Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
Marcelo Pinto*,Gustavo Gaffrée, Roberto Santos and Fábio Ramoa, Jonathan Paixão, Hugo Melo and Célia Archer Ramoa
Received: December 08, 2017; Published: December 13, 2017
Corresponding author: Marcelo Pinto
DOI: 10.26717/BJSTR.2017.01.000587
The mandibular hyperparathyroid brown tumour is considered a rare metabolic disorder, also known as mandibular osteoclastome, therefore its therapy is not well defined yet; This lesion is triggered by the excess of the production of PTH parathyroid hormone, which are directly linked to mechanisms of control of levels of calcium, phosphorus and vitamin D, which confers the lesions the aspect of numerous osteoclastic cells, circumscribed and richly vascularised Which causes their reddish-brown coloration, individuals affected by this disorder show signs and symptoms of weakness, nausea, fatigue, anorexia, excessive thirst, polyuria, constipation and consequently depression, the purpose of this study is to perform a literature review by describing the case of mandibular brown tumour, explaining the conduct performed according to the case by clinical, laboratory analysis and image studies that guided the case.
This disorder, called brown tumour, has its determinant a metabolic bone disarray caused by the excess production of parathyroid hormone, which is produced by the four parathyroid glands located posterior to the thyroid gland, which are responsible for the control of phosphorus (P), calcium (Ca) and vitamin D; The level of calcium present in the blood is considered a triggering factor of the disorder by the release and production of this hormone. Shetty “the hyperparatiroidism HPT is a disease in which there may be a complex, of biochemical anatomic and clinical abnormalities”. Therefore the Brown Tumor has its histopathological complexity described as multiple adenomas, numerous osteoclastic cells, of cystic format, and separated by a highly vascularized tissue which will confer the lesion a dark red or brownish coloration which characterizes its nickname. Some of the signs and symptoms observed in this disorder are fatigue, nausea, weakness, anorexia, excessive thirst, polyuria, constipation, pain, swelling and frequent urination. In severe cases, may present kidney stones, loss of bone mass and fractures, mental confusion and consequent depression.
The systemic scenario begins when the body presents in hypocalcemia, and in the other hand will be inhibited in hyperalcemia, it will be stimulated the uptake of calcium to the extracellular environment, which leads to the increase of serum calcium concentration and decrease of the phosphate ion which is responsible to transport the phosphorous. Two sites of action in bone metabolic disorder are recognized, which are described respectively as actions on kidneys that reduce phosphate absorption and increase calcium absorption and the action on bones that stimulates bone mobilization with increased serum calcium concentration. Another important aspect and the issue of vitamin D which is a regulator of osteo mineral calcium physiology, vitamin D is used in the treatment of the secondary form of the disorder as supplementation. The disorder may be divided into primary, where the treatment will be surgical removing the lesion, and secondary where the basic disorder that will affect the normal functioning of the parathyroid glands and vitamin D supplementation should be treated.
Brown tumor of Hyperparathyroidism it is a metabolic disorder that can affect the entire skeleton. This disorder is named due to macroscopic aspect to the intraossic lesions, presenting reddishbrownish hue, due to the intense bleeding that occurs in these lesions and the deposit of hemosiderin. Commonly, this disorder is a result of a framework of primary hyperparathyroidism, secondary rarely and tertiary. Brown tumor arises only in chronic cases of non treated Hyperparathyroidism (PTH). The lesions are caused by the increased production and release of PTH, leading to increased re absorption of calcium in bones. With the constant calcium sequestration l, it will start to grow a repair tissue, which increases gradually in size [1,2]. This disorder usually rise in individuals who are in third, fourth and sixth decade of life, especially in females. The most affected is in the head and neck area especially in mandibular area [1,2]. Clinical manifestations vary according to the location and extent of the Tumour. In the mandibular bone, there may be pain and hard tumefaction. When extensive it can lead to deformation of the region, impairing the function of the bone [1,2].
