Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
Asad Khan Ghilzai1, Syed Kamran Ali Shah*2, Muhammad Ayub Khan3, Muhammad Arsalan Ghazi2 and Muhammad Kazim Rahim Najjad1
Received: December 29, 2017; Published: January 09, 2018
Corresponding author: Dr Syed Kamran Ali Shah, Department of Orthopaedics, K-Block, Liaquat, National Hospital, Stadium road, Karachi
DOI: 10.26717/BJSTR.2018.02.000645
Objective: To evaluate the functional outcome of unstable Intertrochanteric fractures treated with proximal femoral nail while using Harris hip score.
Materials and Methods: This is a prospective observational study conducted at Orthopaedic Surgery Department. Total 91 patients of either gender with age between 18 to 70 years had closed AO type 31A2 and 31A3 unstable Intertorchanteric fractures of proximal femur and for ease labelled as type I and type II subsequently. All patients were operated with proximal Femoral Nail, using a standard prescribed surgical technique. After 3 months of surgery, patient was called for follow up and asked to answer the Harris hip score questionnaire. Effect modifiers were controlled by stratification using chi square test and p-value ≤0.05 was considered as significant.
Result: Total 91 patients were enrolled, 59 male and 32 were female. The mean age was 47.66±13.40 years, with range of 50(20-70) years. 32(35.2%) patients were aged ≤45 years and 59(64.8%) patients were aged >45 years. 46.2% patients had type-I fracture and 53.8% had type-II fracture. Excellent outcome observed in 28.6% patients, good in 45.1%, fair outcome in 16.5% and only 9.9% expressed poor outcome among 91 patients. No significant association of functional outcome observed with respect to gender (p=0.289), age (p=0.127), type of fracture (p=513), and mode of admission (p=0.662).
Conclusion: Proximal Femoral Nailing is one of safe and better ways of treating unstable intertrochanteric fractures to achieve significantly better outcomes with early rehabilitation as its advantages of being inserted through small exposure, preservation of hematoma and less blood loss. Hence, we observed in our study the Proximal Femoral Nail may be the better fixation implant for unstable intertrochanteric fractures.
Keywords: Unstable Intertrochanteric Fractures; Proximal Femoral Nail; Harris Hip Score
Abbreviations: IT: Intertrochanteric; PFN: Proximal Femoral Nail; PFNA: Proximal Femoral Nail Anti rotation
Intertrochanteric (IT) fractures are disabling injuries that most commonly affect the elderly population and also in young. The incidence has increased significantly during recent years due to the advancing age of the world’s population [1]. The incidence of intertrochanteric fracture is rising because of increasing number of senior citizens with osteoporosis. By 2040 the incidence is estimated to be doubled. In India the figures may be much more [2]. Problems of these fractures are association with substantial morbidity and mortality, malunion, implant failure, cut-out of head, and penetration into hip with great financial burden to the family [2]. Inherently Intertrochanteric fractures composed of anatomically different patterns that vary in their degree of stability following open reduction and internal fixation [3]. The unstable variety constitutes one half of the fracture as described by Evans intertrochanteric fractures classification [4].
With the passage of time and experience has repeatedly emphasized itself that such unstable variety of fractures are not treatable by the standard sliding hip screw used frequently for the stable types [5,6]. In elderly population trochanteric fractures represent a major health risk, although a large number of different implants are available for fixation, the ideal implant for treatment of peritrochanteric fractures is still a matter for discussion. The imperative goals of treatment can be achieved by early mobilization and stable fixation with minimally invasive procedure as possible. Several fixation devices have been developed to overcome the difficulties encountered in the treatment of unstable trochanteric femoral fractures. Recently intramedullary fixations devices have become increasingly popular because of its biomechanical advantage, and high rates of failure are debatable in fractures which were treated with sliding hip-screw system device. One implant of such type is the proximal femoral nail (PFN) was developed by the AO/ASIF in 1996 [7], it is commonly used now internationally [8] as well as nationally [9].
Interrochanteric fractures are very frequently faced by orthopaedic surgeons worldwide [10,11]. Increase in the incidence of these fractures are seen 5th decade of life onwards [11,12]. Age of patient, osteoporosis, general health, associated co morbidities are some of the key factors to be considered for the successful treatment of these fractures [11,13]. There for surgical treatment is preferred option of treatment as it facilitates early mobilization & functional recovery [11-17]. But single screw construct was considered unstable for trochanteric fractures which led to introduction of proximal femoral nail in 1997 by AO/ASIF which has provision of two screw placement in the femoral head. This system of Antirotation screw & cervical load bearing screw in this nail makes this construct biomechanically very stable [11,13,17,18].
