is expected to contribute to further decreases in the incidence of hepatitis C in particular [14].
According to the [17], in 2011, there were 4,494 reported cases of hepatitis B and 2,328 reported cases of hepatitis C. Those numbers increased in 2012, to 4,609 and 2340, respectively, before a noticeable trend in reduced rates became apparent [17]. In 2015, there were 3,486 reported cases of hepatitis B and 1,327 reported cases of hepatitis C [17]. Of the 3,486 cases of hepatitis B reported in 2015, 754 cases were for nonnative Saudi Arabians and 2,732 cases were for native Saudi Arabians [17]. Of the 1,327 cases of hepatitis C reported in 2015, 389 cases were for nonnative Saudi Arabians and 938 cases were for native Saudi Arabians [17]. Although the majority of people in Saudi Arabia in 2015 who had hepatitis B were between the ages of 15 and 45, the majority of people who had hepatitis C were 45 years old or older [17]. For both nonnative and native Saudi Arabians who had hepatitis B or C in 2015, more female residents were infected than male residents [17]. The number of cases of hepatitis B reported in 2015 ranged from zero in Hafr Al-Baten and Jazan to 463 in the Eastern region of Saudi Arabia [17]. The number of cases of hepatitis C reported in 2015 ranged from zero in Jazan to 237 in Makkah [17].
Patients with chronic liver disease (cirrhosis) experience a variety of physiological symptoms [5]. These symptoms can include “loss of muscle mass, low bone mineral density, reduced muscle strength, increased levels of fatigue and decreased aerobic capacity” [4]. Severity of symptoms generally increases as the disease progresses [4]. The Model for End-Stage Liver Disease (MELD) is a formula based on serum creatinine, serum bilirubin, and international normalized ratio that is used to calculate an illness or severity score indicating potential mortality (within 3 months) and can be used to predict patient survival post transplantation [18]. Scores range from less than or equal to 9 to greater than 40 [19]. Those with scores less than or equal to 9 have a 4% chance of mortality in 3 months, while patients with scores equal to or greater than 40 have a 100% chance of mortality in 3 months [19].
In general, post liver transplant patients may experience higher HRQOL, compared to preoperative status, for up to 20 years [20]. Part of this higher HRQOL may be due to the slowing or reversal of muscle atrophy following liver transplantation [21]. The greatest improvements to quality of life are evident in the first year following transplantation [22]. Although research on HRQOL for liver transplant patients following surgery in Saudi Arabia is limited, Alkatheri et al. (2015) has reported that liver transplant patients in Saudi Arabian (N = 154) were moderately or highly satisfied with most aspects of their lives following their transplant surgery. Of those patients, 98.7% expressed having a meaningful life,94.8% expressed enjoying life, and 93.5% expressed satisfaction with their personal relationships. Also, 91.5% expressed feeling safe, and 87.0% expressed being free from pain. A variety of factors may impact patient outcomes post-transplant, including demographic characteristics, diet, and levels of physical activity. For example, Alkatheri et al. (2015) found that male patients reported higher physical, psychological, social, and environmental HRQOL when compared to female patients. These difference were significant for the physical (p < .01), psychological (p < .05) and social (p < .001) HRQOL domains. In addition, overall, those patients with high levels of incomes and higher levels of education reported higher levels of HRQOL when compared to patients with lower levels of income and education[23].Found that changes in patients’ eating habits as the result of dietary counseling helped improve patients’ HRQOL. Using the SF-12 or the SF-36 questionnaire, multiple researchers have found that patient engagement in physical activity improves their HRQOL [23-26] stressed the importance of assessing patients for indications and contraindications to physical activity that might be counterproductive and potentially dangerous for the patient.To our knowledge no such program was previously implemented in the Saudi Arabia.
To determine whether the program was associated with an improvement in HRQOL, an HRQOL questionnaire was administered to patients before and after participating in the walking program. This study was a prospective evaluation of the walking program’s association with improved HRQOL.
