Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
Asmatullah Khan1, Syed Kamran Ali Shah1*, Syed Shahid Noor2 and Muhammad Kazim Rahim Najjad3
Received: January 07, 2018; Published: January 17, 2018
*Corresponding author: Syed Kamran Ali Shah, Department of Orthopaedics, K-Block, Liaquat National Hospital, Stadium road, Karachi, Pakistan
DOI: 10.26717/BJSTR.2018.02.000668
Objective: To evaluate the effectiveness of Continuous Passive Motion in adjunctive with conventional physical therapy in early post operative Total Knee Arthroplasty patients.
Methods: Total 150 patients were enrolled, randomly selected in two groups, CPM (n=73) and Control group (n=75), as 2 patients from CPM group refuse to participate in study. In control group patients received conventional physical therapy intervention alone, while in CPM group patients received conventional physical therapy intervention along with CPM application. Assessment of all patients were carried out twice by experience physical therapist, once at the preoperative visit 2 weeks prior to TKA for baseline measurements and second at discharge after 7 days post operatively. Outcome assessed among both group by assessing active knee range of motion primarily flexion and extension by using Goniometry and as secondarily outcome pain, stiffness and functional difficulty by using WOMAC questionnaire score.
Result: Out of 150 patients, 148 were analyzed in the study to compare the effectiveness of CPM along with standard physiotherapy and physiotherapy alone in early postoperative period after TKA. No statistical significant difference found in Flexion and extension pre operative 2 weeks prior to surgery and post operative assessment at discharge after 7 days among both groups, as p-value was found to be insignificant. Similarly WOMAC Score (for Pain, Stiffness and functional difficulty assessment) were evaluated among both groups, it was noted that there were decreased in scores but it was also statistically insignificant.
Conclusion: Continuous Passive Motion does not provide an additional benefit over the conventional physical therapy interventions employed in an inpatient rehabilitation facility for patient following TKA, more specifically in patients had poor initial knee range of motion specially flexion following surgery, perhaps it increases the financial burden to the patients. So we concluded that Conventional physical therapy alone could be the convenient and sufficient method for rehabilitation in early post operative TKA patients. As it was a single centre prospective study and small sample size; therefore the results of the present study should be exercised with caution.
Keywords: Continuous Passive Motion; Conventional Physical Therapy; Knee Range Of Motion; Total Knee Arthoplasty
Abbreviations: CPM: Continuous Passive Motion; WOMAC: Western Ontario and McMaster Universities; TKA: Total Knee Arthtoplasty; SPSS: Statistical Package for Social Sciences; BMI: Body Mass Index
Osteoarthritis of knee is one of common issue in elder population to cause pain and disability, which can be addressed by total knee replacement surgery for advance osteoarthritis. Number of Total Knee Arthoplasty surgeries will increase to 3.5 million by the calendar year 2030 and simultaneously it will create influential needs for post operative rehabilitation services [1]. For last 25 years continuous passive motion is involved in clinical debate for its merits following knee replacement and now still controversy exists within the current literature for its benefits. Even in various studies no beneficiary effects of CPM were reported when it compare to physical therapy [2]. The main purpose of rehabilitation in total knee arthroplasty is to achieve early knee range of motion with comfortable and pain free mobilization of the patient.
Continuous passive motion (CPM) has been frequently used as part of the postoperative care regime following knee arthroplasty with the aim to increase knee joint mobility and improve postoperative recovery despite little conclusive scientific evidence [3-6]. Clinically meaningful differences between standard physiotherapy and standard physiotherapy combined with CPM are reported to be at least 5° [3]. CPM treatment has been introduced since early 1980s to promote joint mobilization and improve knee flexion and theoretically CPM can maintains range of motion and reduces post operative swelling [6]. The motive of Continuous passive motion in post operative rehabilitation period of knee arthplasty is to gain maximum knee joint mobility and fasten recovery [3]. Conflicting research findings have generated an ongoing debate on its usage. CPM efficacy has been studied in large group of patients to recognize its importance in postoperative period. Range of motion at the knee joint especially flexion was the primary outcome.
That primary outcome was observed for long and short period of time. It was concluded by many authors that CPM use for longer time has no use as compared to shorter duration [7]. The Cochrane Review of Harvey et al. reported evidence for small short-term effects of CPM on active and passive knee flexion range of motion (aFL, pFL) of 2° and 3°. The range of motion is a primary indicator of a successful TKA and is directly related to functional outcomes [8,9]. Adequate knee flexion up to 90-120° is required for activities of daily living such as sit to stand transfers and climbing stairs [9]. Consequently, most research on the effectiveness of CPM focuses on range of motion as the primary outcome variable [10-14]. The attainment of at least 0-90° range of motion is the goal upon hospital discharge and a more functional range of 0-120° should be attained upon completion of postoperative physiotherapy.
Nevertheless, Harvey et al. suggested that the beneficial effects of CPM on range of motions are too small to be practically relevant. Passive mobilization of knee joint in post TKA period does not encourage patients to actively participate in knee joint mobility. Comparison of active range of motion and standard physiotherapy with physiotherapy and CPM application in immediate postoperative period are lacking in present literature [12]. This Randomized control study was conducted to compare the effectiveness of CPM along with standard physiotherapy and physiotherapy alone in early postoperative period after TKA.