HT’s symptoms are observed including fatigue, weakness, nausea, anorexia, excessive thirst, polyuria, constipation and depression [1,2]. The diagnosis are achieved through radiological exams, computerized tomography scans and Histopathological examination of the Tumour. Histopathologically the Brown Tumor is characterized by a soft tissue mass composed of giant cells inside of a fibro vascularstrome, like cystic spaces have queued for connective tissues. The focus of hemorrhage and hemosiderin deposition appears as a reliable reddish-brown mass, a characteristic that gave rise to your name [3,4]. It resembles, yet histopathologically to other inside giant cells, as the central giant cell lesion and cherubism. It is important to analyze the history of the disease and assessment and laboratory tests for determination of definitive diagnosis. The identification of the lesion, through laboratory findings (Hyperparathyroidism) rule out the existence of central giant cell lesion, featuring, in its way the presence of Brown Tumour [4]. Radiographically, the Brown Tumor is characterized as a lytic lesion, expansive, well defined, involves the bone cortical and may present a fine mesh of intralesional steroid septa, which gives the condition a multi side appearance, and may also be uniside.
The Brown Tumour generally shows multiple occurrences, although it can also occur as a single one. When present in the mandibular bone, it usually appears at the hard blade [5,6]. In addition one could observe bone trabeculae neo formed with osteoblasts tumefactions on its edges. Blood tests indicate the increased levels of calcium and alkaline phosphates, as well as the reduction in the level of phosphorus is useful for finding the correct diagnosis [1,2]. The Brown Tumor does not demand specific treatment in most cases because the correction of Hyperparathyroidism leads to the lesion disappearement. However, it can cause pathological fractures and bone marrow compression even when it involves the spine. When it reaches the face can cause breathing difficulties and facial deformities. In such cases, it is recommended that the patient undergoes surgical treatment [7-9].
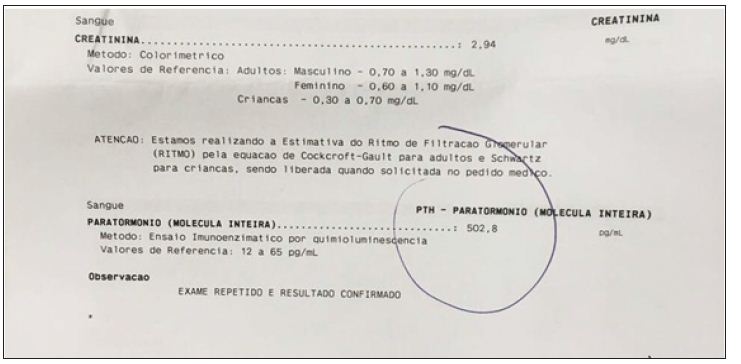
According to radiographs and Tomography scans: it shows a radiolucent / hypodense diffuse, irregular image without bulging of the vestibular and / or lingual bone cortices was verified. Radiographic and CT scans did not show radiopaque halus, that is, descorticalized, involving the region of the element 36. Bone resurfacing in the furcation region in the same element. In computed tomography (CT), the medullary bone presents a granular aspect with bone and lingual cortical thinning, vertical bone loss located in the mesial and distal part of the 36 element, and increased ligament space with absence of hard lamina, apparent mobility, initial external root resorption in the Element mentioned above. Hypothesis: Bone tumor, endo-periodontal envelopment or giant cell lesion. According to the laboratory test of Parathyroid hormone (PTH), by the enzyme immunoassay method by chemiluminescence with a result of 502.8 pg/ml (normal 12 to 65 pg/ ml), creatinine level is high with 2.94 mg/dl (Normal for male patients is 0.70 to 1.30 mg/dl). Histopathological examination by Hematoxylin and Eosin staining method with diagnosis of Brown Tumour (osteoblast matrix with prominent osteoblasts and osteoclasts, amidst fibrous stromal fibroblastic proliferation: proliferated, ecstatic and congestive vessels, haemorrhage and hemostasis).
The parathyroid glands were increased in cervical ecography. The findings of hyperparathyroidism were confirmed together with other exams to the diagnosis of Brown Tumour of Hyperparathyroidism. Patient was submitted to surgical intervention under general anaesthesia, naso-tracheal intubation, vestibule access in the region of the left jaw body, enucleation of the lesion, removal of the element 36, curettage and synthesis of the region. All material was collected and sent to the pathology center of the State University of Rio de Janeiro (UERJ) for histopathological analysis where the diagnosis of Brown Tumour of Hyperparathyroidism was confirmed. Post surgery evolution of the patient in question was compatible with the surgical procedure and without intercurrences.
