Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
Mmule M Magama1, and Mabedi Kgositau2
Received: December 20, 2017; Published: January 09, 2018
Corresponding author: Mmule M. Magama, Assistant Director, Centre for Academic Development, University of Botswana, Botswana, Africa
DOI: 10.26717/BJSTR.2018.02.000643
Background: The study examined the nature of stress among nurses working in Gaborone City Council clinics. The aim of the study was to investigate the nature of stress affecting nurses with a particular attention to nurses understanding of stress, contributing factors, their experiences, coping mechanisms, as well as suggestions on measures they use to minimize stress.
Methods: An Occupational Stress Indicator (OSI) was used as a framework to guide the study. A combined paradigm approach in which a semi structured questionnaire and focus group were used to collect data. None probability technique using conveniently selected sample was employed to identify research participants [1].
Findings: The findings revealed that 90% of nurses have an adequate knowledge about stress, that nurses experience tremendous stress and most have already developed signs and symptoms of stress. Major stressors in the nursing environment were found to be poor conditions of service, in particular poor management styles, lack of resources and supplies such as equipment and drugs. Forty three percent (43%) cited blood pressure machines, weighing scales and furniture as old, poorly maintained and inadequate. Nurses used various strategies to deal with stress; included in the list were smoking, dysfunctional behaviours such as aggression, anger and irritability.
Conclusion: It is apparent that nurses are mostly stressed by poor working conditions related to lack of resources, heavy workload and poor management styles. Though the study cannot be applied to all nurses in Botswana, it is adequate to represent nurses who offer primary health care in the clinics and outpatient settings. Researcher recommended a national study that would be highly representative, more exploration about the extent and the nature of smoking amongst nurses; the need to improve work conditions and to develop counselling programs for nurses.
Nursing is by nature perceived to be a stressful job; Menzies, 1959 was the first author who confirmed that, caring environment arouses strong emotions such as pity, anger, resentment & compassion. The author affirmed that Nurses use defense mechanisms such as avoidance, denial, substance abuse, and this was evidenced by increased turnover. It is possible that in today’s world, nursing may be generating unbearable stress related to emotional trauma, change in patients’ life styles, change in disease patterns, and the increasing violence and abuse. Desire to conduct the study was stimulated by an increasing numerous public complaints that was consistently covered by the media and discussed in political field. The purpose the study was to examine the nature of stress among Nurses working in the primary health care clinics. The study is significant to health care providers and policy makers who are encouraged to acknowledge stress in nursing and how it impacts on nurses. In this way, managers and policy makers could be in a position to be aware of stress and develop programs for managing stress at work for the welfare of nurses. The study addressed questions related to nurses’ understanding of a concept of stress and factors that contribute to stress in the nursing profession. Further exploration was on the signs and symptoms that nurses’ experience when stressed, their coping mechanisms and how they can be assisted to deal with stress at work.
An Occupational Stress Indicator (OSI) Model was used as a guiding framework for the study; sections of the model used were:.
a) Knowledge about stress,
b) Perceived stressors
c) Effects of stress and
d) Coping strategies
However, it is necessary to acknowledge that OSI scale does not look at other stress contributing stress such as personal believe system and personality traits. According to a student essay “is not intended to assess or question personality or to test the personal attributes of the individual, but instead, to provide an indication of how one perceives their working environment and how a number of variables interact to produce potentially stressful effects for the individual’’ (2017) https://www.ukessays.com/essays/ employment/occupational-stress-indicator.php [1].
Mixed method (qualitative and quantitative) approaches were used to conduct the study; quantitative approach being more dominant. Ethical clearance was accorded by the Ministry of Health Research Unit and clinic authority to have access to nurses was granted by the senior nursing supervisors of various clinics. Confidentiality was assured and participation was voluntary. A previously used Chartered Society of Physiotherapy questionnaire was adopted with minor modifications; the tool reflected contents of the OSI model. A self-developed interview guide was developed to guide a focus group discussion for collecting qualitative data. The questionnaire was piloted on 5 nurse practitioner students who had worked for over a period of a year in local clinics in which data was collected. The results for a pilot test were not included in the main result analysis. A convenient sample of 53 nurses was drawn from 7 out of 15 clinics which were randomly selected; the sample only included nurses who were found on duty during data collection period, nurses who were off duty were excluded. All respondents were nurses of different levels and specialties. It is important to note that these respondents had experience of working in both rural and urban areas; hence, their views included experiences reflected views from both areas. Quantitative data were coded using epidemiological information which was transferred as raw data into the Statistical Package for Social Sciences (SPSS) and qualitative data were analyzed thematically to examine emerging themes [2].