This Cross Sectional study was conducted from July 2015 to June 2016 at orthopedics surgery department of Liaquat National Hospital, Karachi. Patients were registered using a predesigned Performa. Approval from institutional ethical review committee was taken prior to commencement of the study. Formal informed written consent was obtained from patients registering in the study. Using a non probability, consecutive sampling technique and 150 patients were registered for the study.
i. Either gender
ii. Patients with knee arthritis, expecting primary TKA
iii. Ambulatory
iv. Literate
v. Patients with previous major lower-limb surgery (like contra lateral TKA or total hip replacement) included but previous surgery had performed at minimum of 1 year before the current TKA.
i. Patients with medical conditions or diseases that could interfere with test performance (like collaboration or comprehension problems, neuromuscular or neurodegenerative disease)
ii. Revision and complex primary knee requiring extensive tissue dissection
iii. Concurrent intervention during surgery that could interfere with outcomes (like collateral ligament repair)
iv. Infection of the affected knee
v. Any major health complications during the hospital stay (like pulmonary embolism, heart attack, problems with scar healing).
Patients were randomly selected in two groups, CPM (n=73) and Control group (n=75) as 2 patients from CPM group refuse to participate in study so 73 patients were analyzed in CPM group. Patients in control group received conventional physical therapy intervention alone, while patients in CPM group received conventional physical therapy intervention along with CPM applications. Assessment of all patients were carried out twice by experience physical therapist, once at the preoperative visit 2 weeks prior to TKA for baseline measurement and second at discharge after 7 days post operatively. For each participant, anthropometric, personal, and clinical characteristics were reported, including sex, age, weight, height, social status, previous disease or surgeries, and time from the onset of symptoms. A questionnaire also was administered to measure the frequency and intensity of physical activity usually performed by the patients.
The same measurements were taken at baseline and at discharge. The primary outcome was maximal active range of motion of knee flexion in a seated position. The secondary outcomes were active range of motion of knee extension, Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) questionnaire scores was used to assess pain, stiffness and functional difficulty. Assessments were carried by experienced physical therapists that were unaware of group assignment and similar assessments repeat at discharge. The range of motion measurement was taken with a 1-degree-increment goniometer. Its center of rotation was placed in line with the center of the knee, the fixed arm aligned with the greater trochanter and the mobile arm aligned with the lateral malleolus. The criterion validity and the intra-tester and intertester reliability of data obtained with the goniometer have been demonstrated to be high [15].
To maximize reliability, the patient’s position was standardized as follows, the patient was seated on an adjustable table, the foot of the affected leg was placed on a cloth, and the contra lateral foot was placed on an 7.6 to 15.2cm high bench. Subjects were asked to actively bend their knee by sliding their foot backward to the maximum range of motion tolerated. The same method was applied for the extension movement, except that patients were lying supine on the adjustable table and had to actively slide their foot forward on a wooden board to the maximum range of motion tolerated. Two trials were performed for both flexion and extension range of motion measurements. If the difference between those trials was more than 5 degrees, a third trial was performed and the mean of the 2 closest ranges of motion measurements was registered. All evaluators were required to participate in a standardization session for the entire procedure of range of motion measurements.
The WOMAC (Western Ontario and McMaster Universities) questionnaire is a self-administered, activity-based, and lower-limb specific questionnaire that contains 24 items covering pain (n 5), stiffness (n 2), and functional difficulty (n 17). Excellent validity and reliability have been shown with many populations and specifically with TKA and total hip arthroplasty populations. At discharge, several questions regarding functional difficulty were excluded from the original form as getting in and out of the car and the bath, shopping, and managing light or heavy household work as patients were unable to attempt these tasks at the early postoperative stage.
CPM group patients were receiving one daily CPM session, beginning on the second day after TKA until discharge or day 7. Physiotherapist applies the CPM device, and the procedure was standardized. Subjects lay supine in their bed, and the CPM device was placed under the affected leg with the knee extended. For stability, one strap surrounded the patient’s thigh, another strap surrounded the patient’s lower leg, and the apparatus was prevented from sliding down by the edge of the bed. CPM was used for 35 minutes continuously, including a 5-minute warm-up period and in the control group patient’s only conventional physical therapy was used. Statistical package for social sciences (SPSS 21) was used for data compilation and analysis. Mean (SD) was calculated for quantitative variables. Frequency and percentage were calculated of qualitative variables chi-square was applied to see association. Independent t-test was applied to see significance in mean difference by considering P-value ≤0.05 as significant.
Pre operatively CPM group have mean knee flexion 61.3±7.8 and mean knee extension -4.7±3.4 as compared to Control group having 63.6±7.4 knee flexion and -4.6±3.3 extension of knee which were statistically insignificant as p-value for flexion 0.076 and for extension 0.861 were more than 0.5. Out of 150 patients, 148 were analyzed in study to compare the effectiveness of CPM along with standard physiotherapy and physiotherapy alone in early postoperative period after TKA. Independent t-test was applied to see significance in mean difference. P value ≤0.05 was considered as significant. In CPM Group 22(30%) were Male 51(70%) were female while in Control group 17(23.2%) were male and 58(77.3%) were female.