Patient male, 35 years W.L.M. R, Brazilian, born in Rio de Janeiro, attended the Oral clinic and traumatology maxillofacial surgery at Municipal Lourenço Jorge Hospital, Barra da Tijuca, capital of Rio de Janeiro. During the anamnesis reported as main complaint “volume increase in unilateral mandibular region being the left side, painful. Current history of the disease (HDA) with account of start approximately 2 (two) years, as a minor injury to the gums, which evolved gradually, resulting in lumps region mentioned above. Still reported that does not have habits like smoking and alcoholism, drug hyper sensibilities, morbid antecedents denies personal and family. Clinical and physical examination showed, increased mandibular unilateral left significant volume, pain and mobility the palpation of the 46 element associated with bulging Protuberance in the abovementioned causing bone, with absence of fungi signs and infectious in the oral cavity (Figure 1).
Figure 1: Clinical and physical examination of patient.

In the dental restorations, specific resin systems are applied to the damaged tooth area to form a cast restoration that is then heat-treated using special ovens under controlled laboratory conditions. The ideal temperature for heat treatment application depends on the thermal behavior of each composite, such as glass transition temperature (Tg) analysis and initial degradation temperature [7]. The Tg can successfully be used as a reference to sign the ideal heat treatment for photo-irradiated resin composites. Above Tg, the secondary molecular interactions are weakened and, as a consequence, material properties are optimized once trapped radicals are given the opportunity to react [8-9]. In addition, the maximum temperature for heating without damaging, i.e., initial degradation temperature, needs to be determined to avoid weight loss [10]. In the present investigation, Conventional TG-DTA is a powerful and convenient thermal analysis technique which allows various important physical and chemical transformations such as glass transition and degradations are examined (Figures 1-4). Glass transition temperature (Tg) and number of phase transitions are evaluated for different dental materials are shown in Table 1.
Anatomical assessment: Preoperatively, the median radial tilt was 29 degrees of dorsal angulation in the group and 32 in the Non Spanning Syringe Distractor group. Postoperatively, the median tilt was 8 degrees of volar angulation in the Hoffman II group and 2 degrees volar in the Non Spanning Syringe Distractor group (p = 0.002). At the time of removal of the fixators, there was still a statistically significant difference in radial tilt: 9 degrees of volar angulation in the Hoffman II group and 4 degrees in the. Non Spanning Syringe Distractor group (p= 0.04). At 1 year, the difference was no longer statistically significant. For the other anatomical variables, no statistically significant differences were found (Table 2).
Figure 2: Computed tomography scan.
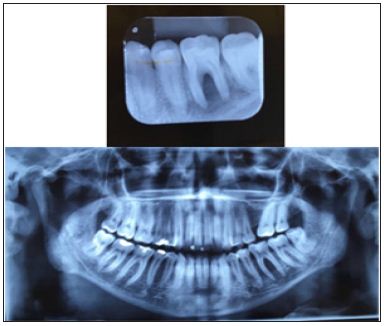
Figure 3: Diagnostic hypothesis: Bone tumor.
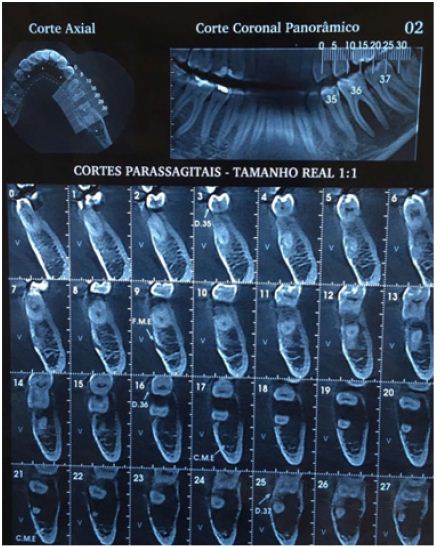
Figure 4: Diagnostic hypothesis: Endo-or giant cell lesion periodontal.

Figure 5: Result of presence of parathyroid harome, by the method of chemiluminescence enzyme Immuno assay.