Data were collected from one of the major cities in the Southern part of Botswana which has a population of 208.441 people (World pop., Prospects, 2017). According to one of the nursing supervisors, the city has 382 nurses. There are 15 clinics out of which 3 has a maternity unit, and 4 provide a 24 hour service. Each busy clinic was allocated 9 nurses, 3 of which were midwives while the less busy were allocated 7 to 8 nurses.
The results revealed that, over 80% of the respondents were able to define stress; respondents defined stress as:
a) Accumulation of unresolved grievances manifested by physical symptoms, and
b) Internal and external force perceived to be threatening,
c) Emotional state of despair aggravated by strenuous work which may result in mental and physical disorders.
The prominent concepts from the definitions were: psycho social factors, psycho somatic syndrome, tension, disappointment, inability to adapt, inability to cope, strain and stressors. Workload was said to be unbearable with multiple responsibilities and this forced respondents to perform duties outside the scope of the nursing practice. According to respondents, high workload resulted in long queues which made patients disgruntled; harassment, belittlement and abusive language directed to nurses were a common trend. Despite the rough conditions that prevailed, respondents revealed that management is more skewed to protection of patients and not professionals. Management and leadership were reported to be poor, dominated by failure to discuss issues and inability to carry out supervisory visits. One respondent cited that the “senior staff is autocratic, never listen, jealous and never involve juniors in decision making” Transfers were reported to be unfair and dominated by bribery and favors; while some nurses circulated in towns, some were bound to rural areas. This state of affairs makes it difficult for respondents to decide on life choices such as choosing marriage partners, education of children, acquiring property and selfdevelopment. One respondent said: This has resulted in the increase in the rate of marriage and intimate relationships between nurses and drivers, watchmen and herdsmen, because there is no one else in the rural areas except nurses and the animals.
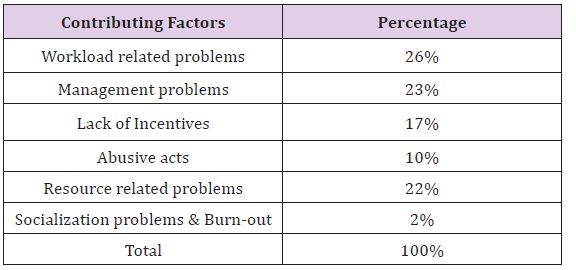
Among the top reported environmental factors that contributed to stress were that, the facilities were too hot or too cold and noisy; unsafe, poor, and uncomfortable; there were no resting places and the lighting was bad. The following Table 1 outlines respondents’ views in regard to what they perceived as stressors in their profession. Other work place factors that scored high were lack of environmental risk assessment (96%), failure to control hazards (66%) and repetitive work (55%). Excess workload (11%) and increased working hours (38%), boring work (34%), lack of training (17%), harassment (38%), threat and violence (32%) were cited as some of the stressors. In an attempt to elaborate on stressors respondents’ faced in the workplace, one respondent said: I have so many frustrations; the work is boring and I am expected to do some duties without any training,” while the other respondent cited that the “workload is too much; we attend 60-75 patients per day against the stipulated rate of 30 patients per nurse per day” All respondents agreed that equipment used in clinics is old, unreliable, inadequate and never replaced. Forty three percent (43%) reported shortages of equipment such as blood pressure machines, weighing scales, furniture, wheel chairs and oxygen apparatus affirming that some of these are faulty, old, rusty and unsafe. Buildings and others structures were said to be worn out and while some were almost falling.
Table 1: Factors Contributing to Stress.