The mean age of study subjects in CPM Group was 62.45±8.79 years while the mean age of Control group was 63.6±7.4 years. Mean BMI of patients in CPM group was 34.26±5.47 while in Control group was 30.26±5.47. In Both groups there is no statistical significant difference found in means of age, BMI and gender. There was no statistically significant difference found among both groups on pre and post operative assessment of patients with knee flexion and extension. Similarly WOMAC Score were also evaluated pre and post operatively among both groups and it was noted that there were decreased in scores (Figure 1) but it was also statistically insignificant (Tables 1-3).
Figure 1: Mean scores pre operatively and post operatively.
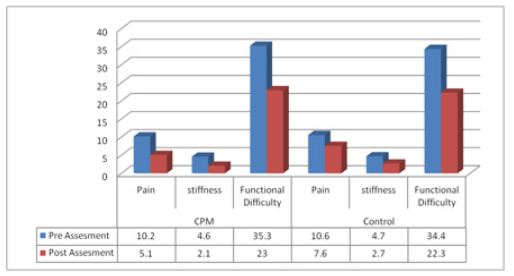
Table 1: Demographic of patients.
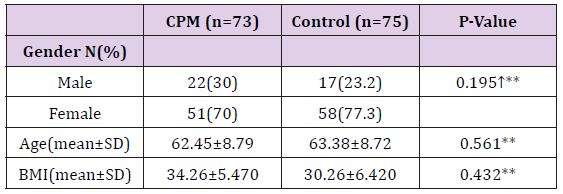
↑Chi square applied
Independent t-test applied
*P-value ≤0.05 considered as Significant
**p-value >0.05, Not Significant at 0.05 Levels
Table 2: Assessment 2 weeks pre operatively.

Independent t-test applied
*P-value ≤0.05 considered as Significant
**p-value >0.05,Not Significant at 0.05 Levels
Table 3: Assessment 7 Days Post Operatively.
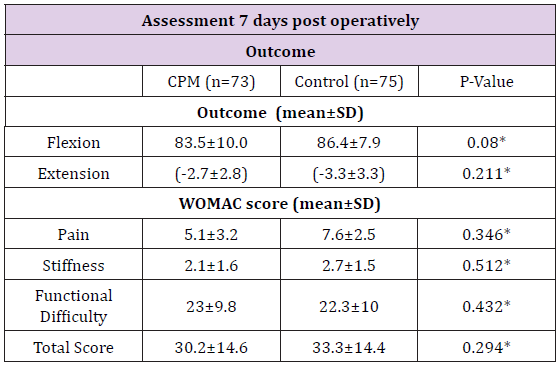
Independent t-test applied
*P-value ≤0.05 considered as Significant
**p-value >0.05,Not Significant at 0.05 Levels
CPM use in post acute rehabilitation, such as within homecare services or in an inpatient rehabilitation facility setting, does not appear to offer long term benefits following unilateral TKR, regardless of initial range of motion [16-18]. Our study further explored its use by applying it to only patients with active maximum knee flexion range of motion between 45°-75° which identified patients most at risk for stiffness. The findings confirm that in patients with poor initial range of motion, CPM use offers no added benefit to discharge range of motion values when compared to conventional physical therapy alone. The CPM intervention of this study may have been applied beyond the time period where passive knee range of motion to reduce stiffness will yield benefit [19]. Another explanation may lie in the nature of post acute rehabilitation where active participation in therapy is the hallmark of its services.
Simple functional activities such as rising from a low chair may introduce a greater degree of knee flexion than the CPM facilitating a greater degree of functional independence during the post acute rehabilitation phase. Since preoperative factors play a major part in determining post operative range of motion, identifying these factors would enable specific and focused use of physical therapy resources. A study following over TKA patients identified the most important factors impacting post operative knee range of motion [20]. The diagnosis of osteoarthritis and pre-operative knee flexion less than 75 degrees were the best predictors of post-operative range of motion whereas the total knee prosthesis, sex, age and the diagnosis of rheumatoid arthritis were not [21].
Knowledge of patients pre-operative clinical findings may help to identify those patients most at risk for stiffness so that effective early interventions can be promoted. CPM as a component of the physical therapy program in acute care hospitals is quite common. Its continued use in acute care hospital immediately following surgery is likely based the short term benefit it offers, especially when used with early flexion parameters [16,21,22].
Continuous Passive Motion does not provide an additional benefit over the conventional physical therapy interventions employed in an inpatient rehabilitation facility for patient following TKA, more specifically in patients had poor initial knee range of motion specially flexion following surgery, perhaps it increases the financial burden to the patients. So we concluded that Conventional physical therapy alone could be the convenient and sufficient method for rehabilitation in early post operative TKA patients. As it was a single centre prospective study with small sample size; therefore the results of the present study should be exercised with caution.