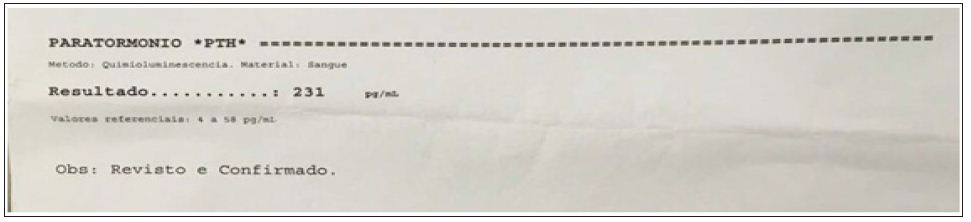
Figure 6: Brown Tumor diagnosis.
Histopathological examination, by coloring method by hematoxylin and eosin with Brown Tumor diagnosis (with prominent osteoid matrix osteoblasts and osteoclasts in fibrous stroma with fibroblastic proliferation: vases proliferated, entranced and congestion, pockets of deposition of hemosiderin and hemorrhage). Parathyroid glands were increased in cervical ultrasound. The findings of hyperparathyroidism confirmed together with the other tests the diagnosis of Hyperparathyroidism Brown Tumor (Figure 7). Patient underwent surgery under general anesthesia, naso-tracheal intubation, accomplished access in lobby Fund in the region of left mandibular body, enucleation of the lesion, dental extraction of 36 element, curettage and synthesis of the region. All material was collected and forwarded to the pathology Center of Rio de Janeiro State University (UERJ) for histopathological analysis where it was confirmed the diagnosis of Hyperparathyroidism Brown Tumor. Postoperative evolution of the patient in question was compatible with the surgical procedure and without complications (Figure 8).
Figure 7: Result of microscopic examination.

Figure 8: Patient underwent surgery under anesthesia.

The Brown tumour is a lesion associated with the hyperparathyroidism and can be divided into primary or secondary. Affects more the mandible than the maxilla and your prevalence is by the feminine gender above 50 years. We can clinically identify a Brown tumour of hyperparathyroidism because of an increase volume in the region causing pain and mobility, presenting as an extroverted mass of slow growth and destructive character. Depending on where the tumour is located, they can cause: diplopia, deformity, bleeding, chewing trauma, among other adversities. Radiographically, we identified this Brown tumour of hyperparathyroidism, due to the presence of a uni or multiocular radiolucent image, descorticalized, besides that when the Computed Tomography was performed, described in the above case, absence of the hard blade was revealed.
Histologically, the Brown tumour of hyperparathyroidism manifests as a mass of soft tissue composed of a giant cells inside the fibro vascular stroma, presenting focus of bleeding and hemosiderin deposition as a friable red-brown mass.
Diagnostic errors can occur if we only evaluate their histological characteristics, since other lesions such as the giant cell lesion present similar aspects to this lesion, thus causing unnecessary radical therapeutics and severe sequels if the diagnosis is incorrectly concluded. . Therefore, it is extremely important to analyze the history of the disease and laboratory tests. On laboratory examination, elevated creatinine level revealed parathyroid gland hyperplasia confirming the diagnosis, in addition with the other exams, of Brown tumour of hyperparathyroidism. The treatment accomplished in the relate of case was surgical with the objective was remove all the tumour and for this reason a naso-tracheal intubation was performed, with your purpose was allow a good surgical access, giving better tranquillity to the surgeons work, besides ensuring that the patient was treated in a single surgical time. Posteriorly, was done the enucleation of the tumour, which was the purpose of the surgery, the element 36 removal, curettage and suture of the region.
The literature review on the mechanism of pathological action of the brown tumour associated with a clinical case study, it was possible to reaffirm that dentistry is on the correct path both to diagnose the disorder through the diagnostic exams, establishment of differential diagnostic and laboratory exams as long as long-term treatment, not only through aspects closely related to the dental surgeon, but also in the supplementation of vitamins and minerals, it is worth emphasizing that all cases should maintain long-term treatments booking appointments regularly, although cases of Brown Tumour are rare, the treatment was performed with total efficiency.