The target population for this project was post liver transplant patients from a tertiary hospital in Riyadh. Patients who were included were approximately 1-monthpost-transplant. Participants were between the ages of 18 and 69 years. Patients were excluded from the walking program if they were second-time liver transplant recipients, had physical limitations such impaired mobility, had active wound in fections, or if their conditions were otherwise determined to be unstable(e.g., high liver enzymes, signs of acute rejection, electrolytes imbalances). All of the patients who met the inclusion criteria were invited to participate in the walking program during their first follow-up visit to the outpatient clinic, approximately 1 month post liver transplant. Approval to implement the program was granted by the Research Ethics Committee (REC) of the hospital.
Recruitment occurred at the patients’ 1-month post liver transplant clinic visits. As part of the recruitment process, the post liver transplant patients were provided with a copy of the consent form for review. After consent was obtained, the patients completed the baseline IPAQ and SF-12, and immediately begin to engage in the physical activity (walking) portion of the program. The goal of the walking program was for patients to walk 30 minutes a day at least 5 times a week by the end of the 7-week program and for the patients to record their walking activities in a walking log. Patients began walking immediately after enrolling in the program and began walking 5 minutes each time they walked for the first 3 days of the program. Patients increased their walking time by 5 minutes every 3 days until they reached 30 minutes of walking on Day 16. For each of the next five groups of 7 days, Days 16-22, 23-29, 30- 36, 37-43, and 45-50, patients walked for 30 minutes for 5 of the 7 days.
Data collection began during patients’ first outpatient follow-up clinic visit 1 month after the transplant and at the end of 7 weeks of participation in the walking program. Data on patients’ levels of physical activity were collected using the IPAQ and data on patients’ HRQOL were collecting using the SF-12 Version 1, a shortened version of the SF-36.
The data analysis for this study was conducted to determine if there was a relationship between physical activity and patient HRQOL and if, after participating in the walking program, patients’ levels of HRQOL improved. To make these two determinations, a McNemar’s test was conducted.“McNemar’s test is used to compare dependent proportions” [27] with a dichotomous variable (Upton & Cook, 2014).This test is particularly useful when making comparisons with a pre- and posttest design [28]. Results are presented accordingly. While patients’ demographic information were not analyzed, frequency of patient characteristics are presented both numerically and as percentages.
Of the 20 patients invited to participate in the walking program, 15 patients agreed to participate. All 15 patients were able to complete the 7 week walking exercise program and to do so without any difficulties. Participants indicated having one of eight different diagnoses: hepatitis B (n = 5), hepatitis C (n = 1), autoimmune hepatitis (n = 2), liver cirrhosis (n = 2), cryptogenic liver disease (n = 2), primary sclerosis cholangitis (n = 1), Caroli disease (n = 1) and Bilharzia liver cirrhosis (n = 1). Of the 15 participants, nine were men and six were women. The gender distribution of participants is presented graphically in Figure 1. The average age for the male patients was 47, and the average age for the female patients was 56. These numbers are presented graphically in Figure 2. The average MELD score was 29 for the men and 27 for the women.
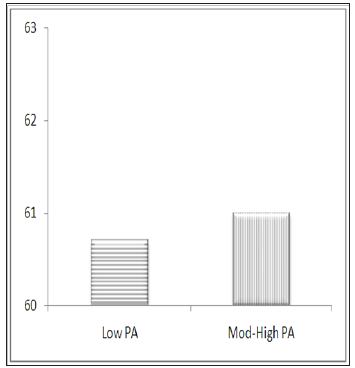
All 15 patients answered the IPAQ questionnaire at baseline and at 7 weeks. At baseline, the MET scores ranged from 99 to 628.5 and at 7 weeks the scores ranged from 1402.5 to 3006. Most of the participants walked longer or for more days than were required. Table 1 shows how many minutes the patients walked and on how many days they walked. The repeated measures analysis of IPAQ scores for physical activity (low vs. moderate/high), the coefficient of low MET score is -20 and significant p<.0001). This means that on average, those with low MET (M = 33.48) performance score as low as -20, compared to those with moderate/high MET (M = 53.49). The repeated measures analysis of IPAQ scores for physical activity (low vs. moderate/high), the coefficient of low MET score was -0.34 but not significant (p = 0.8319). This means that there was no difference in means scores for the two groups, those with low MET scores (M = 60.67) compared to those with moderate/ high MET scores (M = 61.03). The difference in average IPAQ scores between Week1 and Week 7 is shown in Figure 1. The difference between low and moderate/high physical activity for Week 1 is shown in Figure 2. The difference between low and moderate/high physical activity for Week 7 is shown in Figure 3.