The main principle of this type of fixation is based on a sliding screw in the femoral neck-head fragment, attached to an intramedullary nail. Despite being technically difficult to perform, these implants are gaining wide acceptance in treating unstable intertrochanteric fractures because of its advantages of being inserted through small exposure, preservation of hematoma and less blood loss [19,20]. Uzun M et al. [21] evaluated radiographic complications occurring after treatment of unstable intertrochanteric hip fractures with the Proximal Femoral Nail (PFN) and their effect on functional results on 35 patients. The Harris hip score results were excellent in 11 patients (31.4%), good in 15 patients (42.9%), and fair in seven patients (20%). Ye PH et al. [22] investigated the clinical results of the proximal femoral nail antirotation (PFNA) system in the treatment of unstable intertrochanteric femoral fractures in 90 patients. The mean Harris hip score was (80.5 +/- 9.8). According to Harris hip scores evaluation system, 26 patients (28%) reached an excellent result, 37 good (41%), 18 poor (20%).
Sahin S et al. [23] conducted a study Radiographic and functional results of osteosynthesis using the proximal femoral nail antirotation (PFNA) in the treatment of unstable intertrochanteric femoral fractures in 45 patients. The mean Harris hip score was 77.8. Harris hip scores were very good in 11 patients (24.4%), good in 19 patients (42.2%), moderate in nine patients (20%), and poor in six patients (13.3%). Aim of our study is to evaluate the functional outcome of Proximal Femoral Nail in patients with unstable intertrochanteric fractures. Number of studies has been published nationally and internationally in literature on treatment of these fractures with a dynamic hip screw, but not much has been published on fixation with proximal femoral nail. This study will provide a baseline data and if the results are acceptable it may help to change operative treatment of unstable intertrochanteric femur fractures.
This was a prospective observational study conducted at the Department of Orthopaedic Surgery, Liaquat National Hospital and Medical College, Karachi. March 2015 to Feb 2016. Patients were registered using a predesigned Performa. Approval from institutional ethical review committee was taken prior to commencement of the study. Formal informed written consent was obtained from patients registering in the study. Using a nonprobability, consecutive sampling technique 91 patients were registered for the study.
i. Patients aged between 18 yrs and 70yrs
ii. Patients of either sex
iii. Patients with closed fractures
iv. Patients admitted through Accident and Emergency or Outpatients Department with AO type 31A2(type I) and 31A3(type II) intertorchanteric fractures of femur (diagnosed by X rays)
v. Patients fit to undergo surgical procedure
i. Patients with cognitive disorders not able to communicate effectively
ii. Pathological fracture
iii. Open fracture
iv. Any other associated injury
After meeting the inclusion and exclusion criteria, patients were included in the study. Physical and radiological examination was done by principal investigator. All patients were operated using a standard prescribed surgical technique by the experienced surgeon (having greater than 5 yrs experience). Patients have a follow up protocol at 2nd, 6th, and 12th week after operations. After 3 months of surgery, patient was called for follow up and asked to answer the Harris hip score questionnaire. Harris hip score was collected using a pre-designed Performa by the principal investigator. Confounding variables as well as bias was controlled by strictly following the exclusion criteria. Data were entered and analyzed through Statistical Package for Social Sciences (V-17).
Mean and standard deviation were computed for the quantitative variable i.e., age. Frequency and percentage were calculated for qualitative variables like gender, mode of admission, type of fracture, and functional outcome (Excellent to poor). Effect modifiers were controlled by stratification of age, gender, type of fracture and mode of admission to observe the effect of these modifiers on outcome by using chi square test and p value≤0.05 was considered significant.
Total 91 patients of either gender with age 18 to 70 years admitted through emergency department with closed fracture of AO type 31A2 (type I) and 31A3 (type II) were evaluated to determine the functional outcome of unstable intertrochanteric fractures treated with proximal femoral nail using Harris hip score. Descriptive statistics was calculated. Mean ± SD were calculated for quantitative variables. Frequency and percentages were calculated for qualitative variables. Stratification was done and post stratification chi square test was used. P-value ≤0.05 was considered as significant. The results showed that there were 59 (64.8%) male and 32 (35.2%) female patients with mean age were 47.66±13.40 years, with range of 50(20-70) years. Age is stratified in two groups and according to stratified groups, 32(35.2%) patients were aged ≤45 years and 59(64.8%) patients were aged >45 years.
