Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
Masatomo Kaneko1,2, Eiichi Konishi3, Toru Matsugasumi4, Hidefumi Taniguchi5, Akira Onishi2, Hideo Seki6, Emi Inui2, Naoki Imada2 and Osamu Ukimura1
Received: February 19, 2018; Published: February 22, 2018
*Corresponding author: Masatomo Kaneko, Department of Urology, Kyoto Prefectural University of Medicine, 602 8566 Kajii-cho, Kamigyo-ku, Kyoto, Japan
DOI: 10.26717/BJSTR.2018.02.000788
An 89-year-old woman was admitted with complaining of fever and anuria. Physical examination revealed pyuria and left costovertebral angle (CVA) tenderness. A CT scan showed atrophy of the right kidney, and perirenal fat stranding in the left abnormally enlarged kidney. Based on a clinical diagnosis of acute kidney injury (AKI) due to acute pyelonephritis (APN) in the left, intravenous antibiotics, fluid, and hemodialysis was started. After healing of APN, she could not wean from hemodialysis. In order to prevent AKI due to APN from progression to end stage renal disease (ESRD), further studies about new treatment are needed.
Keywords: End Stage Renal Disease; Acute Kidney Injury; Acute Pyelonephritis; Solitary Kidney
Abbrevations: ESRD: End Stage Renal Disease; AKI: Acute Kidney Injury; APN: Acute Pyelonephritis; CVA: Costovertebral Angle; KDIGO: the Kidney Disease Improving Global Outcomes Introduction
APN is an inflammation of the kidney and renal pelvis [1]. APN frequently cause mild AKI, but, irreversible renal function loss is rare [2]. It is presumed that solitary kidney, pregnancy, indwelling urinary catheter or use of non-steroidal anti-inflammatory drugs (NSAIDs) is the cause of severe AKI due to APN [3]. We reported a case of 89-year-old woman with solitary functioning kidney who was diagnosed AKI due to APN.
An 89-year-old female was referred to us with complaining of fever and anuria for one day. She had the past history of chronic kidney disease (CKD) stage G4A1, and hypertension. She had not taken NSAIDs. When she was admitted, her temperature was 37.6°C, blood pressure 131/46 mmHg, pulse 60/min. On physical examination, she had left CVA tenderness, nausea, vomiting, and disturbance of consciousness. She denied other symptoms. Laboratory analysis showed white blood cells (WBC) 12 x 103 /μL, hemoglobin 8.0 g/dL, hematocrit 24.0%, platelets 220 x 103/μL, neutrophils 88%, blood urea nitrogen (BUN) 85mg/ dl, creatinine 6.75mg/dl, C-reactive protein (CRP) 20.07mg/dl,plasma sodium 125m Eq/l, potassium 6.2m Eq/l, chloride 99m Eq/l. Urinalysis showed urine protein (2+), specific gravity ≧1.030, red blood cells (RBC) 5-9/high-power field (HPF), WBC 100/HPF. Immunoglobrins and autoantibodies associated with glomerular nephritis were all normal level.
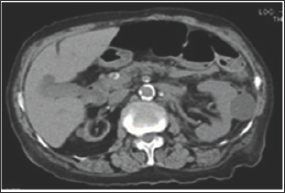
A non-contrast abdominal CT scan revealed the atrophic right kidney and perirenal fat stranding around left enlarged kidney. Hydronephrosis and urolithiasis was not detected (Figure 1). The diagnosis of AKI stage 3 in the Kidney Disease Improving Global Outcomes (KDIGO) classification due to APN in solitary functioning kidney was suggested. Intravenous dose of ceftriaxone 2g daily, hydration, furosemide 40mg, calcium gluconate 8.5% 10mL, and 6 units of regular insulin in 50ml of 50% dextrose were initiated. In spite of these treatments, anuria was prolonged, her conscious level decreased, and blood chemistry showed creatinine 7.3mg/dl and plasma potassium 6.2mEq/l on her 2nd hospital day. Hemodialysis was started. During hospitalization, Escherichia coli were cultured from her urine and blood. According to result of the culture, ceftriaxone was changed to piperacillin/tazobactam 2.25g IV q12hr on the 5th day. Her CRP and WBC were almost normalized on day 20. After recovery from APN, anuria continued, therefore she could not wean from hemodialysis. Because of patient's refusal, renal biopsy was not performed.
Figure 1: A CT scan revealed the atrophic right kidney, and perirenal fat stranding around the left enlarged kidney.
Recent study revealed AKI in elderly increased the incidence of ESRD, and the risk among patients with both AKI and CKD was higher [4]. It is considered that advanced age, increased Charlson comorbidity index score [5] during AKI episode, hypoalbuminemia, past history ofdiabetes mellitus, hypertension, heart failure, and CKD are the risk factor of CKD progression after AKI [6]. The mechanism of AKI to CKD progression has not been clarified. Takaori et al. recently indicated that selective proximal tubule injury can trigger fibrosis, reduced Epo production, glomerulosclerosis, atubular glomeruli, and distal tubule injury by the animal model of CKD [7]. In this case, an elder woman whose medical history included hypertension and CKD with APN in solitary kidney lost renal function irreversibly in spite of prompt treatments. Treatments for preventing AKI to ESRD progression has not been developed, it is presumed to protect proximal tubules and treatments of fibrosis are effective [7].
In order to prevent acute kidney injury due to acute pyelonephritis from progression to end stage renal disease, further studies about new treatment are needed.