Figure 2: Week 1 IPAQ scores showing the difference between low and moderate/high levels of physical activity.
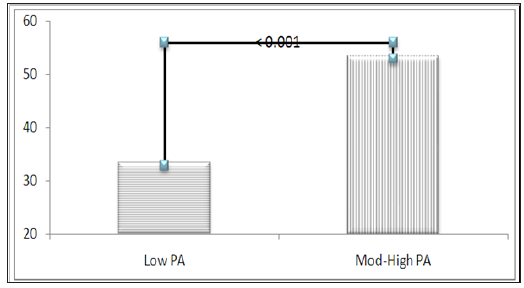
Figure 3: Week 7 IPAQ scores showing the difference between low and moderate/high levels of physical activity.
All 15 patients answered the SF-12 questionnaire at Week 1 and Week 7.The eight domains of the SF-12 are “physical functioning, bodily pain, role limitations due to physical health problems, role limitations due to personal or emotional problems, emotional well-being, social functioning, energy/fatigue, and general health perceptions” [29]. However, in this analysis, the 12 items that makes up the eight domains were analyzed individually. Also, PCS and MCS scores, summary scores for the physical and mental components, were not calculated.
At Week 1, 13 patients reported having good or fair health. At Week 7, 14 of the patients reported having excellent or very good health. The McNemar’s test statistic for this HRQOL indicator was 12, which was significant at the p = 0.0005 level. This result indicated that participation in the walking program was effective in changing patients’ overall level of perceived health(general health perceptions domain). At Week 1, all of the patients reported that their health limited them during moderate activities. At Week 7, patients did not report any health related limitations during moderate activities. The McNemar’s test statistic for this HRQOL indicator was 15, which was significant at the p = 0.0001 level. This result indicated that participation in the walking program was effective in decreasing the impact of patient health on patients’ ability to complete moderate activities (first of two items making up the physical functioning domain)[30].
At Week 1, all of the patients reported that their health limited their ability to climb stairs. At Week 7,patients did not report any health related limitations regarding their ability to climb stairs. The McNemar’s test statistic for this HRQOL indicator was 15, which was significant at thep = 0.0001 level. This result indicated that participation in the walking program was effective in decreasing the impact of patient health on patients’ ability to climb stairs (second of two items making up the physical functioning domain).
At Week 1, all of the patients reported that their health impacted their ability to accomplish all of the activities they would have liked to accomplish. At Week 7,none of the patients reported decreased accomplishment of activities due to their health. The McNemar’s test statistic for this HRQOL indicator was 15, which was significant at the p = 0.0001 level. This result indicated that participation in the walking program was effective in improving patients’ ability to accomplish all the activities they would like to accomplish (first of two items making up the role limitations due to physical health problems domain). At Week 1, all of the patients reported that their health limited the kind of work they could accomplish or the kind of activities in which they could engage. At Week 7, none of the patients reported being limited by their health with regard to the kind of work they could accomplish or the kind of activities in which they could engage. The McNemar’s test statistic for this HRQOL indicator was 15, which was significant at the p = 0.0001 level. This result indicated that participation in the walking program was effective in decreasing the impact that patient health had on the kind of work patients could accomplish (second of two items making up the role limitations due to physical health problems domain).
At Week 1, all of the patients reported that their health impacted their ability to accomplish all of the activities they would have liked to accomplish. At Week 7,none of the patients reported decreased accomplishment of activities due to their health. The McNemar’s test statistic for this HRQOL indicator was 15, which was significant at the p = 0.0001 level. This result indicated that participation in the walking program was effective in improving patients’ ability to accomplish all the activities they would like to accomplish (first of two items making up the role limitations due to physical health problems domain). At Week 1, all of the patients reported that their health limited the kind of work they could accomplish or the kind of activities in which they could engage. At Week 7, none of the patients reported being limited by their health with regard to the kind of work they could accomplish or the kind of activities in which they could engage. The McNemar’s test statistic for this HRQOL indicator was 15, which was significant at the p = 0.0001 level. This result indicated that participation in the walking program was effective in decreasing the impact that patient health had on the kind of work patients could accomplish (second of two items making up the role limitations due to physical health problems domain). reported that emotional problems caused them to work less carefully than they usually do. At Week 7,none of the patients reported that emotional problems caused them to work less carefully than they usually do. The McNemar’s test statistic for this HRQOL indicator was 2, which was not significant (p = 0.1573). This result indicated that participation in the walking program was not effective in decreasing the impact of emotional problems on the amount of work patients usually do (second of two items making up the role limitations due to personal or emotional problems domain).