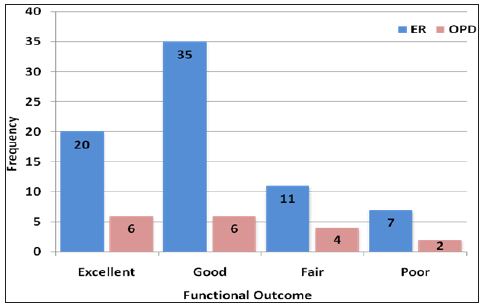
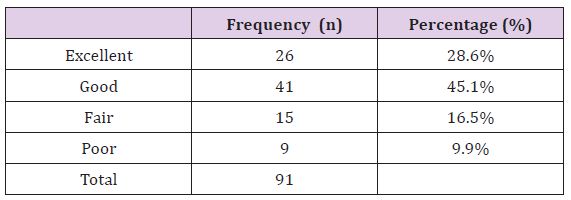
Mean age of patients aged ≤45 years was 31.97±9.26 years and for patients aged >45 years the mean age was 56.17±4.83 years. The results showed that 46.2% patients had AO type 31A2 (type-I) fracture according to AO classification and 53.8% had AO type 31A3 (type-II) fracture according to the same classification. It was observed that 73 (80.2%) patients were admitted through Emergency department and 18 (19.8%) patients were admitted throughout patients department. The functional outcome was observed and results showed that excellent outcome was found in 26 (28.6%) patients, good outcome was found in 41 (45.1%) patients, fair outcome was found in 15 (16.5%) patients, and poor outcome was found in 9 (9.9%) patients (Figures 1-5).
Figure 1: Frequency of functional outcome according to gender (n=91).
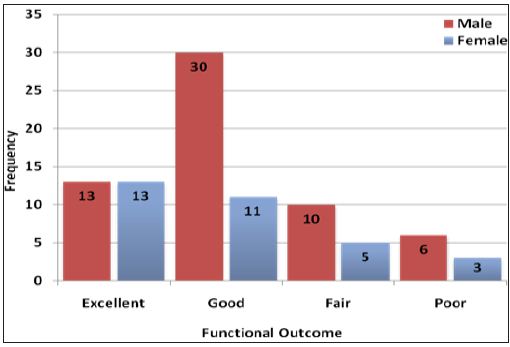
Figure 2: Histogram presenting distribution of age in years (n=91).
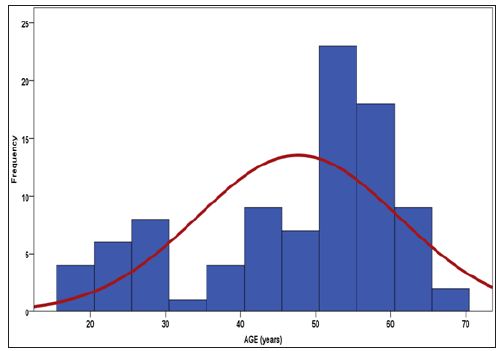
Figure 3: Frequency of functional outcome according to age groups (n=91).
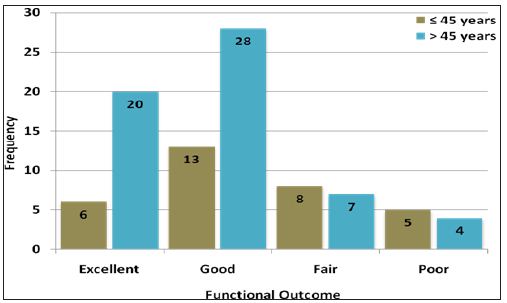
Figure 4: Frequency of functional outcome according to type of fracture (n=91)
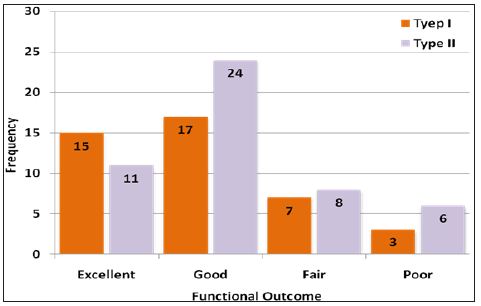
Figure 5: Frequency of functional outcome according to mode of admission (n=91).
The Harris hip score was observed according to outcome. Among patients with excellent outcome the mean Harris hip score was 95.77±3.15 and in patients with good outcome the mean score was 85.29±2.90, similarly among patients with fair outcome the mean Harris hip score was 75.53±2.80 and in patients with poor outcome the mean score was 65.44±2.45. The stratification was done on gender, age, type of fracture and mode of admission. Chi square test was applied considered p-value≤0.05 as significant (Table 1).
Table 1: Frequency Distribution of Functional Outcome (n=91).