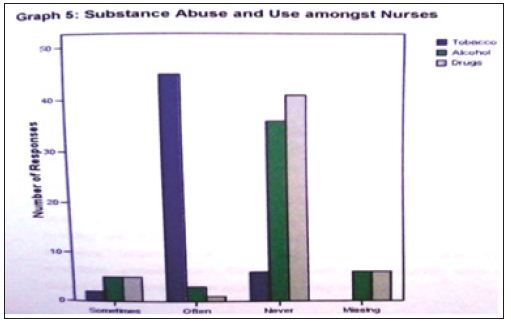
In response to a question exploring if respondents suffer stress related symptoms; a wide variety of symptoms such as confusion, fatigue, exhaustion, headaches, anxiety, depression and palpitations and many other symptoms were mentioned and irritability scored high (73%). One respondent said “I normally experience tension headache which I normally take treatment for and gastric ulcers which I am also taking treatment for.” One respondent disclosed that: ‘sometimes I feel like going away where nobody would find or trace me and sometimes I feel like resigning.” Exploring how respondents cope with stress and stressors; most respondents use various strategies ranging from rest, prayer, sleep, talking with someone, exercises, television, novels, crying, taking sleep tablets, and self-reward (new clothes, doing facials & visiting relatives). In regard to what respondents do to clients, themselves and or management when experiencing stress, respondents revealed symptoms of irritability. One respondent said “I become angry at clients, and consult them quickly so that they can get out of my sight,” while the other one she “i ignore management or tell them that what they are doing is wrong.” Another respondent said “I develop selfblame on why I took nursing as my profession” On enquiring use of substance as a means to reduce stress or overcoming symptoms experienced, results revealed low substance use or abuse; 10% sometimes use drugs or alcohol. However, over 80% of respondents admitted frequent smoking to cope with stress. Refer to the graph below for details of responses (Figure 1).
Figure 1:
Respondents recommended a series of strategies to assist them in coping with work related stress; that development of welfare policies for nurses, emphasizing that policies should cover transfers and accommodation, appreciation of work that nurses do and development of safety measures such as making police part of staffing of health facilities.
According to results, respondents understand the meaning of stress; however, different respondents explained the meaning differently (Hardy & Carson, 1998). Respondents’ view of stress and job stressors is different and they respond differently to stressful stimuli. Respondents seem to associate stress with extrinsic factors such as workload, management styles and environmental factors etc. These findings are similar to other studies on stress on health care providers [3-5]. Intrinsic factors such as professional socialization personality traits and spiritual health status were not considered as having a relationship with stress that respondents had. Bangkok Charter of 2005 for the Health Promotion in a Globalized world endorsed determinants of health as encompassing not only physical and mental health, but also the spiritual well-being. This may be a limitation of knowledge in which respondents could not relate personality traits, professional socialization and spiritual health status as determinants of the level of stress that nurses may develop. It is evident that nurses experience tremendous stress at work, coupled with personal issues, the situation may be worse. According to findings by Chartered Society of Physiotherapy (2004) employment relations and Union services, “stress at work is not an illness, but if it is excessive and prolonged, it can lead to mental and physical ill health, including depression, nervous breakdown and heart disease”.
Major stressors for respondents were associated with workload, limited resources and supplies, poor management, lack of incentives and security. There seem to be a relationship between respondents’ disgruntlement and the stress experienced; hence, it may be possible that dealing with the root cause of stress would motivate nurses to improve service delivery and the relationship with communities at large. Dealing with resources and supplies will not only satisfy nurses, but, but also improve quality of services; it will enhance accuracy of results and client diagnosis and reduce medical errors [5-8].
Since respondents consider external forces as responsible for stress, counseling strategies were not viewed as measures that could alleviate stress; how-ever, various strategies such as development of welfare programs and development of welfare policies that provide support to nurses and the nursing profession would be beneficial. Though evidence of stress has been identified; there was no prove that stress experienced by respondents is directly work related and the pathological and mental impact of stress among these respondents could not be determined because other sources of stress were not explored and the respondents were not medically examined to confirm the impact of stress on their well-being. Respondents seem to be well educated in regard to drug use and abuse because majority was not engaged in substance use and or abuse. However, it would be interesting to explore more about smoking in order to determine the nature of smoking and its impact on respondents’ health. Generally, recommendations for improvement should focus on improving administrative procedures, management skills for supervisors, and conditions of work and to regularly provide training opportunities. Due to a small sample size and the nature of sampling, the study may not be generalized to all nurses in Botswana; however, it is adequate to generalize the study to nurses working in the major cities of Botswana; the study can serve as a clue to what could be happening in the Botswana Health care system. Future research should explore other factors that may be responsible for stress in the nursing profession using theoretical models such as Pressure Management Indicator (PMI) which are more holistic in nature. According to Williams & Cooper, 1996. PMI is reliable, comprehensive and quick to complete than the OSI Model. It considers a wider spectrum of sources of stress and these include a) individual health, personality (behavior, attitude and ambition) as well as locus of control.