At Week 1, 13 patients reported that some level of pain interfered with their normal work to some degree (a little bit, a moderate amount, quite a bit, or to an extreme extent). At Week 7, 3patients reported that pain interfered with their normal work to some degree. The McNemar’s test statistic for this HRQOL indicator was 8.33, which was significant at p = 0.0039.This result indicated that participation in the walking program was effective in decreasing the impact of pain on patients’ ability to accomplish normal work (bodily pain domain). At Week 1, 14 patients reported that they felt calm and peaceful most or a good bit of the time. At Week 7, all of the patients reported that they felt calm and peaceful all of the time. The McNemar’s test statistic for this HRQOL indicator was 14, which was significant at p = 0.0002. This result indicated that participation in the walking program was effective in improving patients’ overall sense of calm and peacefulness (first of two items making up the emotional well-being domain).
At Week 1, all of the patients reported having a lot of energy most or some of the time. At Week 7, 12 patients reported having energy all of the time. The McNemar’s test statistic for this HRQOL indicator was 12, which was significant at p = 0.0005.This result indicated that participation in the walking program was effective in improving patients’ level of energy (energy/fatigue domain). At Week 1, 11 patients reported that they did not feel downhearted or blue any of the time. At Week 7, all of the patients reported that they did not feel downhearted or blue any of the time. The McNemar’s test statistic for this HRQOL indicator was 4, which was significant at p = 0.0455.This result indicated that participation in the walking program was effective in improving patients’ overall outlook on life (second of two items making up the emotional well-being domain).
At Week 1, 10 patients reported that physical health or emotional problemsdid not interfere with their social activities any of the time. At Week 7, all of the patients reported that physical health or emotional problems did not interfere with their social activities any of the time. The McNemar’s test statistic for this HRQOL indicator was 5, which was significant at p = 0.0253. This result indicated that participation in the walking program was effective in decreasing the extent to which physical health or emotional problems interfered with patients’ social activities (social functioning domain).
All 15 participants of this project were able to complete all 7 weeks of the walking program. Also, all patients were able to complete their walking log and return it at Week 7. Results of data analysis showed a decrease in low levels of physical activity from Week 1 to Week 7, and an increase in moderate/high levels of physical activity from Week 1 to Week 7. These results suggest that the walking program was significantly improved levels of physical activity among post liver transplant patients at KSFH.
All 15 patients completed the SF-12 at Week 1 and Week 7. Results showed significant improvement for 10 of the 12 individual items on the SF-12. Specifically, results showed that participation in the walking program (a) improved patients’ perceptions of their general health, (b) decreased the impact of health on patients’ ability to complete moderate activities, (c) decreased the impact of health on patients’ ability to climb stairs, (d) improved patients’ ability to accomplish all the activities they would like to accomplish, (e) decreased the impact of health on the kind of work patients could accomplish, (f) decreased the impact of pain on patients’ ability to accomplish normal work, (g) improving patients’ overall sense of calm and peacefulness, (h) improved patients’ level of energy, (i) improved patients’ overall outlook on life, and (j) decreased the extent to which physical health or emotional problems interfered with patients’ social activities. The walking program did not significantly decrease the impact of emotional problems on patients’ ability to accomplish work or decrease the impact of emotional problems on the amount of work patients usually do. However, overall, these results were consistent with the results of previous studies that showed physical activity can help improve patients’ HRQOL [16,17,23,24].
The results of this projectshow that a walking program that engages post liver transplant patients in physical activity is feasible in an outpatient clinic setting. Also, the results of this project show that this walking program can have a significant impact on the amount of physical activity in which post liver transplant patients engage as well as on patients’ HRQOL. Healthcare providers should promote the incorporation of this walking program into their daily practice. By educating patients and engaging them in this structured physical activity program, nurses can help impacted the HRQOL for post liver transplant patients.