Results showed no significant association of functional outcome was observed with gender (p=0.289), age (p=0.127), type of fracture (p=513), and mode of admission (p=0.662) as p value found statistically insignificant.
Proximal femoral nail is an intramedullary device and has all advantages of intramedullary biomechanics, such as decreasing the moment arm, can be performed by closed technique, which preserve the fracture haematoma and it’s an important consideration in fracture healing, it also decrease blood loss, infection risk, minimizes soft tissue dissection and wound related complications [24]. The Proximal Femoral Nail (PFN) System offers some major biomechanical innovations [25]. Axial loading in A1 and A2 fractures leads to fracture impaction, whereas in A3 fractures such impaction doesn’t occur, and medial displacement of the distal fragment of the fracture is common due to the instability. Proximal Femoral Nail for A3 type unstable fracture has superior results; PFN has been shown to prevent the fractures of the femoral shaft by having a smaller distal shaft diameter which reduces stress concentration at the tip [26].
Due to its position close to the weight-bearing axis the stress generated on the intramedullary implants is negligible. The PFN implant also acts as a buttress in preventing the mediatisation of the shaft. The entry portal of the PFN through the trochanter limits the surgical insult to the tendinous hip abductor musculature, only unlike those nails which require entry through the pyriformis fossa [27,28]. The stabilising and the compression screws of the PFN adequately compress the fracture, leaving between them a bone block for further revision should the need arise [26]. Domingo et al. [29] conducted a study on 295 patients for intertrochanteric fracture fixation with PFN and obtained overall results were comparable with those of other frac¬ture systems, authors assert that technically surgery is not complex and numbers of recoded complications were acceptable. The intraoperative variables and the systemic complications were similar to those encoun¬tered by other devices [30,31].
At present, PFN is an acceptable and minimally invasive implant for unstable proximal femoral fractures. Quality of life and function are usually measures that are important for patients and health care provid¬ers [25]. There is ability to perform activities of daily routine like walking, squatting, cross leg sitting, climbing stairs was acceptable in patients of intertrochanteric fracture fixation with PFN [18]. A comparable study was carried out on total of 39 patients for unstable intertrochanteric fractures (AO/OTA 31-A3) were treated with PFN and 95° screw-plate with one year follow up. Result reported that patients treated with PFN had shorter operative times, fewer blood transfusions, and shorter hospital stays compared with those treated with a 95° screw-plate. Also noticed seven of the 19 patients who had been treated with the 95° screw-plate experienced implant failure and/or non union but in comparison to this only one fracture out of 20 treated with PFN underwent non union [19].
Poor reduction, malrotation or wrong choice of screws results in technically failures of PFN. An intraoperative fracture displacement during manual insertion of the nail into the femoral shaft may be a problem with the PFN, as the entry point of the PFN at the tip of the greater trochanter is located directly in the fracture region which can cause an intra operative fracture displacement [31]. The use of the PFN has become an attractive option now as locally manufactured implant and instruments are available in Pakistan. Because of excellent experience with femoral and tibial inter-lock nailing and our increasing expertise in the technique, we have used the new method of nailing more and more frequently during the last few years. Immediate stability and early bony union vindicated the overall efficacy of the close nailing technique and is in line with another study by Anglen et al. [32] Immediate stability had the concomitant advantage of restoration of full function of the extremity. This was demonstrated by the fact that 68% of our patients achieved prefracture mobility in the injured limb within six months. This is in line with other studies of the proximal femoral nail and Gamma nail, which reported a restoration of mobility in 40% to 70% of patients [33].
It would seem that the improvement in mobility can be attributed to improved restoration of hip anatomy and biomechanics achieved by this new implant. Studies comparing the DHS with the PFN also found that patients who received a nail were 50% more mobile than those with a DHS, which had best results before AO/Asif PFN [9]. Our findings regarding mobility are in line with these studies. At present, we consider that the PFN is a good minimally invasive implant when closed reduction is possible. The modification of the PFN and careful surgical technique should reduce the high complication rate in our study.
From our experience with the Proximal Femoral Nail, it was observed that although the method is technically demanding and requires special instrumentation, but the advantage of immediate stability in difficult and unstable fractures, and the relatively few complications serve to recommend it for the method of choice for surgical treatment of unstable intertrochanteric femoral fractures. The intramedullary nail provided significantly lower rates of implant failure and delayed healing, thereby lessening the need for revision surgery. We conclude that in unstable intertrochanteric fractures the PFN has significantly better outcomes in terms of earlier restoration of walking ability as its advantages of being inserted through small exposure, preservation of hematoma and less blood loss. In our opinion, PFN may be the better fixation device for most intertrochanteric fracture.


